胸主動(dòng)脈病變腔內(nèi)修復(fù)術(shù)合并“煙囪”支架置入術(shù)后內(nèi)漏情況分析
謝力民,王曉明,李曉召,閆瑞,楊鵬偉,閆繼鋒
?
臨床研究
胸主動(dòng)脈病變腔內(nèi)修復(fù)術(shù)合并“煙囪”支架置入術(shù)后內(nèi)漏情況分析
謝力民,王曉明,李曉召,閆瑞,楊鵬偉,閆繼鋒
目的:探討Standford B 型主動(dòng)脈病變?cè)诮隋^定區(qū)不足時(shí),置入覆膜支架行胸主動(dòng)脈腔內(nèi)修復(fù)術(shù)(TEVAR)合并“煙囪”支架處理受累的左頸總動(dòng)脈或左鎖骨下動(dòng)脈時(shí),術(shù)中發(fā)生內(nèi)漏的情況及其與病變位置之間的關(guān)系、手術(shù)療效及預(yù)后。
方法:回顧性分析2011-09至2015-07我院收治的Standford B 型主動(dòng)脈病變?cè)诮隋^定區(qū)不足的患者32例,采用置入覆膜支架行TEVAR合并“煙囪”支架治療,觀察術(shù)后即刻左頸總動(dòng)脈或左鎖骨下動(dòng)脈顯影、神經(jīng)系統(tǒng)并發(fā)癥及左上肢嚴(yán)重缺血癥狀、內(nèi)漏情況,并術(shù)后隨訪3~46個(gè)月神經(jīng)系統(tǒng)并發(fā)癥及左上肢嚴(yán)重缺血癥狀、內(nèi)漏情況。
結(jié)果:32例患者TEVAR合并“煙囪”支架均成功。術(shù)后即刻左頸總動(dòng)脈或左鎖骨下動(dòng)脈均顯影良好,患者均未出現(xiàn)神經(jīng)系統(tǒng)并發(fā)癥及左上肢嚴(yán)重缺血癥狀,主動(dòng)脈弓發(fā)生內(nèi)漏7例,其中病變位于主動(dòng)脈弓大彎側(cè)6例,病變位于主動(dòng)脈弓小彎側(cè)1例。術(shù)后隨訪3~46個(gè)月,主動(dòng)脈覆膜支架形態(tài)良好,“煙囪”支架內(nèi)血流通暢,7例發(fā)生內(nèi)漏患者中5例內(nèi)漏逐漸減小、消失,2例持續(xù)存在。
結(jié)論:Standford B 型胸主動(dòng)脈病變?cè)诮隋^定區(qū)不足時(shí),“煙囪”支架可延長(zhǎng)錨定區(qū)并保持左頸總動(dòng)脈或左鎖骨下動(dòng)脈通暢,更為安全地拓展了胸主動(dòng)脈病變腔內(nèi)治療的適應(yīng)證,達(dá)到微創(chuàng)、安全、有效的目的,但當(dāng)破口位于主動(dòng)脈弓大彎側(cè)時(shí),“煙囪”支架可能增加內(nèi)漏發(fā)生幾率。
主動(dòng)脈,胸;鎖骨下動(dòng)脈;頸總動(dòng)脈; “煙囪”支架
Abstract
Objective: To investigate thoracic endovascular aortic repair (TEVAR) and “Chimney” technique for treating the involved left common carotid artery (LCCA) or left subclavian artery (LSA) in Standford B patients with aortic lesion and in-sufficient proximal anchoring area. Meanwhile, to explore the relationship between endoleaking condition and the location of lesion with the prognosis.
Methods: A total of 32 relevant patients treated by TEVAR + “Chimney” technique in our hospital from 2011-09 to 2015-07 were retrospectively analyzed. Immediate post-operative image development of LCCA or LSA was observed; cerebral complications,severe upper limb ischemic symptoms and endoleaking conditions were recorded. The patients were followed-up for (3-46) months.
Results: Thoracic aortic stent-graft placement was successfully carried out in all 32 patients. Immediate post-operative image development of LCCA or LSA was favorable, no cerebral complications and no severe upper limb ischemic symptoms were observed. There were 7 patients suffered from endoleak at aortic arch including 6 with the lesion located at the greater curvature side and 1 at the small curvature side. During follow-up period, aortic stent-graft remained in a stable condition and the blood flow in “Chimney” stent was unobstructed. Endoleking condition was gradually reduced and disappeared in 5 patients, it was persisted in 2 patients.
Conclusion: “Chimney” technique may prolong anchoring area and keep LCCA or LSA unobstructed, therefore expand the indication of TEVAR in a mini-invasive, safe and effective way. When aortic lesion located at the greater curvature side, the endoleaking probability could be increased.
(Chinese Circulation Journal, 2016,31:692.)
近年來(lái),隨著胸主動(dòng)脈覆膜支架的改進(jìn)與支架的完善,經(jīng)股動(dòng)脈置入覆膜支架行胸主動(dòng)脈腔內(nèi)修復(fù)術(shù)(TEVAR)已經(jīng)成為Standford B 型主動(dòng)脈病變的首選治療方案[1-3]。但在TEVAR修復(fù)主動(dòng)脈弓部病變時(shí),由于病變鄰近左鎖骨下動(dòng)脈或位于左鎖骨下動(dòng)脈與左頸總動(dòng)脈之間,導(dǎo)致近端錨定區(qū)不足,往往會(huì)改用開放性手術(shù)或雜交手術(shù)治療,而高齡、肝腎功能差、整體耐受力差等高危患者可能因不能耐受外科手術(shù)而放棄TEVAR或外科治療。回顧性分析我院2011-09至2015-07采用TEVAR合并“煙囪”(Chimney)支架成功治療32例主動(dòng)脈弓部病變患者的療效,以及術(shù)中發(fā)生內(nèi)漏的情況及其與病變位置之間的關(guān)系。
1 資料與方法
一般資料:回顧性分析我院心血管內(nèi)科2011-09至2015-07 的Standford B 型主動(dòng)脈病變患者,從中篩選出近端錨定區(qū)不足(距左鎖骨下動(dòng)脈錨定區(qū)<15 mm)患者32例,男性25例(78.1%),年齡35~65歲,平均年齡(53.3±10.1)歲;32例患者病變類型包括: B型主動(dòng)脈病變夾層24例(75.0%),假性動(dòng)脈瘤3例(9.3%),穿透性潰瘍5例。病變位置包括:夾層破口位于主動(dòng)脈弓小彎側(cè)或側(cè)壁4例(12.5%),夾層破口位于主動(dòng)脈弓大彎側(cè)20例(62.5%),假性動(dòng)脈瘤位于主動(dòng)脈弓大彎側(cè)2例,假性動(dòng)脈瘤位于主動(dòng)脈弓小彎側(cè)或側(cè)壁1例,潰瘍破口位于主動(dòng)脈弓大彎側(cè)4例,潰瘍破口位于主動(dòng)脈弓小彎側(cè)或側(cè)壁1例。手術(shù)相關(guān)材料包括胸主動(dòng)脈覆膜支架系統(tǒng)(美國(guó),Medtronic公司生產(chǎn))、“Chimney”支架系統(tǒng)(美國(guó),Medtronic公司生產(chǎn))及各規(guī)格導(dǎo)絲、導(dǎo)管等。
影像學(xué)檢查:所有患者術(shù)前均行主動(dòng)脈全程計(jì)算機(jī)斷層掃描血管造影(CTA)檢查,以明確診斷,并確定裂口的位置及數(shù)目、血栓情況,病變累及的范圍及有無(wú)大分支受累,測(cè)量左側(cè)鎖骨下動(dòng)脈開口、夾層近端裂口、最大瘤體、肝臟頂部水平真假腔的直徑。
“Chimney”支架置入原因:29例患者( B型主動(dòng)脈病變夾層22例,假性動(dòng)脈瘤3例,穿透性潰瘍4例)病變開口位于左鎖骨下動(dòng)脈開口遠(yuǎn)側(cè),距左鎖骨下動(dòng)脈錨定區(qū)<15mm,行左鎖骨下動(dòng)脈內(nèi)“Chimney”支架置入;3例患者( B型主動(dòng)脈病變夾層2例,穿透性潰瘍1例)病變破口位于左鎖骨下動(dòng)脈與左頸總動(dòng)脈之間,為延長(zhǎng)主動(dòng)脈覆膜支架近側(cè)錨定區(qū),保障完全覆蓋主動(dòng)脈內(nèi)膜破口并增加支架置入后的穩(wěn)定性,行左頸總動(dòng)脈內(nèi)“Chimney”支架置入。
方法:患者均在局麻下進(jìn)行手術(shù),經(jīng)股動(dòng)脈切開途徑輸送主動(dòng)脈覆膜支架完成主動(dòng)脈病變腔內(nèi)隔絕術(shù),經(jīng)左肱動(dòng)脈置入“Chimney”支架至左鎖骨下動(dòng)脈或左頸總動(dòng)脈內(nèi)。手術(shù)關(guān)鍵步驟包括:(1)穿刺左側(cè)肱動(dòng)脈置入標(biāo)記豬尾導(dǎo)管。(2)標(biāo)準(zhǔn)全主動(dòng)脈造影,包括升主動(dòng)脈、降主動(dòng)脈、腹主動(dòng)脈和髂動(dòng)脈,明確主動(dòng)脈內(nèi)膜破口位置和夾層累及范圍,第一破口距左鎖骨下動(dòng)脈或左頸總動(dòng)脈距離,測(cè)量左鎖骨下動(dòng)脈開口部位主動(dòng)脈直徑,腹腔主要血管分支累及情況。(3)頭臂動(dòng)脈造影,在頭臂動(dòng)脈無(wú)病變情況下,觀察椎動(dòng)脈供血情況和Willis環(huán)是否完整并規(guī)劃手術(shù):右側(cè)椎動(dòng)脈供血良好,Willis環(huán)完整者,僅做主動(dòng)脈覆膜支架置入;右側(cè)椎動(dòng)脈供血差,或Willis環(huán)不完整者,先行TEVAR,再置入“Chimney”支架。(4)保留左肱動(dòng)脈豬尾導(dǎo)管在升主動(dòng)脈,切開暴露股動(dòng)脈,以Seldinger技術(shù)穿刺后置入豬尾導(dǎo)管至主動(dòng)脈真腔。切開股總動(dòng)脈,替換入加硬導(dǎo)絲。(5)切開一側(cè)股動(dòng)脈,阻斷后通過(guò)加硬導(dǎo)絲送入覆膜支架至左鎖骨下動(dòng)脈開口近側(cè)水平主動(dòng)脈弓部。(6)控制收縮壓水平于80~90 mmHg (1 mmHg=0.133 kPa),釋放主動(dòng)脈支架。(7)經(jīng)左肱動(dòng)脈置入長(zhǎng)度為5~6 cm,直徑為0.8 cm覆膜支架至保留三分之一支架在主動(dòng)脈弓內(nèi)。(8)左頸總動(dòng)脈置入“Chimney”支架患者,使用PLUG封堵器封閉左鎖骨下動(dòng)脈近端開口。(9)重復(fù)主動(dòng)脈造影,外科縫合股動(dòng)脈。觀察術(shù)后即刻左鎖骨下動(dòng)脈或左頸總動(dòng)脈顯影、神經(jīng)系統(tǒng)并發(fā)癥及左上肢嚴(yán)重缺血癥狀、內(nèi)漏情況,術(shù)后3個(gè)月、6個(gè)月、12個(gè)月隨訪患者并行CTA檢查,以后每年復(fù)查一次主動(dòng)脈及頸部、顱腦動(dòng)脈CTA檢查。
統(tǒng)計(jì)學(xué)方法:數(shù)據(jù)分析采用SPSSl7.0統(tǒng)計(jì)軟件。計(jì)數(shù)資料以例(率)表示,連續(xù)性變量采用獨(dú)立樣本t檢驗(yàn),不同病變部位的內(nèi)漏發(fā)生率比較采用Fisher精確檢驗(yàn)。P<0.05為差異有統(tǒng)計(jì)學(xué)意義。
2 結(jié)果
術(shù)中、術(shù)后即刻及圍手術(shù)期的結(jié)果: 32例患者均成功地行TEVAR合并“Chimney”支架,“Chimney”支架同時(shí)分別置入在 左鎖骨下動(dòng)脈 29例,左頸總動(dòng)脈 3例(圖1、2)。32例患者術(shù)中即刻造影發(fā)現(xiàn)I型近端內(nèi)漏7例(21.9%),無(wú)逆向撕裂累及升主動(dòng)脈;26例主動(dòng)脈大彎側(cè)病變的患者發(fā)生內(nèi)漏6例(23.1%,其中主動(dòng)脈夾層5例、假性動(dòng)脈瘤1例),6例主動(dòng)脈小彎側(cè)病變的患者發(fā)生內(nèi)漏1例(16.7%,為主動(dòng)脈夾層)。即刻內(nèi)漏發(fā)生率主動(dòng)脈大彎側(cè)病變較小彎側(cè)病變處高,差異有統(tǒng)計(jì)學(xué)意義(P=0.001)。術(shù)后即刻左鎖骨下動(dòng)脈或左頸總動(dòng)脈均顯影良好,術(shù)中及圍手術(shù)期均無(wú)死亡、神經(jīng)系統(tǒng)并發(fā)癥及左上肢嚴(yán)重缺血癥狀發(fā)生。
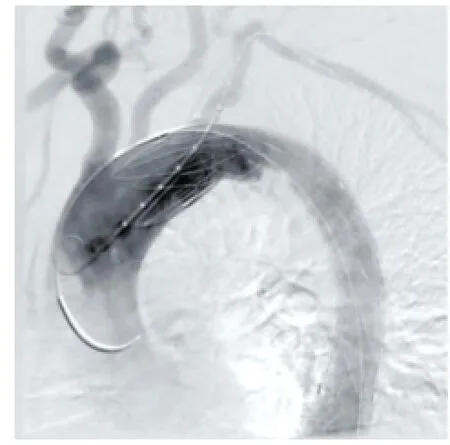
圖1 “煙囪”支架置入前

圖2 “煙囪”支架置入后
隨訪結(jié)果:術(shù)后隨訪3~46個(gè)月,主動(dòng)脈覆膜支架形態(tài)良好,“Chimney”支架內(nèi)血流通暢,5例內(nèi)漏逐漸減小、消失,2例持續(xù)存在但無(wú)明顯擴(kuò)大惡化,其中1例為小彎側(cè)主動(dòng)脈夾層合并主動(dòng)脈弓嚴(yán)重成角患者。
3 討論
Standford B 型主動(dòng)脈病變應(yīng)用TEVAR技術(shù)治療已被廣泛接受,并成為首選治療方案, TEVAR技術(shù)的關(guān)鍵在于有足夠的錨定區(qū),當(dāng)病變前錨定區(qū)不足時(shí),如果想追求覆膜支架釋放后的穩(wěn)定性和主動(dòng)脈夾層破口封堵的可靠性,則可能封閉左鎖骨下動(dòng)脈或左頸總動(dòng)脈,影響腦供血或左上肢供血。解剖結(jié)構(gòu)上,左鎖骨下動(dòng)脈發(fā)出的左側(cè)椎動(dòng)脈作為后腦一條供血血管且與右側(cè)椎動(dòng)脈匯合形成基底動(dòng)脈,而且通過(guò)Willis環(huán)與前腦的大腦中動(dòng)脈相溝通。以往研究[4-6]發(fā)現(xiàn)如果右側(cè)椎動(dòng)脈及雙側(cè)頸內(nèi)動(dòng)脈供血正常,覆膜支架完全封堵或不全封堵左鎖骨下動(dòng)脈,可以通過(guò)Willis環(huán)代償,不會(huì)出現(xiàn)嚴(yán)重腦缺血癥狀。故右側(cè)椎動(dòng)脈血流正常,則可同期完全封堵或不全封堵左鎖骨下動(dòng)脈開口;如果左側(cè)椎動(dòng)脈顯著優(yōu)勢(shì)型或Willis環(huán)本身不通暢的患者,就不能單純同期封堵左鎖骨下動(dòng)脈,必須重建左鎖骨下動(dòng)脈血流。既往對(duì)于主動(dòng)脈病變近端錨定區(qū)不足已有的技術(shù)包括頸—胸雜交、胸—胸雜交、“開窗”支架型血管、“豁口”支架型血管、分支支架型血管[7, 8]。“Chimney”支架是在TEVAR覆蓋主動(dòng)脈弓分支血管后經(jīng)被覆蓋血管遠(yuǎn)側(cè)端將血管內(nèi)支架放置在被覆蓋分支血管的開口及近段,突出部分與主動(dòng)脈覆膜大支架并列,從而恢復(fù)被覆蓋分支血管的血流[9, 10]。“Chimney”支架擴(kuò)展了TEVAR的錨定區(qū),改善了近端錨定區(qū)不足時(shí)TEVAR的療效又避免了“頸—胸雜交、胸—胸雜交”等手術(shù)痛苦,使更多不能耐受巨大血管外科創(chuàng)傷手術(shù)的患者有機(jī)會(huì)接受微創(chuàng)治療[11]。本組病例分析結(jié)果發(fā)現(xiàn)在TEVAR+Chimney術(shù)中內(nèi)漏的發(fā)生率與病變的位置有關(guān)。
有研究結(jié)果顯示,內(nèi)漏是主動(dòng)脈夾層腔內(nèi)隔絕術(shù)后的主要并發(fā)癥,其發(fā)生率為0~38.2%[12-14]。內(nèi)漏是指主動(dòng)脈覆膜支架置入后假腔未被徹底隔絕,仍有血液流入假腔。根據(jù)內(nèi)漏來(lái)源分為四型:I型指近端內(nèi)漏;Ⅱ型指遠(yuǎn)端內(nèi)漏,包括來(lái)源于覆膜支架遠(yuǎn)端與管壁之間的縫隙、遠(yuǎn)端裂口的反流和動(dòng)脈分支的反流;Ⅲ型指與覆膜支架毀損或破裂、針孔有關(guān)的內(nèi)漏;Ⅳ型內(nèi)漏指覆膜支架密封性能較差,形成廣泛滲漏。內(nèi)漏按發(fā)生時(shí)問(wèn)可分為:即時(shí)內(nèi)漏和遲發(fā)性內(nèi)漏。根據(jù)內(nèi)漏血流量的大小可分為大量、中量、少量、微量?jī)?nèi)漏[15]。在TEVAR+Chimney技術(shù)中絕大部分內(nèi)漏是I型內(nèi)漏[16, 17]。
Chimney支架本身不會(huì)影響主動(dòng)脈覆膜支架的穩(wěn)定性,但從本組病例分析結(jié)果發(fā)現(xiàn)如果是破口和假腔位于大彎側(cè)的夾層動(dòng)脈瘤或梭形膨大的假性動(dòng)脈瘤,則術(shù)中即刻發(fā)生內(nèi)漏的幾率較大(大彎側(cè)病變內(nèi)漏發(fā)生率23.1% vs 小彎側(cè)病變內(nèi)漏發(fā)生率16.7%,P=0.001),主要原因可能為Chimney支架突入主動(dòng)脈部分與主動(dòng)脈覆膜支架并列,使主動(dòng)脈覆膜支架與主動(dòng)脈壁大彎側(cè)貼附緊密度受影響,但卻增加了主動(dòng)脈覆膜支架與主動(dòng)脈壁小彎側(cè)的貼附緊密度,出現(xiàn)內(nèi)漏后(尤其是大彎側(cè)),予以主動(dòng)脈支架后擴(kuò)張則可改善支架與主動(dòng)脈壁的貼附緊密度,可改善內(nèi)漏情況。另外小口徑Chimney支架置入也能減少內(nèi)漏的發(fā)生。
綜上所述,本研究證實(shí)在近端錨定區(qū)不足的Standford B 型主動(dòng)脈病變應(yīng)用TEVAR+Chimney技術(shù)是一種安全有效保留重要分支血管維持重要器官血供的方法,但當(dāng)主動(dòng)脈病變位于大彎側(cè)時(shí),術(shù)中出現(xiàn)內(nèi)漏的幾率增加,提示術(shù)前需充分評(píng)估病變位置,估計(jì)術(shù)中、術(shù)后并發(fā)癥,周密設(shè)計(jì)手術(shù)方案,術(shù)后密切隨訪觀察。同時(shí)本研究因例數(shù)較少,諸多問(wèn)題仍需長(zhǎng)期密切觀察和更大樣本的研究。
[1] Eggebrecht H, Nienaber CA, Neuhauser M, et al. Endovascular stentgraft placement in aortic dissection: a meta-analysis. Eur Heart J,2006, 27: 489-498.
[2] 明廣華, 張宇輝, 吳海英, 等. 179例主動(dòng)脈夾層患者的臨床資料分析. 中國(guó)循環(huán)雜志, 2004, 05: 45-48.
[3] 郭偉, 蓋魯粵, 劉小平, 等. 主動(dòng)脈夾層腔內(nèi)修復(fù)術(shù)178例術(shù)后早期療效分析. 中華外科雜志, 2005, 43: 921-925.
[4] 董智慧, 符偉國(guó), 王玉琦, 等. 胸主動(dòng)脈腔內(nèi)修復(fù)擴(kuò)展近端錨定區(qū)的探討. 中華外科雜志, 2005, 43: 857-860.
[5] 趙珺, 辛軍. 開窗型覆膜支架腔內(nèi)修復(fù)術(shù)聯(lián)合頸-頸動(dòng)脈搭橋術(shù)治療主動(dòng)脈弓部動(dòng)脈瘤. 外科理論與實(shí)踐, 2011, 16: 140-142.
[6] Kotelis D, Geisbüsch P, Hinz U, et al.Short and midterm results after left subclavian artery coverage during endovascular repair of the thoracic aorta. J Vasc Surg, 2009, 50:1285-1292.
[7] Ohrlander T, Sonesaon B, Ivancev K, et al.The chimney graft: a technique for preserving or rescuing aortic branch vessels in stentgraft sealing zones. Endovasc Ther, 2008, 15: 427-432.
[8] Criado FJ. Following the curve in TEVAR: adapting stent-grafts to the aortic arch. J Endovase Ther, 2008, 15: 67-71.
[9] Sonesson B, Reseh T, Allers M, et al.Endovascular total aortic arch replacement by in situ stent Faft fenestration technique.J Vasc Surg,2009, 49: 1589-1591.
[10] 郭偉,劉小平,尹太,等.主動(dòng)脈弓部病變腔內(nèi)修復(fù)術(shù)的研究.中國(guó)實(shí)用外科雜志,2007,27:136-138.
[11] 易定華, 段維勛. 中國(guó)主動(dòng)脈夾層診療現(xiàn)狀與展望. 中國(guó)循環(huán)雜志,2013, 01: 1-2.
[12] Nienaber CA, Fattofi R, Lund G, et al.Nonsurgiud reconstruction of thoracic aortic dissection by stent—graft placement.N Eng J Med,1999, 340: 15-39.
[13] Lee WA, Wolf YG, Fogarty TJ, et al. Does complete aneurysm exclusion ensure long-term success after endovascular repair?. Endovasc Ther, 2000, 7: 494-500.
[14] Krajcer Z, Dougherty KG, Gregoric ID.Long-term results of aortic banding for complex infrarenal neck anatomy and type I endoleak after endovascular abdominal aortic aneurysm repair. Tex Heart Inst J,2012, 39: 799-805.
[15] Schurinlc GWH, Aarts NJM, van Baalen JM, et a1.Stent attachment site--related endoleakage after stent graft treatment.an in vitro study of then effects of graft size, slant type, and atherosclerotic wall changes. Vase Surg, 1999, 30: 658-667.
[16] Fukui D, Wada Y, Komatsu K,et al. Innovative application of available stent grafts in Japan in aortic aneurysm treatment-significance of innovative debranching and chimney method and coil embolization procedure. Ann Vasc Dis, 2013, 6:601-611.
[17] Moulakakis KG, Mylonas SN, Dalainas I, et al. The chimney-graft technique for preserving supra-aortic branches: a review. Ann Cardiothorac Surg, 2013, 2: 339-346.
(編輯:曹洪紅)
Analysis on Thoracic Endovascular Aortic Repair and Endoleak of “Chimney” Technique for Treating the Patients With Thoracic Aortic Lesions
XIE Li-min, WANG Xiao-ming, LI Xiao-zhao, YAN Rui, YANG Peng-wei, YAN Ji-feng.
Department of Cardiology, Chest Hospital of Henan Province, Zhengzhou (450003), Henan, China
Corresponding Author: XIE Li-min, Email: xlm761229@126.com
Aorta, thoracic; Subclavian artery; Common carotid artery; Stent implantation; “Chimney” technique
450000 鄭州市,河南省胸科醫(yī)院 心血管六病區(qū)
謝力民 主治醫(yī)師 碩士研究生 主要從事心血管疾病的介入診療研究 Email: xlm761229@126.com 通訊作者:謝力民
R541
A
1000-3614(2016)07-0692-04
10.3969/j.issn.1000-3614.2016. 07.017
( 2015-10-22)
- 中國(guó)循環(huán)雜志的其它文章
- 原花青素對(duì)缺血再灌注大鼠心肌細(xì)胞凋亡及凋亡相關(guān)基因蛋白表達(dá)的影響
- 黃芩苷對(duì)再灌注心肌細(xì)胞保護(hù)作用及與心肌細(xì)胞自噬的相關(guān)性
- 經(jīng)導(dǎo)管主動(dòng)脈瓣置換術(shù)的進(jìn)展與未來(lái)
- 經(jīng)皮肺動(dòng)脈瓣植入術(shù)后患者心功能的變化8例分析
- 徒手心肺復(fù)蘇與心肺復(fù)蘇機(jī)在急診科應(yīng)用的療效比較
- 肝功能Child-Turcotte-Pugh評(píng)分在住院心力衰竭患者風(fēng)險(xiǎn)評(píng)估中的應(yīng)用

