不同超聲檢查對直腸乙狀結腸深部浸潤型子宮內膜異位癥診斷價值的Meta分析
牛 旺,史鐵梅,張原溪,宗 璨,周 錚,劉 晨
(中國醫科大學附屬盛京醫院超聲科,遼寧 沈陽 110004)
不同超聲檢查對直腸乙狀結腸深部浸潤型子宮內膜異位癥診斷價值的Meta分析
牛 旺,史鐵梅*,張原溪,宗 璨,周 錚,劉 晨
(中國醫科大學附屬盛京醫院超聲科,遼寧 沈陽 110004)
目的 采用Meta分析評價經陰道增強超聲(E-TVS)、經陰道超聲(TVS)、經直腸超聲(TRS)對直腸乙狀結腸深部浸潤型子宮內膜異位癥的診斷價值。方法 檢索1990年1月—2016年6月關于E-TVS、TVS、TRS診斷直腸乙狀結腸深部浸潤型子宮內膜異位癥(DIE)的中英文文獻,提取納入研究的信息,采用Meta-disc 1.4軟件對研究數據進行統計學分析。結果 共納入25篇英文文獻。E-TVS的敏感度、特異度、陽性似然比、陰性似然比、診斷性比值比分別為0.92、0.96、16.64、0.09、227.95;TVS為0.83、0.97、16.95、0.17、112.97;TRS為0.94、0.96、14.43、0.08、208.72。3組SROC曲線下面積分別為0.980 4、0.966 3、0.979 0。結論 3種超聲檢查方法對直腸乙狀結腸DIE的診斷價值由高至低依次為E-TVS、TRS、TVS。E-TVS可作為超聲診斷直腸乙狀結腸DIE的首選方法。
子宮內膜異位癥;直腸;結腸,乙狀;超聲檢查,經陰道;超聲檢查,經直腸;Meta分析
深部浸潤型子宮內膜異位癥(deep infiltration endometriosis, DIE)是子宮內膜異位癥的一種特殊類型,是指任何子宮內膜異位癥病灶在腹膜下浸潤深度超過5 mm。DIE累及部位按發病率依次為宮骶韌帶、直腸乙狀結腸、陰道、膀胱,其中直腸乙狀結腸發病率為4%~37%,是除生殖系統外發病率最高部位[1]。目前不同超聲檢查方法對其診斷價值并無一致結論。
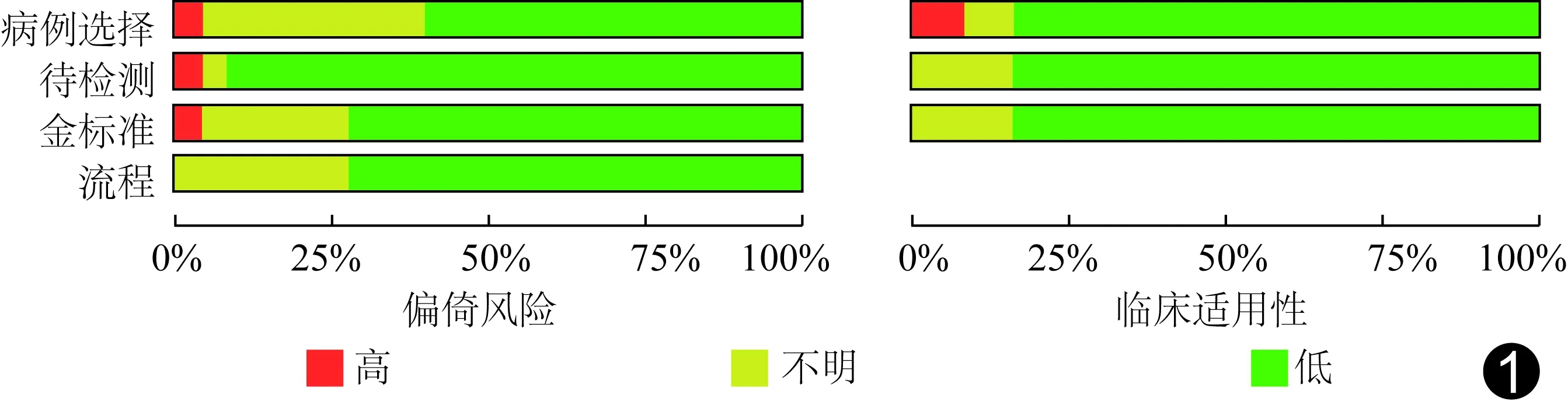
圖1 25篇納入研究的文獻質量評價(QUADAS-2)
本研究旨在采用Meta分析方法評價經陰道增強超聲(enhanced transvaginal ultrasound, E-TVS)、經陰道超聲(transvaginal ultrasound, TVS)、經直腸超聲(transrectal ultrasound, TRS)對直腸乙狀結腸DIE的診斷價值。
1 資料與方法
1.1 文獻檢索 檢索中文數據庫CNKI、萬方和維普數據庫,英文數據庫Pubmed、EMBASE和Cochrane library,文獻發表時間為1990年1月—2016年6月。中文檢索詞為:子宮內膜異位癥、深部浸潤型子宮內膜異位癥、深部內異癥、直腸、乙狀結腸、腸道、超聲、經陰道超聲、經直腸超聲;英文檢索詞為endometriosis、infiltration、infiltrating、transvaginal、transrectal、ultrasound、sonography、bowel、intestine、intestinal、rectosigmoid、rectal、endorectal、colonsigmoideum。
1.2 納入標準 ①研究對象:可疑DIE患者;②研究設計:前瞻性研究;③檢查方式:E-TVS、TVS、TRS;④金標準:腹腔鏡或切除標本經組織病理學檢查確診為直腸乙狀結腸DIE;⑤可直接或間接獲得四格表數據;⑥語種:中文、英文;⑦樣本含量≥15例。
1.3 排除標準 ①研究設計:回顧性研究;②無腹腔鏡或組織病理學檢查結果;③無法獲得四格表數據;④語種:非中文、英文;⑤樣本含量<15例;⑥綜述、個案報道、會議論文、經驗交流、文摘;⑦動物實驗等基礎研究;⑧重復發表的文獻。
1.4 質量評價 采用診斷試驗準確性質量評價工具-2(quality assessment of diagnostic accuracy studies 2, QUADAS-2),從病例選擇、待評價試驗、金標準、病例流程和進展情況對文獻的偏倚風險和臨床適用性進行評價。
1.5 文獻篩選及質量評價 由2名研究者獨立完成后匯總,有爭議時協商,必要時與第3名專家協商。
1.6 統計學分析 提取并匯總各文獻四格表數據,采用Meta-disc 1.4軟件進行異質性分析:計算敏感度(sensitivity, Se)對數與[1-特異度(specificity, Sp)]對數的Spearman相關系數檢測閾值效應引起的異質性;采用Q檢驗、χ2檢驗及I2檢驗檢測非閾值效應引起的異質性。采用隨機效應模型合并Se、Sp、陽性似然比(positive likelihood ratio, LR+)、陰性似然比(negative likelihood ratio, LR-)、診斷性試驗比值比(diagnostic odds ratio, DOR),繪制綜合受試者工作特征 (summary receiver operator characteristic curve, SROC)曲線。對3種檢查方法的合并Se與合并Sp分別進行χ2檢驗、I2檢驗。P<0.05為差異有統計學意義。
2 結果
初步檢索獲得英文文獻582篇,中文文獻354篇。最終25篇[2-26]文獻符合納入標準,均為英文文獻。其中采用E-TVS文獻8篇[2-6,14-15,21],TVS文獻10篇[7-9,11-13,18-19,22,24],TRS文獻3篇[23,25-26],同時涉及E-TVS和TVS文獻2篇[10,20],E-TVS和TRS文獻1篇[16],TVS和TRS文獻1篇[17]。25篇文獻的基本特征見表1。
2.1 文獻質量評價 偏倚風險:病例選擇偏倚風險主要源于未強調納入患者是否連續,有9篇文獻[3,7,10-11,14,20,24-26];待檢測部分偏倚風險,除文獻[7,25]外,均為低風險;金標準偏倚風險主要源于未明確金標準結果的判讀是否在不知道檢測結果的情況下進行,有6篇文獻[2-4,16,25-26],5篇文獻[4-5,8-9,21]采用的金標準是腹腔鏡,而不是病理;病例流程偏倚風險主要源于未明確指出待檢測試驗與金標準的判讀間是否有合適的間期,有7篇文獻[5-7,12,17-18,23]。
臨床適用性:病例選擇方面除文獻[18,25]外,余文獻的病例具有較好的適用;待檢測部分和金標準部分的適用性良好。其中有1篇文獻[25]的質量較差,主要因選擇的病例不符合入組的標準,見圖1。
2.2 統計分析結果
2.2.1 異質性分析 閾值效應:E-TVS、TVS、TRS的Se對數與(1-Sp)對數的Spearman相關系數分別為-0.17(P=0.61)、-0.26(P=0.39)、-0.20(P=0.75),差異均無統計學意義。SROC曲線圖呈不典型“肩臂狀”分布(圖2~4)。3種檢查方法均不存在閾值效應引起的異質性,故分別合并各統計指標。
非閾值效應:經Q檢驗,P均<0.10。除TRS的合并Se(χ2=4.57,P=0.333 8)與合并Sp(χ2=8.88,P=0.064 1)差異無統計學意義外,余差異均有統計學意義(P均<0.05);除TRS的合并Se的I2=12.60%(<50%)外,余I2均>50%。3種檢查方法均存在非閾值效應引起的異質性,故合并統計指標時均采用隨機效應模型。
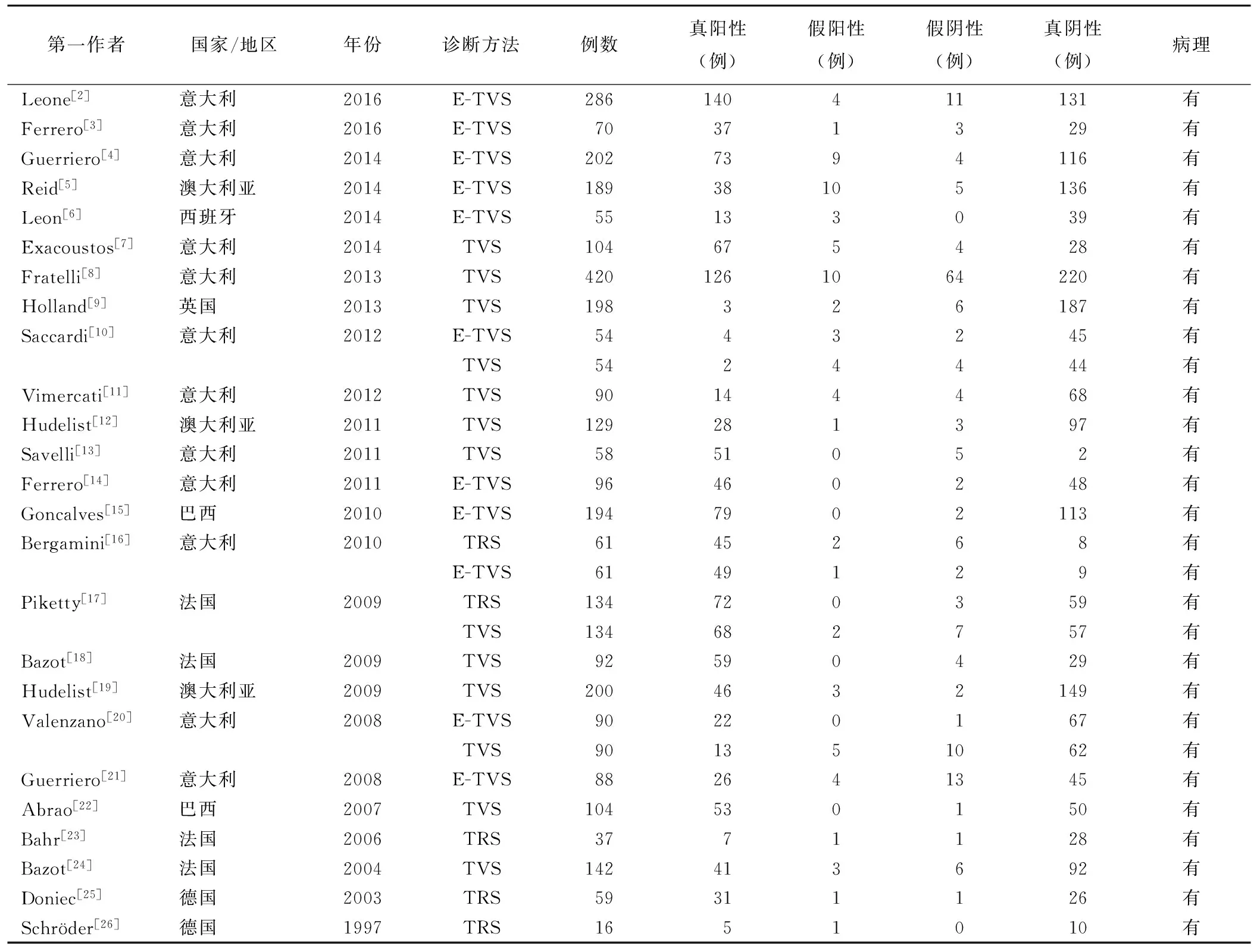
表1 25篇納入研究的文獻資料
2.2.2合并評價指標 采用隨機效應模型獲得E-TVS、TVS、TRS的Se、Sp、LR+、LR-、DOR見表2;SROC曲線下面積分別為0.980 4[95%CI(0.973 0,0.987 8),圖2]、0.966 3[95%CI(0.955 2,0.974 4),圖3]、0.979 0[95%CI(0.964 4,0.993 6),圖4]。
3 討論
直腸乙狀結腸DIE超聲表現為位于肌層內或累及肌層的形態不規則低回聲結節,可導致肌層收縮和粘連,常致慢性盆腔疼痛[27]。對DIE治療前診斷評估有利于選擇合理的治療方案和合適的手術方式,有效控制疾病進展。目前,診斷DIE的金標準是組織病理學檢查,其次為腹腔鏡[4],但均屬有創性檢查。非創傷性檢查包括超聲和MRI等,但Medeiros等[28]進行Meta分析表明,MRI診斷直腸乙狀結腸DIE的Se為0.84,Sp為0.97。隨著超聲技術發展,超聲診斷DIE的前瞻性研究增多,Guerriero等[29]的研究結果表明TVS的Se為0.89,Sp為0.97;E-TVS的Se為0.93,Sp為0.97,較MRI略有優勢。
目前超聲檢查包括TVS、E-TVS、TRS及直腸內鏡超聲(rectalendoscopic ultrasonography, EUS)等。TVS作為子宮附件區的常規檢查手段[30],診斷盆腔DIE有較高的效能和較好的觀察者間一致性。E-TVS是用水、生理鹽水或凝膠,在陰道或直腸中人為制造透聲窗,提高對DIE的診斷能力[2]。TRS也可清晰顯示腸道DIE病灶部位、大小、腸壁浸潤深度等。
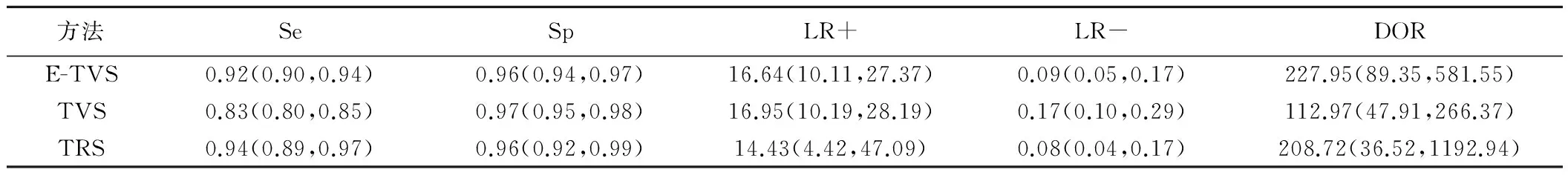
表2 3種超聲診斷方法的各指標比較(95%CI)
圖2 E-TVS的SROC曲線圖 圖3 TVS的SROC曲線圖 圖4 TRS的SROC曲線圖
診斷準確性是評價診斷價值的重要方面。在檢測指標Se、Sp、LR+、LR-、DOR和SROC曲線下面積中,LR+和LR-較Se和Sp更穩定,LR+越大,LR-越小,診斷準確率越高,DOR=LR+/LR-,DOR值越大,診斷準確性越高。雖然LR+、LR-、DOR綜合應用了真陽性率、假陽性率的信息,但均與診斷界點的選取有關。SROC曲線下面積排除了診斷界值的影響,可更好地反映診斷效能,SROC曲線下面積越大,診斷準確性越高。因此,在本研究中,綜合SROC曲線下面積和DOR,E-TVS對直腸乙狀結腸DIE的診斷價值略高于TRS和TVS,TVS的診斷價值最低。由于TRS檢查過程中探頭與直腸壁直接接觸,透聲好,對直腸乙狀結腸肌層的顯示率好,圖像質量高,因而提高了對直腸病變的檢測價值。而E-TVS人為制造了良好的透聲窗,也可較好地顯示直腸乙狀結腸DIE病灶;經直腸灌注制造透聲窗時,可造成直腸的蠕動,有利于發現病灶;E-TVS縱向掃查范圍大,可檢測到離肛門較遠的受累腸壁[16]。TVS診斷價值較低的主要原因為透聲性差,超聲圖像的分辨率低。另外,目前針對直腸乙狀結腸DIE患者TRS檢查的相關準備工作的研究較少,如檢查前表面麻醉、腸道準備、直腸指檢,尚未形成程序性參考標準。檢查過程中部分患者不能耐受,使TRS檢查在臨床應用有所減少。另因TRS普及率較低,其對疾病的觀察者間一致性及同一觀察者的可重復性還需探討。由于E-TVS在臨床的接受程度高,診斷價值也略高于TRS,因此,推薦將E-TVS作為超聲診斷直腸乙狀結腸DIE的首選方法。
本研究結果表明3種超聲檢查均存在非閾值效應引起的異質性,可能來源于:①醫師的操作技能及經驗差異;②病例來源于多個國家,存在人種、地域和醫療水平的差異;③增強技術、檢查設備及探頭型號存在差別。④所有的研究中,外科醫師不可能忽視影像學報告,導致了固有的異質性。
本研究局限性:①文獻檢索時未檢索會議記錄、未發表文獻等導致的發表偏倚;②文獻的語種僅限于中、英文,可能存在語種偏倚。
綜上所述,本研究結果表明,3種超聲檢查對直腸乙狀結腸DIE的診斷價值依次為E-TVS、TRS、TVS。推薦E-TVS可作為超聲診斷直腸乙狀結腸DIE的首選方法。
[1] Nisenblat V, Bossuyt PM, Farquhar C, et al. Imaging modalities for the non-invasive diagnosis of endometriosis. Cochrane Database Syst Rev, 2016,2:CD009591.
[2] Leone Roberti Maggiore U, Biscaldi E, Vellone GV, et al. Magnetic resonance enema vs rectal water-contrast transvaginal sonography in diagnosis of rectosigmoid endometriosis. Ultrasound Obstet Gynecol, 2017,49(4):524-532.
[3] Ferrero S, Biscaldi E, Vellone VG, et al. Computed tomographic colonography vs rectal-water contrast transvaginal ultrasonography in diagnosis of rectosigmoid endometriosis: A pilot study. Ultrasound Obstet Gynecol, 2017,49(4):515-523.
[4] Guerriero S, Saba L, Ajossa S, et al. Three-dimensional ultrasonography in the diagnosis of deep endometriosis. Hum Reprod, 2014,29(6):1189-1198.
[5] Reid S, Lu C, Hardy N, et al. Office gel sonovaginography for the prediction of posterior deep infiltrating endometriosis: A multicenter prospective observational study. Ultrasound Obstet Gynecol, 2014,44(6):710-718.
[6] Leon M, Vaccaro H, Alcazar JL, et al. Extended transvaginal sonography in deep infiltrating endometriosis: Use of bowel preparation and an acoustic window with intravaginal gel: Preliminary results. J Ultrasound Med, 2014,33(2):315-321.
[7] Exacoustos C, Malzoni M, Di Giovanni A, et al. Ultrasound mapping system for the surgical management of deep infiltrating endometriosis. Fertil Steril, 2014,102(1):143-150.
[8] Fratelli N, Scioscia M, Bassi E, et al. Transvaginal sonography for preoperative assessment of deep endometriosis. J Clin Ultrasound, 2013,41(2):69-75.
[9] Holland TK, Cutner A, Saridogan E, et al. Ultrasound mapping of pelvic endometriosis: Does the location and number of lesions affect the diagnostic accuracy? A multicentre diagnostic accuracy study. BMC Womens Health, 2013,13:43.
[10] Saccardi C, Cosmi E, Borghero A, et al. Comparison between transvaginal sonography, saline contrast sonovaginography and magnetic resonance imaging in the diagnosis of posterior deep infiltrating endometriosis. Ultrasound Obstet Gynecol, 2012,40(4):464-469.
[11] Vimercati A, Achilarre MT, Scardapane A, et al. Accuracy of transvaginal sonography and contrast-enhanced magnetic resonance-colonography for the presurgical staging of deep infiltrating endometriosis. Ultrasound Obstet Gynecol, 2012,40(5):592-603.
[12] Hudelist G, Ballard K, English J, et al. Transvaginal sonography vs. clinical examination in the preoperative diagnosis of deep infiltrating endometriosis. Ultrasound Obstet Gynecol, 2011,37(4):480-487.
[13] Savelli L, Manuzzi L, Coe M, et al. Comparison of transvaginal sonography and double-contrast barium enema for diagnosing deep infiltrating endometriosis of the posterior compartment. Ultrasound Obstet Gynecol, 2011,38(4):466-471.
[14] Ferrero S, Biscaldi E, Morotti M, et al. Multidetector computerized tomography enteroclysis vs.rectal water contrast transvaginal ultrasonography in determining the presence and extent of bowel endometriosis. Ultrasound Obstet Gynecol, 2011,37(5):603-613.
[15] Goncalves MO, Podgaec S, Dias JA Jr, et al. Transvaginal ultrasonography with bowel preparation is able to predict the number of lesions and rectosigmoid layers affected in cases of deep endometriosis, defining surgical strategy. Hum Reprod, 2010,25(3):665-671.
[16] Bergamini V, Ghezzi F, Scarperi S, et al. Preoperative assessment of intestinal endometriosis: A comparison of transvaginal sonography with water-contrast in the rectum, transrectal sonography, and barium enema. Abdom Imaging, 2010,35(6):732-736.
[17] Piketty M, Chopin N, Dousset B, et al. Preoperative work-up for patients with deeply infiltrating endometriosis: Transvaginal ultrasonography must definitely be the first-line imaging examination. Hum Reprod, 2009,24(3):602-607.
[18] Bazot M, Lafont C, Rouzier R, et al. Diagnostic accuracy of physical examination, transvaginal sonography, rectal endoscopic sonography, and magnetic resonance imaging to diagnose deep infiltrating endometriosis. Fertil Steril, 2009,92(6):1825-1833.
[19] Hudelist G, Tuttlies F, Rauter G, et al. Can transvaginal sonography predict infiltration depth in patients with deep infiltrating endometriosis of the rectum? Hum Reprod, 2009,24(5):1012-1017.
[20] Valenzano Menada M, Remorgida V, Abbamonte LH, et al. Does transvaginal ultrasonography combined with water-contrast in the rectum aid in the diagnosis of rectovaginal endometriosis infiltrating the bowel? Hum Reprod, 2008,23(5):1069-1075.
[21] Guerriero S, Ajossa S, Gerada M, et al. Diagnostic value of transvaginal 'tendernessguided' ultrasonography for the prediction of location of deep endometriosis. Hum Reprod, 2008, 23(11):2452-2457.
[22] Abrao MS, Goncalves MO, Dias JA Jr, et al. Comparison between clinical examination, transvaginal sonography and magnetic resonance imaging for the diagnosis of deep endometriosis. Hum Reprod, 2007,22(12):3092-3097.
[23] Bahr A, de Parades V, Gadonneix P, et al. Endorectal ultrasonography in predicting rectal wall infiltration in patients with deep pelvic endometriosis: A modern tool for an ancient disease. Dis Colon Rectum, 2006,49(6):869-875.
[24] Bazot M, Thomassin I, Hourani R, et al. Diagnostic accuracy of transvaginal sonography for deep pelvic endometriosis. Ultrasound Obstet Gynecol, 2004,24(2):180-185.
[25] Doniec JM, Kahlke V, Peetz F, et al. Rectal endometriosis: High sensitivity and specificity of endorectal ultrasound with an impact for the operative management. Dis Colon Rectum, 2003,46(12):1667-1673.
[26] Schr?der J, Lohnert M, Doniec JM, et al. Endoluminal ultrasound diagnosis and operative management of rectal endometriosis. Dis Colon Rectum, 1997,40(5):614-617.
[27] Xia WT, Cai YY, Yang SM, et al. Prevalence of endometriosis during abdominal or laparoscopic hysterectomy for chronic pelvic pain. Obstet Gynecol, 2016,128(3):658.
[28] Medeiros LR, Rosa MI, Silva BR, et al. Accuracy of magnetic resonance in deeply infiltrating endometriosis: A systematic review and meta-analysis. Arch Gynecol Obstet, 2015,291(3):611-621.
[29] Guerriero S, Ajossa S, Orozco R, et al. Accuracy of transvaginal ultrasound for diagnosis of deep endometriosis in the rectosigmoid: Systematic review and meta-analysis. Ultrasound Obstet Gynecol, 2016,47(3):281-289.
[30] 梁星新,王保鋼,馬鋼,等.經陰道超聲診斷早期異位妊娠的影響因素.中國醫學影像技術,2015,31(1):98-100.
Ultrasound value in diagnosis of deep infiltrating endometriosis in rectosigmoid: Meta-analysis
NIUWang,SHITiemei*,ZHANGYuanxi,ZONGCan,ZHOUZheng,LIUChen
(DepartmentofUltrasound,ShengjingHospitalofChinaMedicalUniversity,Shenyang110004,China)
Objective To explore the diagnostic value of comparing enhanced transvaginal ultrasound (E-TVS), none enhanced transvaginal ultrasound (TVS), and transrectal ultrasound (TRS) in preoperative detection of deep infiltrating endometriosis (DIE) in the rectosigmoid by Meta-analysis. Methods The literatures published from January 1990 to June 2016 were searched. The information of literatures were selected and evaluated. The included data was statistically analyzed by Meta-disc 1.4 software. Results Totally 25 literatures were enrolled. The pooled sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, diagnostic odds ratio were 0.92, 0.96, 16.64, 0.09, 227.95 for E-TVS, 0.83, 0.97, 16.95, 0.17, 112.97 for TVS, 0.94, 0.96, 14.43, 0.08, 208.72 for TRS, respectively. Area under the curve were 0.980 4, 0.966 3, 0.979 0, respectively. Conclusion Diagnostic value of the three ultrasonography in preoperative detection of DIE in the rectosigmoid are E-TVS, TRS, TVS. E-TVS can be used as the preferred method of ultrasonic diagnosis of DIE in the rectosigmoid.
Endometriosis; Rectum; Colon, sigmoid; Ultrasonography, transvaginal; Ultrasonography, transrectal; Meta-analysis
牛旺(1991—),女,黑龍江大慶人,在讀碩士。研究方向:婦科超聲診斷。E-mail: 251291417@qq.com
史鐵梅,中國醫科大學附屬盛京醫院超聲科,110004。
E-mail: shitm@sj-hospital.org
2016-10-24
2017-01-18
R711.71; R445.1
A
1003-3289(2017)06-0912-05
10.13929/j.1003-3289.201610107