移動醫療用于孕產婦健康管理的效果研究
景聯紅 肖文霞 肖玲
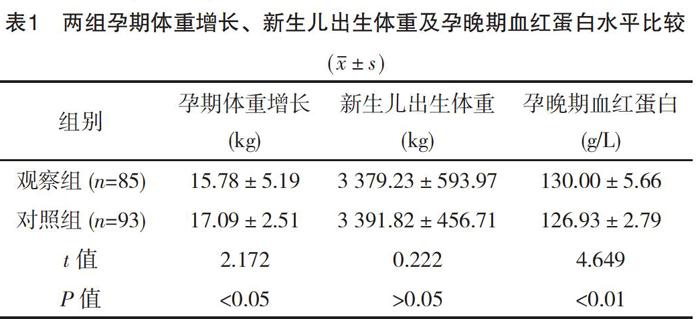
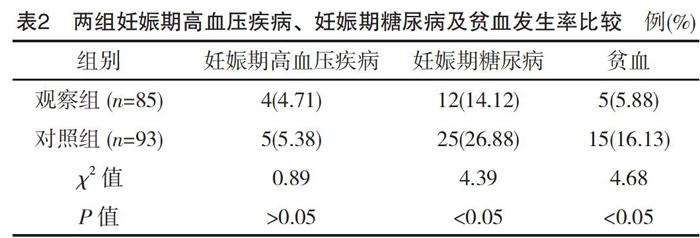
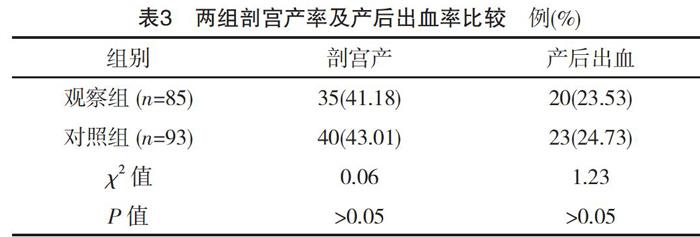
【摘要】 目的:探討移動醫療對于孕產婦健康管理的效果,為推行移動醫療提供理論依據。方法:采用前瞻性研究方法,選取2017年10月1日-12月31日在筆者所在醫院門診建檔的230例孕婦為研究對象。將研究對象隨機分為兩組,每組115例。對照組采用常規規律產檢+筆者所在醫院正常安排的孕婦學校課程;觀察組采用常規規律產檢+筆者所在醫院正常安排的孕婦學校課程+微信群結合幸運媽咪APP進行移動醫療干預。觀察并比較兩組孕婦孕期體重增長、新生兒出生體重及孕晚期血紅蛋白水平,妊娠期高血壓疾病、妊娠期糖尿病及貧血發生率,剖宮產率及產后出血率。結果:(1)觀察組孕期體重增長明顯少于對照組,差異有統計學意義(P<0.05);兩組新生兒出生體重比較,差異無統計學意義(P>0.05);觀察組孕晚期血紅蛋白水平明顯高于對照組,差異有統計學意義(P<0.01)。(2)兩組妊娠期高血壓疾病發生率比較,差異無統計學意義(P>0.05);觀察組妊娠期糖尿病及貧血的發生率均明顯低于對照組,差異有統計學意義(P<0.05)。(3)兩組剖宮產率及產后出血率比較,差異均無統計學意義(P>0.05)。結論:移動醫療是一種健康教育方式,能減少孕期體重增長,降低妊娠期糖尿病和貧血的發生率,對于新生兒體重、分娩方式及產后出血無明顯影響。
【關鍵詞】 移動醫療; 健康管理; 效果
doi:10.14033/j.cnki.cfmr.2019.25.068 文獻標識碼 B 文章編號 1674-6805(2019)25-0-03
Effect of Mobile Health on Maternal Health Management/JING Lianhong,XIAO Wenxia,XIAO Ling.//Chinese and Foreign Medical Research,2019,17(25):-162
【Abstract】 Objective:To explore the effect of mobile health on maternal health management and to provide theory evidence for the implementation of mobile health.Method:A total of 230 pregnant women who were documented in the outpatient department of our hospital from October 1st to December 31st 2017 were selected as the research object by prospective study.They were randomly divided into two groups,with 115 cases in each group.The control group was treated by routine regular obstetric examination and normal school courses for pregnant women arranged by our hospital.The observation group was treated by routine regular obstetric examination,and normal school courses for pregnant women arranged by our hospital,and wechat group with lucky mummy APP for mobile health.The pregnancy weight gain,neonatal birth weight,hemoglobin level in the third trimester,incidence of hypertensive disorder of pregnancy and gestational diabetes mellitus and anemia,cesarean section rate and postpartum hemorrhage rate were observed and compared between the two groups.Result:(1)The pregnancy weight gain in the observation group was significantly less than that in the control group,the difference was statistically significant(P<0.05).There was no significant difference in neonatal birth weight between two groups(P>0.05).The level of hemoglobin in the third trimester of observation group was significantly higher than that of the control group,the difference was statistically significant(P<0.01).(2)The incidence of hypertensive disorder of pregnancy between the two groups was not statistically significant(P>0.05).The incidence of gestational diabetes mellitus and anemia of the observation group were significantly lower than those of control group,the differences were statistically significant(P<0.05).(3)There were no significant differences in cesarean section rate and postpartum hemorrhage rate between the two groups(P>0.05).Conclusion:Mobile health is a kind of health education,which can reduce pregnancy weight gain,and reduce the incidence of gestational diabetes mellitus and anemia.It has no effect on neonatal birth weight,mode of delivery and postpartum hemorrhage.
本研究顯示:與對照組相比,觀察組孕婦的血紅蛋白水平明顯高于對照組(P<0.05)。說明通過移動醫療干預,結合孕婦常規的保健檢查結果,對孕婦進行生活方式指導并提出建議,使孕婦有意識補充鐵劑,有利于防止孕期貧血。兩組新生兒出生體重比較,差異無統計學意義(P>0.05)。孕期體重增長與新生兒出生體重具有一定相關性,本研究顯示觀察組孕婦體重增長少于對照組,但新生兒體重比較,差異無統計學意義(P>0.05),推測與樣本較少有關,有待于進一步擴大樣本深入研究。此外,觀察組妊娠期糖尿病及貧血發生率均明顯低于對照組,差異有統計學意義(P<0.05);而兩組妊娠期高血壓疾病發生率比較,差異無統計學意義(P>0.05)。由于移動醫療干預主要通過健康教育對孕婦進行生活方式的干預和指導,妊娠期糖尿病和貧血與孕婦飲食、運動等生活方式關系密切,因此,通過生活方式干預可降低妊娠期糖尿病和貧血的發生。而妊娠期高血壓疾病的發病因素較為復雜,并非單獨由于不良生活方式引起,因此移動醫療干預對于其發病影響不大,并且該病發病率約7%[10],本研究樣本較少,應進一步擴大樣本研究移動醫療對于妊娠期高血壓疾病的意義。而兩組剖宮產率及產后出血率比較,差異均無統計學意義(P>0.05)。分析原因可能為分娩方式及產后出血涉及諸多因素,社會因素、分娩鎮痛、胎兒大小、骨盆大小、產程進展及產后子宮收縮等因素,移動醫療通過醫患互動宣教分娩方式、生活方式干預等,可增加患者的生育知識,可增加依從性,但是并不能代替醫院的醫療操作,因此對于剖宮產率和產后出血率影響不明顯。
綜上所述,移動醫療是現代化的健康教育手段,可通過智能手機增加醫患互動,增加患者生育健康知識,增加患者的依從性,并可對患者進行生活方式干預,控制孕期體重增長,減少貧血及妊娠期糖尿病的發生;并且移動醫療方便可行,費用低,很受廣大孕婦喜愛。因此,移動醫療有望成為一種新的健康教育和管理模式。但是,移動醫療是一種健康教育方式,不能代替真正的醫療操作和檢查,對于產后出血及分娩方式的影響并不明顯,因此移動醫療可作為一種常規醫療的補充和宣教。關于移動醫療對于孕期健康管理的作用仍有待進一步探討和研究。
參考文獻
[1] Kallander K,Tibenderana J K,Akpogheneta O J,et al.Mobile health(mHealth) approaches and lessons for increased performance and retention of community health workers in low-and middle-income countries:a review[J].J Med Internet Res,2013,15(1):e17.
[2] Park S H,Hwang J,Choi Y K.Effect of Mobile Health on Obese Adults:A Systematic Review and Meta-Analysis[J].Health Inform Res,2019,25(1):12-26.
[3] Bush J,Barlow D E,Echols J,et al.Impact of a Mobile Health Application on User Engagement and Pregnancy Outcomes Among Wyoming Medicaid Members[J].Telemed J E Health,2017,23(11):891-898.
[4]中華醫學會婦產科學分會產科學組.孕前和孕期保健指南(2018)[J].中華婦產科雜志,2018,53(1):7-13.
[5] Henriksson P,Sandborg J,Blomberg M,et al.A Smartphone App to Promote Healthy Weight Gain, Diet,and Physical Activity During Pregnancy (HealthyMoms):Protocol for a Randomized Controlled Trial.JMIR Res Protoc,2019,8(3):e13011.
[6] Chan K L,Chen M.Effects of Social Media and Mobile Health Apps on Pregnancy Care:Meta-Analysis[J].JMIR Mhealth Vhealth,2019,7(1):e11836.
[7] Bowser D M,Shepard D S,Nandakumar A,et al.Cost Effectiveness of Mobile Health for Antenatal Care and Facility Births in Nigeria[J].Ann Glob Health,2018,84(4):592-602.
[8] Saronga N J,Burrows T,Collins C E,et al.mHealth interventions targeting pregnancy intakes in low and lower-middle income countries:Systematic review[J].Matern Child Nutr,2019,15(2):e12777.
[9] Redman L M,Gilmore L A,Breaux J,et al.Effectiveness of SmartMoms,a Novel eHealth Intervention for Management of Gestational Weight Gain:Randomized Controlled Pilot Trial[J].JMIR Mhealth Uhealth,2017,5(9):e133.
[10] Meggyes M,Miko E,Lajko A,et al.Involvement of the PD-1/PD-L1 Co-Inhibitory Pathway in the Pathogenesis of the Inflammatory Stage of Early-Onset Preeclampsia[J].Int J Mol Sci,2019,20(3):583.
(收稿日期:2019-04-08) (本文編輯:桑茹南)

