Early changes of retinal and choroidal microvascular structure in hypertensive patients
Abstract
?AIM:To explore the feasibility of swept source optical coherence tomography angiography (SS-OCTA) in evaluating early retinal and choroidal microcirculation changes in patients with hypertension.
?METHODS:Prospective clinical study. A total of 27 patients with grade 2 or 3 essential hypertension (hypertension group) diagnosed in the Department of Cardiology of Xi’an First Hospital from July to November 2022 were included in the study. There were 14 males and 13 females. The mean age was (57.11±3.36) years. During the same period, 27 age- and sex-matched normal people without a history of hypertension were selected as the control group, including 12 males and 15 females. The average age was (55.74±2.95) years old. All patients underwent BCVA (LogMAR), intraocular pressure, axial length, slit lamp examination, fundus color photography and SS-OCTA examination. SS-OCTA was used to scan the macular area of the right eye in the range of 6×6 mm. The retina and choroid were divided into three concentric circles with diameters of 0-1 mm, 1-3 mm and 3-6 mm around the fovea according to ETDRS. Macular vessel density (VD), perfusion area (PA), retinal thickness (CMT), choroidal thickness (CT), choroidal vessel volume (CVV) and choroidal vasculr index (CVI) of the superficial capillary plexus (SCP) and the deep capillary plexus (DCP) in the macular area of 0-1 mm, 1-3 mm and 3-6 mm were analyzed and recorded. The changes in VD, PA, CMT, CT, CVV and CVI were compared between the two groups. Independent sample t-test was used to compare VD, PA, CMT and CVI between the two groups; CT, CVV and LogMAR visual acuity were analyzed by Wilcoxon signed rank test of independent samples.
?RESULTS:Compared with the control group, the hypertensive group had significantly lower VD in the macular area 0-3 mm (0-1 mm, t=-3.144; 1-3 mm, t=-3.611, P<0.05). VD in the area of 3-6 mm showed a tendency to increase compared with the control group (t=1.715, P>0.05). The CMT in the 0-1mm area of the macular area in the hypertension group was lower than that in the control group (t=-2.624, P<0.05). There was no significant difference in CT, CVV and CVI between the two groups (P>0.05).
?CONCLUSION:The VD of DCP in the 0-3 mm area and the CMT in the 0-1 mm area are decreased in hypertensive patients. There were no significant differences in CT, CVV and CVI between the two groups. VD and CMT in macular DCP may be used as indicators to evaluate the early changes of retinal and choroidal microcirculation in hypertensive patients.
KEYWORDS:hypertensive retinopathy; vessel density; swept-source optical coherence tomography angiography; choroidal vascularity index; retinal microvascular
INTRODUCTION
Hypertension, as a serious global health problem, is a major risk factor for cardiovascular disease and death[1]. Long-term hypertension can lead to damage to the structure and function of target organs such as cardiovascular and cerebrovascular, kidney and eye. Early detection of target organ damage in hypertension is of great significance for improving the quality of life of patients and improving the prevention and treatment of hypertension. The eye is the only organ in the human body where microvascular abnormalities can be directly observed. Subclinical target organ damage in hypertension includes hypertensive retinopathy (HRP) of Keith-Wagener (K-W) grade 1-2, while 2/3 of hypertensive patients have HRP of grade 1-2[2]. K-W classification is mainly based on ophthalmoscope or fundus photography. It is difficult to strictly distinguish between grades 1 and 2 in clinical practice, and it mainly depends on doctors’ experience and is affected by subjective factors.
In order to objectively evaluate the early fundus changes in patients with hypertension, current studies are mostly based on retinal vessel density (VD) and retinal thickness quantified by optical coherence tomography angiography (OCTA), and subfoveal choroidal thickness (SFCT) by enhanced depth imaging OCT (EDI-OCT) technology to evaluate the choroidal changes. However, SFCT is affected by many physiological factors. And the variability is large, and the results of the correlation with hypertension are also different. In recent years, swept source OCTA (SS-OCTA) has made extraordinary development recently. As a new biological measurement tool, SS-OCTA enables a longer wavelength, a stronger penetration and a clearer choroidal imaging. Three-dimensional imaging and quantitative analysis of retinal and choroidal vessels can be carried out through optimization algorithms, and changes in choroidal structure can be effectively evaluated[3]. At present, it has been widely used in the detection of choroidal structure in central serous chorioretinopathy (CSC), age-related macular degeneration (AMD), diabetic retinopathy (DR) and other eye diseases. Therefore, in this study, SS-OCTA was used to measure macular VD, perfusion area (PA), central macular thickness (CMT), choroidal thickness (CT), choroidal vessel volume (CVV) and choroidal vascular index (CVI) in a group of essential hypertension patients without definite HRP. To explore the feasibility of SS-OCTA in evaluating early retinal and choroidal microcirculation changes in patients with hypertension.
SUBJECTS/MATERIALS AND METHODS
A prospective clinical study. The study adhered to the principles of the Declaration of Helsinki, and the subjects were informed and signed written informed consent.
A total of 27 patients with grade 2 or 3 essential hypertension diagnosed in the Department of Cardiology of Xi’an First Hospital from July to November 2022 were included in this study (hypertension group), including 14 males and 13 females; the mean age was (57.11±3.36) years. During the same period, 27 age- and sex-matched normal people without a history of hypertension were selected as the control group, including 12 males and 15 females. The average age was (55.74±2.95) years old. Inclusion criteria: 1) age 50-70 years old; 2) patients with primary hypertension of grade 2 or grade 3, whose diagnostic criteria were in accordance with the Chinese Guidelines for Hypertension Prevention and Treatment, 2018 Revised Edition, including those with normal blood pressure under drug control; 3) hypertension duration >5a; 4) HRP grading standard was in accordance with K-W grading standard of grade 0 and grade 1, that is, no obvious retinal artery constriction, arteriovenous cross compression sign, fundus exudation or hemorrhage, optic disc edema were found; 5) voluntary cooperation with relevant examinations, OCTA signal intensity ≥7/10. Exclusion criteria: 1) secondary hypertension or malignant hypertension; 2) history of systemic diseases affecting microvascular perfusion such as diabetes mellitus, arrhythmia and coronary heart disease; 3) high myopia or hyperopia; 4) patients with corneal or intraocular diseases or cataract that affect the examination results.
All subjects underwent best corrected visual acuity(BCVA), intraocular pressure, axial length, slit lamp examination, fundus color photography and SS-OCTA examination. BCVA examination was performed using the standard logarithmic visual acuity chart, which was converted to the logarithm of the minimum angle of resolution (LogMAR) visual acuity. SS-OCTA examination was performed using the VG200D of Vision Micro Imaging (Henan) Technology Co., Ltd. All the examinations were performed by the same senior physician. The right eyes of all subjects were selected, the scanning range was 6mm×6mm, and the image signal intensity was ≥7. The retina and choroid were divided into three concentric circles with diameters of 0-1 mm, 1-3 mm and 3-6 mm around the fovea according to ETDRS. VD, PA, CMT, CT, CVV, and CVI of superficial capillary plexus (SCP) and deep capillary plexus (DCP) in the macular area of 0-1 mm, 1-3 mm, and 3-6 mm were analyzed and recorded by the self-provided software (Figure 1). The level of SCP is from the inner limiting membrane to the inner plexiform layer; the level of DCP is from the inner nuclear layer to the outer plexiform layer. CVV was the total volume of choroidal vessels per unit measurement area. CVI is the ratio of CVV obtained after choroidal image processing to the total choroidal volume, which reflects the choroidal VD per unit volume.
RESULTS
RetinalbloodflowdensityandfovealmorphologyThe VD and PA of SCP in the 0-6 mm area of the macular area in the hypertension group were lower than those in the control group, but the differences were not statistically significant (P>0.05). The VD and PA of DCP in the 0-3 mm area in the hypertensive group were lower than those in the control group, and the difference of VD was statistically significant (P<0.05), but the difference of PA was not statistically significant (P>0.05). The VD and PA of the DCP in the 3-6mm area of the macular area in the hypertension group were higher than those in the control group, but the difference was not statistically significant (P>0.05). The CMT in the 0-6 mm area of the macular area in the hypertension group was lower than that in the control group, and the difference was statistically significant in the 0-1 mm area (P<0.05).
ChoroidalvascularparametersandthicknessThere was no significant difference in CT, CVV and CVI in the 0-6 mm area of the macular area between the two groups (P>0.05).
DISCUSSION
In this study, SS-OCTA was used to quantitatively describe the changes in the microvascular structure of the macular retina and choroid in a group of essential hypertension patients without obvious HRP. A number of studies have analyzed retinal and choroidal biomarkers and microvascular morphology by SS-OCTA[4-5], which have proved that these quantitative parameters have good repeatability and reliability. The patients included in this study were patients with chronic hypertension under drug control, and the data obtained were all in the normal state of blood pressure control.
This study showed that VD in the 0-3mm area of the macular area in the hypertensive group was significantly reduced in the DCP, and there was also a trend of reduction in the SCP, which was similar to the results of Sunetal[6]and Liuetal[7]. This phenomenon is also present in a number of other diseases including DR and retinal vein occlusion[6]. This may be related to the anatomical and functional distribution of the retina. SCP plexus is mainly distributed in the ganglion cell layer, connected with the retinal arterioles, and there is a large perfusion pressure. The DCP, however, is distributed within the inner nuclear layer and is mainly composed of venous collecting channels, which are conduits for blood from the SCP to the deep veins, where there are more retinal capillary termination units, making it more distant from the arterial circulation and therefore more vulnerable to disruption by retinal blood flow. Bonninetal[8]reported different patterns of two capillary plexuses in normal individuals. In SCP, capillaries are arranged between arterioles and venules, forming an interconnected transverse capillary plexus. However, in the DCP, which consists of polygonal units, the capillaries converge radially toward the middle, which is called the vortex of the capillary. They speculated that the different patterns and structures of the two capillary plexuses might be related to their flow resistance and perfusion[8]. We also found that the VD of the DCP in the macular area of 3-6mm in the hypertensive group tended to be higher than that in the normal group. We speculate that this may be a compensatory mechanism to provide greater arterial pressure to the foveal capillaries.
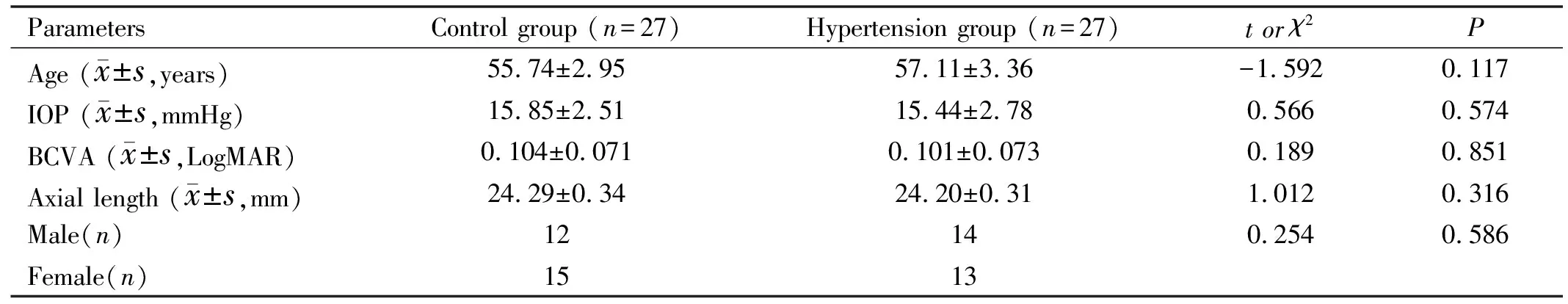
Table 1 Basic information of the control group and the hypertension group
In our study, we found that CMT in the hypertensive group was significantly thinner within the range of 0-1 mm, which may be closely related to the anatomy of the macular area. The macular area is the thinnest area of the retina, the densest cone cells, and the peripheral capillary network is rich. Arterioles arise from the side of the retinal branch arteries at an angle of 90° and directly supply the macular capillary network. Blood flow into these arterioles requires high perfusion pressure. The center of the macula is the avascular zone, where the capillary network forms the macular arch ring structure and terminates. The special anatomical structure of vessels in the macular area makes its density susceptible to hypertensive arteriolar lesions[9]. Some patients in the chronic hypertension group may have experienced early hypertensive events, leading to retinal blood circulation disorders, hardening or shrinkage of its microstructure[10], leading to retinal thickness thinning. The anatomical structure of the fovea makes its thickness more susceptible to thinning.
The normal structure and function of the choroid are essential for the maintenance of retinal function, and abnormal or reduced choroidal blood flow can cause photoreceptor cell dysfunction[11]. Therefore, studying choroidal circulation and thickness is helpful to detect early ocular changes in patients with essential hypertension. Previous studies of the choroid have focused on CT. Studies have found that CT is related to age, gender, intraocular pressure, axial length and systolic blood pressure. SFCT under the age of 60 has nothing to do with age, while SFCT decreases with age over the age of 60[12]. SFCT is thicker in males than in females[13]. CT is negatively correlated with axial length[14]. In our study, there was no statistical difference in the above factors between the two groups, thus reducing the influence on CT. The results showed that there was no significant difference in the macular area 0-6 mm between the two groups. This is the same as the results of Shaoetal[15]and G?ketal[16]. However, the effect of hypertension on CT is controversial. Mittaletal[17]found that SFCT decreased in hypertensive patients. Simseketal[18]also found that CT was reduced in patients with systemic hypertension, and they suggested that it might be due to arteriosclerosis of choroidal arterioles caused by hypertension, leading to a reduction in thickness caused by vasoconstriction.
To further illustrate the effect of hypertension on choroidal vascular structure, choroidal vascular parameters CVV and CVI were used. Among them, CVI is a more powerful marker of choroidal diseases. CVI is relatively less affected by physiological factors, and its coefficient of variation is much smaller than SFCT[19], which has a tendency to gradually replace SFCT. At present, only axial length and age are considered as factors affecting the outcome of CVI[20]. Our results showed that there was no significant difference in CVV and CVI in the 0-6 mm area of the macular region between the two groups. Studies have shown that the choroid is very sensitive to blood pressure changes, and the pathophysiological response to blood pressure changes is obviously different from that of the retinal vascular system. The choroid is sympathetic innervated and sensitive to vasoconstrictor factors of the circulatory system such as angiotensin 2, epinephrine, vasopressin, and these factors and nerve stimuli can initiate choroidal and choriocapillary vasoconstriction, leading to ischemia[21], which may reduce SFCT. If chronic hypertension persists, the choroid will enter a chronic repair phase, occluded choroidal arteries, arterioles and choroid capillaries will be recanalized and repaired, and the CT will also be thickened at the same time. Therefore, chronic hypertension changes within a certain range, and the choroid is regulated by neural and humoral factors and responds to maintain optimal retinal perfusion pressure[16], so that CT and blood flow remain normal. The patients in our hypertensive group were all taking antihypertensive drugs, which may have contributed to the improvement in choroidal blood flow and ultimately affected CT.
In conclusion, our present study showed that the VD of DCP in the 0-3 mm area and the CMT in the 0-1 mm area were decreased in the hypertensive group, and there were no significant differences in CT, CVV and CVI in the 0-6 mm area between the two groups. We speculate that VD and CMT in macular DCP may be used as indicators to evaluate the early changes of retinal and choroidal microcirculation in hypertensive patients.