頜骨囊腫摘除術聯合同期引導骨再生技術修復術后骨缺損的臨床療效分析
[摘要]目的:探討頜骨囊腫摘除術聯合同期引導骨再生技術(Guided bone regeneration,GBR)對頜骨囊腫患者的療效及對骨缺損的修復作用。方法:選取2018年1月-2022年12月安徽醫科大學第一附屬醫院收治的60例頜骨囊腫患者,根據其治療方法將其分為研究組(30例)及對照組(30例),對照組采用頜骨囊腫摘除術進行治療,研究組采用頜骨囊腫摘除術聯合同期GBR技術治療。采用錐形束CT(Cone beam CT,CBCT)影像學參數評估患者骨缺損修復情況,比較兩組術后3個月、6個月的囊腫體積縮小量、囊腫面積縮小量、骨密度、骨質增生厚度、頜骨高度及寬度;比較兩組患者的臨床療效。結果:兩組患者術后3個月及術后6個月CT值均高于術前(P<0.05),術后6個月均高于術后3個月(P<0.05),且研究組術后3個月及術后6個月CT值高于對照組(P<0.05);兩組術后6個月囊腫體積縮小量及囊腫面積縮小量均大于術后3個月(P<0.05),且研究組術后3個月及術后6個月囊腫體積縮小量及囊腫面積縮小量均大于對照組(P<0.05);兩組術后6個月骨密度及骨質增生厚度均高于術后3個月(P<0.05),且研究組術后3個月及術后6個月的骨密度、骨質增生厚度均高于對照組(P<0.05);兩組術后6個月上下頜骨高度及寬度均高于術后3個月(P<0.05),且研究組術后6個月上下頜骨高度及寬度均高于對照組(P<0.05);研究組臨床有效率高于對照組(P<0.05)。結論:頜骨囊腫摘除術聯合同期GBR技術能夠顯著修復骨缺損,有效縮小囊腫體積及面積,促進頜骨生長發育,療效顯著。
[關鍵詞]頜骨囊腫摘除術;引導骨再生技術;頜骨囊腫;骨缺損;骨密度
[中圖分類號]R782.4" " [文獻標志碼]A" " [文章編號]1008-6455(2024)12-0068-04
Analysis of Clinical Effect of Mandibular Cyst Excision Combined with Simultaneous Guided Bone Regeneration Technique for Repairing Postoperative Bone Defect
ZHANG Zhe, CHEN Shengfeng, YANG Bin, LI Yong
( Department of Stomatology, Dongcheng Hospital, the First Affiliated Hospital of Anhui Medical University, Hefei 231600,
Anhui, China )
Abstract: Objective" To explore the curative effect of jaw cyst excision combined with simultaneous guided bone regeneration (GBR) on patients with jaw cyst and the repair of bone defect. Methods" 60 patients with jaw cysts who were treated in First Affiliated Hospital of Anhui Medical University from January 2018 to December 2022, and divide them into study group (30 cases) and control group (30 cases) according to their treatment methods. The control group was treated with removal of jaw cyst, while the study group was treated with removal of jaw cyst combined with GBR technology at the same time. Evaluation of bone defect repair in patients with cone-beam CT (CBCT) imaging parameters. The reduction of cyst volume, reduction of cyst area, bone density, thickness of bone hyperplasia, height and width of jaw bone in the two groups were compared 3 and 6 months after operation. The clinical efficacy of the two groups were compared. Results" The CT values of patients in the two groups were higher than those before operation at 3 months and 6 months after operation (P<0.05), Six months after operation were higher than three months after operation (P<0.05), The CT value of the study group was higher than that of the control group at 3 months and 6 months after operation (P<0.05). The reduction of cyst volume and area in both groups at 6 months after operation was greater than that at 3 months after operation (P<0.05), The reduction of cyst volume and area in the study group were greater than those in the control group at 3 months and 6 months after operation (P<0.05). The bone mineral density and thickness of bone hyperplasia in the two groups at 6 months after operation were higher than those at 3 months after operation (P<0.05), and the bone mineral density and thickness of bone hyperplasia in the study group at 3 months and 6 months after operation were higher than those in the control group (P<0.05). The height and width of maxilla and mandible in the two groups at 6 months after operation were higher than those at 3 months after operation (P<0.05), In addition, the height and width of maxilla and mandible in the study group were higher than those in the control group 6 months after operation (P<0.05). The clinical effective rate of the study group was higher than that of the control group (P<0.05). Conclusion" Jaw cyst excision combined with simultaneous GBR technology can significantly repair bone defects, effectively reduce the size and area of the cyst, and promote the growth and development of the jaw, with significant curative effect and high safety.
Key words: excision of cyst of jaw; guided bone regeneration technology; jawbone cyst; bone defect; bone density
頜骨囊腫是口腔頜面部常見病、多發病之一,指出現在根端的炎性囊腫,具有病程長、發病隱匿的特點,此病可發生在任何年齡階段[1]。頜骨囊腫早期癥狀不明顯,但隨著病情發展,囊腫逐漸變大,頜骨受損,嚴重者可導致面部畸形,部分患者還可出現神經性癥狀,甚至發生感染,對患者的生活及健康造成不良影響[2-3]。傳統治療主要是對患者進行頜骨囊腫摘除術,但術后囊腔空置易出現積液、積血,且術后腫脹及疼痛消退時間較長,不僅增加了患者的痛苦,且影響其術后恢復[4]。同期引導骨再生技術(GBR)逐漸應用在骨缺損中,通過骨移植或骨替代品填充,能夠加速骨愈合,減少組織塌陷造成的不良影響[5]。目前,鮮有文獻報道應用GBR技術修復頜骨囊腫所致骨缺損,因此,本研究將頜骨囊腫摘除術聯合同期GBR技術應用于頜骨囊腫患者的治療中,以期為臨床治療頜骨囊腫提供參考。
1" 資料和方法
1.1 一般資料:選取筆者醫院于2018年1月-2022年12月收治的60例頜骨囊腫患者,根據其治療方法將其分為研究組(30例)及對照組(30例)。研究組男15例,女15例;年齡13~81歲,平均(37.82±8.76)歲;發病位置:上頜骨18例,下頜骨12例;病程1~16個月,平均(10.83±3.71)個月;對照組男12例,女18例;年齡8~78歲,平均(38.24±8.85)歲;發病位置:上頜骨17例,下頜骨13例;病程2~18個月,平均(10.37±3.56)個月;兩組性別、年齡、發病位置及病程比較差異無統計學意義(P>0.05)。本研究已經醫院醫學倫理審核批準(YK-20170506)。
1.1.1 納入標準:均符合《開窗治療頜骨囊性病變的專家共識》[6]中頜骨囊腫的診斷標準;經錐束CT檢查確診為頜骨囊腫;患者對本研究知情同意并簽署知情同意書。
1.1.2 排除標準:嚴重心肝腎功能障礙者;凝血系統障礙者;合并影響骨愈合、再生系統性疾病者;合并傳染疾病者;妊娠及哺乳期患者;合并精神疾病者。
1.2 方法
1.2.1 對照組:采用頜骨囊腫摘除術治療,口內切口,在口腔前廳處做角形或梯形切口,用骨鑿或動力系統磨除部分骨壁,顯露囊壁組織,用咬骨鉗去除囊腫表面骨質,用骨膜分離器或刮匙摘除囊壁,最后沖洗囊腔,縫合黏骨瓣膜。
1.2.2 研究組:采用頜骨囊腫摘除術聯合同期GBR技術治療,頜骨囊腫摘除方法與對照組一致,摘除后使用0.05%氯己定溶液與生理鹽水交替沖洗囊腔,根據囊腔大小植入適量骨粉和自體血混合物,將生物膜按所需部位修剪形態,覆蓋在和骨缺損區表面并固定,復位黏骨膜瓣,縫合切口;術后創口局部冷敷24 h,給予生理鹽水含漱,3次/天,1~2周后拆線,術后3個月及6個月復診。
1.3 觀察指標
1.3.1 骨修復情況:分別于術前、術后3個月及6個月采用CBCT進行檢測患者骨缺損區CT值,選取感興趣區(Area of Interest,ROI),在三維圖圖像上勾畫出病變區域,確保各個方向大小均與ROI一致,分別測量頰舌向、近遠中向和矢狀位方向CT值,各個CT值均連續測量3次,取其平均值作為結果。所有患者均由同一名放射科醫生進行CBCT檢測。
1.3.2 囊腫體積縮小量、囊腫面積縮小量:分別于術前、術后3個月及6個月時對患者進行CT影像學檢查,連續測量3次頜骨囊腫橫徑(a)、前后徑(b)及上下徑(b),取3次的平均值作為最終結果,計算囊腫體積以及面積,囊腫面積根據CT影像學結果得出,囊腫體積=4π×a×b×c/3,最后計算得出術后3個月及6個月的囊腫體積縮小量、囊腫面積縮小量。囊腫體積縮小量=術前囊腫體積-術后囊腫體積;囊腫面積縮小量=術前囊腫面積-術后囊腫面積。
1.3.3 兩組骨密度、骨質增生厚度:采用CBCT檢測患者術后3個月及6個月的骨密度、骨質增生厚度。
1.3.4 兩組患者頜骨高度及寬度:采用CBCT檢測患者術后3個月及6個月的上下頜骨高度及寬度,上頜骨高度從牙槽嵴頂到上頜竇底,下頜高度從牙槽嵴頂到下頜神經管上緣,頜骨寬度從植骨位點的頜骨頰側到舌側或腭側。
1.3.5 兩組患者臨床療效:于術后6個月對患者治療效果進行評估。治愈:臨床癥狀及囊腫完全消失、頜骨對稱良好,骨密度及骨質增生厚度完全恢復,頜骨高度及寬度增加30%以上;顯效:臨床癥狀及囊腫明顯改善,頜骨基本對稱,骨密度及骨質增生厚度基本恢復,頜骨高度及寬度增加低于30%;無效:臨床癥狀及囊腫沒有明顯改善,頜骨未對稱,骨密度、骨質增生厚度、頜骨高度及寬度沒有明顯變化。臨床有效率=(治愈+顯效)例數/總例數×100%。
1.4 統計學分析:采用SPSS 22.0統計學軟件進行數據分析,計量資料采用“xˉ±s”描述,組間采用t檢驗,組內采用配對樣本t檢驗;計數資料用“%”表示,采用“χ2”檢驗,P<0.05為差異具有統計學意義。
2" 結果
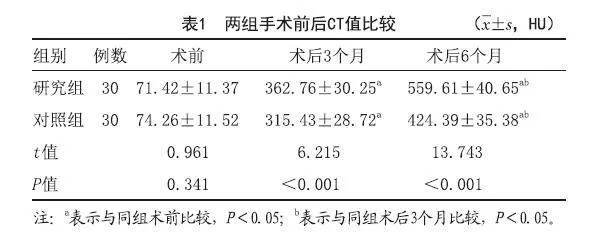
2.1 比較兩組患者CT值:兩組患者術后3個月及術后6個月CT值均高于術前(P<0.05),術后6個月CT值均高于術后3個月(P<0.05),且研究組術后3個月及術后6個月CT值高于對照組(P<0.05),見表1。
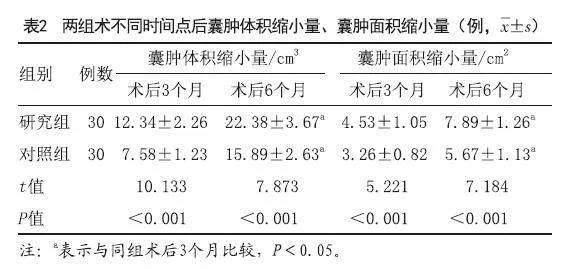
2.2 兩組囊腫體積縮小量、囊腫面積縮小量比較:兩組術后6個月囊腫體積縮小量及囊腫面積縮小量均大于術后3個月(P<0.05),且研究組術后3個月及術后6個月囊腫體積縮小量及囊腫面積縮小量均大于對照組(P<0.05),見表2。
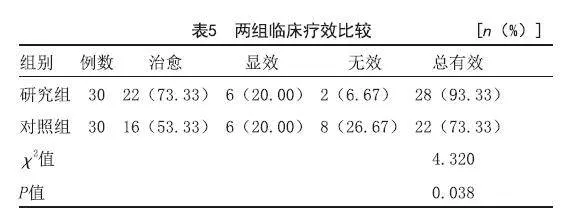
2.3 兩組骨密度、骨質增生厚度比較:兩組術后6個月骨密度及骨質增生厚度均高于術后3個月(P<0.05),且研究組術后3個月及術后6個月的骨密度、骨質增生厚度均高于對照組(P<0.05),見表3。
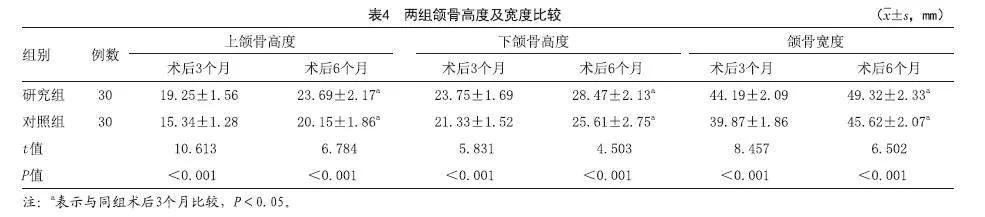
2.4 比較兩組頜骨高度及寬度:兩組術后6個月上下頜骨高度及寬度均高于術后3個月(P<0.05),且研究組術后6個月上下頜骨高度及寬度均高于對照組(P<0.05),見表4。
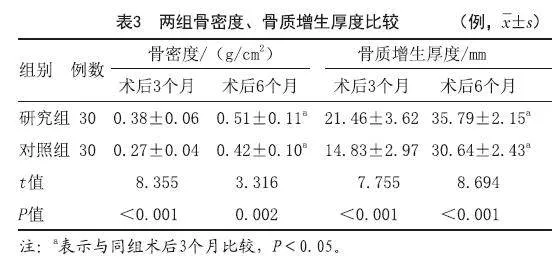
2.5 兩組臨床療效比較:研究組臨床有效率高于對照組(P<0.05),見表5。
3" 討論
頜骨囊腫是臨床常見的口腔頜面部良性病變,主要由牙組織或牙上皮發展而成,其生長較為緩慢,囊腫長期發展可造成頜骨膨隆,可導致面部畸形、牙齒松動移位以及牙根吸收,嚴重者還可引起下唇麻木等[7-8]。研究表明,頜骨囊腫能夠影響患者的面部容貌及咀嚼功能,若長期發展,可對患者造成永久性的身體及心理創傷[9]。因此對頜骨囊腫患者有效治療至關重要。
臨床常采用頜骨囊腫摘除術治療頜骨囊腫,該方式具有手術操作簡單、快捷,適用范圍較廣的優點,但當頜骨囊腫較大,臨近神經、血管或上頜竇時,其操作易造成重要解剖結構受損,從而導致術中出血量較大[10]。此外,頜骨囊腫摘除術后遺留骨質較薄,可增加病理性骨折的風險,且術后留下較大的囊腔影響患者面容[11]。另外,多數非病灶牙的牙髓會發生壞死,需對患者進行根管治療及修復治療,不僅影響患者的健康,且增加了患者的經濟壓力[12]。Ku JK等[13]研究發現,頜骨囊腫術后患者骨修復速度較慢,12個月后囊腫殘余缺損體積仍舊較大,骨缺損區域難以修復到原有生理結構及外形,骨愈合率較低。
本研究結果顯示,研究組術后3個月及術后6個月CT值、囊腫體積縮小量及囊腫面積縮小量、骨密度及骨質增生厚度、上下頜骨高度及寬度均高于對照組,臨床有效率高于對照組,說明頜骨囊腫摘除術聯合GBR技術能夠加快囊腫消除及骨缺損區骨愈合,提高骨生成率及骨密度。聯合GBR技術時,骨組織愈合通過機體炎性介質促進血管生成和間充質干細胞增殖、分化,形成局部微循環,而植入骨粉能夠為新生骨提供成骨基質及空間結構,進而完成骨改建,達到骨組織愈合[14-15]。另外,GBR生物膜對骨組織細胞具有引導骨再生作用,能夠直接參與骨愈合過程,其特有的三維網狀結構能夠聚集骨質細胞,促進局部骨缺損的修復,恢復其骨質量及頜骨外形[16]。研究發現,富血小板纖維蛋白聯合GBR技術修復種植體周圍炎骨缺損的療效顯著,術后60 d及術后120 d的骨密度較高,能夠促進骨缺損重建[17]。有研究表明,與單純頜骨囊腫刮治術比較,采用頜骨囊腫刮治術聯合GBR技術治療頜骨囊腫患者的囊腫縮小量、頜骨高度及寬度、骨密度及骨質增生厚度均較高,且復發風險較低,效果顯著[18]。另有研究顯示,富血小板纖維蛋白聯合GBR技術治療牙周病頜骨缺損患者,能夠促進骨組織修復及新生,有效提高骨密度,骨缺損修復效果較好[19]。結合本研究結果,頜骨囊腫摘除術聯合同期GBR技術能顯著提升頜骨囊腫患者的臨床療效,促進骨質生長、頜骨發育,修復頜骨缺損效果良好。
綜上所述,將頜骨囊腫摘除術聯合同期GBR技術應用于頜骨囊腫的治療中,能夠明顯增加囊腫體積及面積縮小量,提升骨密度、頜骨高度及寬度,增加骨質,修復骨缺損。
[參考文獻]
[1]Cserni G, Cserni D, Zombori T, et al. The role of interdisciplinary communication in the proper diagnostics of jaw cyst[J]. Orv Hetil, 2021,162(12):458-467.
[2]Banik R, Uddin M W, Asaduzzaman M, et al. Effect of application of platelet-rich plasma on bone regeneration after removal of jaw cysts[J]. Mymensingh Med J, 2022,31(1):107-111.
[3]Tamiolakis P, Thermos G, Tosios K I, et al. Demographic and clinical characteristics of 5294 cjaw cysts: a retrospective study of 38 years [J]. Head Neck Pathol, 2019,13(4):587-596.
[4]樊星,白振西,肖霞,等.植骨修復上頜骨囊腫術后骨缺損的臨床研究[J].實用口腔醫學雜志,2020,36(1):127-128.
[5]Yun J, Lee J, Ha C W, et al. The effect of 3-D printed polylactic acid scaffold with and without hyaluronic acid on bone regeneration[J]. J Periodontol, 2022,93(7):1072-1082.
[6]陶謙,何悅,劉冰,等.開窗治療頜骨囊性病變的專家共識[J].口腔疾病防治,2020,28(2):69-72.
[7]Ide F, Ito Y, Muramatsu T, et al. The advent of studies on jaw cysts with keratinization: a review of overlooked papers on odontogenic keratocyst and orthokeratinized odontogenic cyst[J]. Head Neck Pathol, 2020,14(3):785-791.
[8]Buchbender M, Neukam F W, Lutz R, et al. Treatment of enucleated odontogenic jaw cysts: a systematic review [J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2018,125(5):399-406.
[9]章禮玉,周瑜,葉茂昌,等.Image J軟件評估頜骨囊腫開窗減壓術的臨床療效研究[J].臨床口腔醫學雜志,2022,38(1):52-55.
[10]樊星,白振西,肖霞,等.同種異體松質骨修復頜骨囊腫術后骨缺損[J].生物骨科材料與臨床研究,2018,15(6):38-40.
[11]Marin S, Kirnbauer B, Rugani P, et al. The effectiveness of decompression as initial treatment for jaw cysts: Aa 10-year retrospective study[J]. Med Oral Patol Oral Cir Bucal, 2019,24(1):e47-e52.
[12]Shi J, Zhou J, Liu C, et al. Radiographic bone volume alteration after jaw cyst enucleation with or without simultaneous bone grafts: a prospective randomized study [J]. Clin Implant Dent Relat Res, 2022,24(4):468-474.
[13]Ku J K, Han M, Yongvikul A, et al. Volumetric analysis of spontaneous bone healing after jaw cyst enucleation[J]. Sci Rep, 2022,12(1):14953.
[14]Yang L, Zhou J, Yu K, et al. Surface modified small intestinal submucosa membrane manipulates sequential immunomodulation coupled with enhanced angio- and osteogenesis towards ameliorative guided bone regeneration [J]. Mater Sci Eng C Mater Biol Appl, 2021,119(115):111641.
[15]Wang B, Feng C, Liu Y, et al. Recent advances in biofunctional guided bone regeneration materials for repairing defective alveolar and maxillofacial bone: A review[J]. Jpn Dent Sci Rev, 2022,58:233-248.
[16]Hwang C, Park S, Kang I G, et al. Tantalum-coated polylactic acid fibrous membranes for guided bone regeneration[J]. Mater Sci Eng C Mater Biol Appl, 2020,5(115):111112.
[17]Sun G, Cao L, Li H. Effects of platelet-rich fibrin combined with guided bone regeneration in the reconstruction of peri-implantitis bone defect [J]. Am J Transl Res, 2021,13(7):8397-8402.
[18]陳軒,支強,費亦凡,等.引導骨再生技術聯合頜骨囊腫刮治術治療牙源性頜骨囊腫的臨床療效觀察[J].廣西醫學,2021,43(20):2389-2392,2396.
[19]謝紅幗,姚琴,盧驍鵬,等.富血小板纖維蛋白聯合引導骨再生技術治療牙周病頜骨缺損[J].中國新藥與臨床雜志,2019,38(8):489-493.
[收稿日期]2023-03-13
本文引用格式:張哲,陳圣峰,楊斌,等.頜骨囊腫摘除術聯合同期引導骨再生技術修復術后骨缺損的臨床療效分析[J].中國美容醫學,2024,33(12):68-71.