Beta-amyloid precursor protein cleavage enzyme-1 expression in adult rat retinal neurons in the early period after lead exposure**☆
Jufang Huang, Kai Huang, , Lei Shang, Hui Wang, Xiaoxin Yan, Kun Xiong
1Department of Anatomy and Neurobiology, Xiangya School of Medicine, Central South University, Changsha 410013, Hunan Province,China
2Department of Anatomy, Shaoyang Medical College, Shaoyang 422000, Hunan Province, China
lNTRODUCTlON
Lead is currently used worldwide for transport and in industrial production. A correlation between early exposure to lead during development and senile neurodegenerative diseases has been well documented in rodents and non-human primates[1-2]. However, the possible effects of adult lead exposure on neurodegenerative diseases remain largely unknown[3-5].
Retrospective studies have indicated that environmental factors may play a role in Alzheimer’s disease (AD)[6-7]. AD is a chronic,degenerative central nervous system disease affecting the elderly. The pathological characteristics of AD include the presence of β-amyloid deposits (senile plaques) and neurofibrillary tangles[8]. The amyloid deposition cascade hypothesis is one of the more widely accepted theories for the pathological mechanism of AD[9]. Lead exposure is associated with β-amyloid (Aβ)sediment and β-amyloid precursor protein(β-APP)[10]. β-amyloid precursor protein cleavage enzyme-1 (BACE-1) is an important rate-limiting enzyme involved in amyloid precursor protein (APP) cleavage[11].
APP is first cleaved into β-C-terminal fragments (β-CTF), which later change into Aβ, exerting neurotoxic effects. It is currently unclear whether BACE-1 expression is regulated and controlled in the early period of lead exposure. The precise function of BACE-1 in the process of further cleaving APP also remains to be elucidated. At present, most AD research is focused on the central nervous system, and particularly brain tissue. However, recent studies have indicated that the retina may provide a new approach for investigating neurodegenerative diseases and related molecules[12-13]. Therefore, the current study sought to investigate the effects of lead on BACE-1 expression and Aβ as its downstream product in a model of retinal lead exposure in adult rats. In addition, this paradigm enabled an examination of whether BACE-1 is a predominant agent in the overproduction of Aβ induced by lead exposure in the early period. This question is important for clarifying the molecular mechanisms of AD induced by environmental factors via the retina, which provides a novel window into the central nervous system.
RESULTS
Quantitative analysis of experimental animals
A total of 56 young adult Sprague-Dawley rats were randomly divided into seven groups, comprising five groups receiving single intraocular injections of lead acetate at different doses (10 μmol/L, 100 μmol/L,1 mmol/L, 10 mmol/L and 100 mmol/L), a vehicle control group (single intraocular injection with an equal volume of PBS) and a normal control group. All 56 rats were included in the final analysis.
Retinal lead level
At 48 hours after injecting different concentrations of lead acetate to vitreous body (10 μmol/L, 100 μmol/L, 1 mmol/L,10 mmol/L and 100 mmol/L), the retinal lead level was increased in all lead groups except the 10 μmol/L group, in a dose-dependent manner. In the 100 mmol/L group, lead concentration in the retina exceeded the equipment’s maximum measurement level, indicating that it could not be presented normally (Figure 1).

Figure 1 Retinal lead level after injecting different caoncentrations of lead acetate into the vitreous body.F = 282.205, P < 0.01, vs. normal control group or vehicle control group.
BACE-1 expression, as detected by western blot assay
BACE-1 was mainly exhibited as a single 50 kDa band in the western blot analysis. β-CTF (BACE-1 cleavage production) was mainly exhibited as a single 14 kDa band; and β-Tubulin was mainly exhibited as a single 55 kDa band. The BACE-1 and β-CTF bands became thicker and larger with increased lead acetate concentration in the vitreous body (100 μmol/L, 1 mmol/L,10 mmol/L and 100 mmol/L). The homogeneous intensity of β-Tubulin, as well as band size, demonstrated the similarity of total protein levels in each group. The average gray volume indicated that the average gray level of the BACE-1 and β-CTF bands (except 10 μmol/L group) showed a clear decrease as lead acetate concentration in the vitreous body increased, in a dose-dependent manner (Figure 2).

Figure 2 Western blot analysis results. After injecting lead acetate into the vitreous body, retinal β-amyloid precursor protein cleavage enzyme-1 (BACE-1) and β-C-terminal fragment (β-CTF) expression (A) and the analysis result of band average gray level (B). Comparison of retinal BACE-1 protein: aF = 89.957, P < 0.01, vs. normal control group or vehicle control group. Comparison of retinal β-CTF: bF = 106.654, P < 0.01, vs. normal control group or vehicle control group. I-VII: Normal control, vehicle control, 10 μmol/L, 100 μmol/L, 1 mmol/L, 10 mmol/L, 100 mmol/L lead acetate groups, respectively.
Aβ1-40 concentration of retinal tissue determined by enzyme linked immunosorbent assay (ELlSA)
Aβ1-40concentration of retinal tissue increased in all experimental groups, with the exception of the 10 μmol/L group, after 48 hours of injecting different concentrations of lead acetate to the vitreous body (10 μmol/L,100 μmol/L, 1 mmol/L, 10 mmol/L, and 100 mmol/L), in a dose-dependent manner (Figure 3).

Figure 3 β-amyloid 1-40 (Aβ1-40) concentration of retinal tissue after injecting different concentrations of lead acetate into the vitreous body (enzyme linked immunosorbent assay). aF = 22.984, P < 0.01, vs. normal control group or vehicle control group.
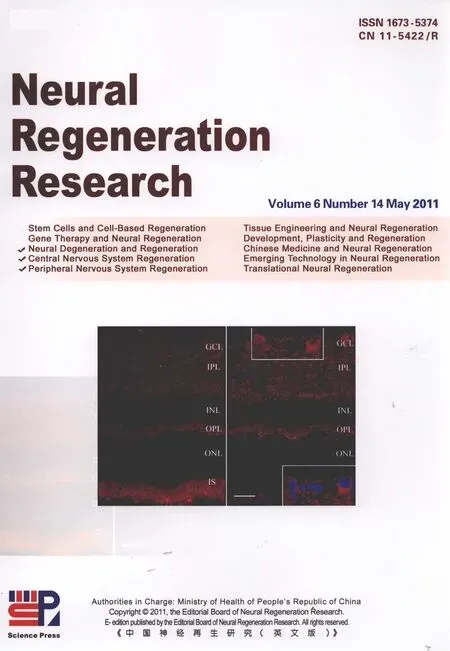
lmmunofluorescence staining
BACE-1 immunofluorescence staining: Normal retina BACE-1 positive production was primarily distributed in ganglion layer, the inner plexiform layer and the outer plexiform layer without distinct cell body staining. This result was congruent with the results of a previous study by our research group[14]. In the vehicle control group, the distribution characteristics of retinal BACE-1 were the same as in the normal retina (supplementary Figure 1 online). Increased concentration of lead acetate injected in vitreous body did not alter retinal BACE-1 distribution.
However, BACE-1 expression was upregulated in a dose-dependent manner. It should be noted that BACE-1 staining appeared in the ganglion cell body in the 100 mmol/L lead acetate group, indicating that higher concentrations of lead acetate caused ganglion cell over-expression of BACE-1 protein, especially in the cell bodies (Figure 4).
Glial fibrillary acidic protein (GFAP)immunofluorescence staining: A previous study reported that microglia do not express BACE-1 under physiological conditions, but under certain pathological conditions, neuronal BACE-1 can be upregulated and microglia can produce excessive BACE-1 after activation[15]. The current study evaluated whether microglia cells in the retina were activated, using GFAP immunofluorescence staining.
Our results indicated that, in the normal retina, strong GFAP staining was observed in the ganglion layer,while medium levels of staining were observed in the inner plexiform layer, inner nuclear layer and outer plexiform layer. In the vehicle control group, the distribution characteristics of retinal GFAP were the same as in the normal retina (supplementary Figure 2A online). We chose two lead exposure groups to illustrate the effects of concentration on distribution,the 100 μmol/L (median dose) and 100 mmol/L groups(for other concentrations, see supplementary Figures 2B-D online). No obvious changes in retinal GFAP were observed in terms of distribution range and intensity, suggesting that retinal microglia were not substantially activated (Figure 5).

Figure 5 Glial fibrillary acidic protein (GFAP) expression in normal rat retina is located in ganglion cell layer (GCL),inner plexiform layer (IPL) and inner nuclear layer (INL).The expression distribution showed no obvious changes in different concentration lead acetate treatment groups.OPL: Outer plexiform layer; ONL: outer nuclear layer.Scale bar: 20 μm.
Synaptophysin immunofluorescence staining:Synaptophysin is a specific pre-synaptic marker and its expression can indirectly reflect synaptic changes in the retina[16]. Our results revealed that synaptophysin showed a stratified distribution in the normal retina, and was mainly distributed in the inner plexiform layer and outer plexiform layer. The distribution characteristics of retinal synaptophysin in the vehicle control group were consistent with those in the normal retina (supplementary Figure 3A online). We chose two lead exposure groups to illustrate the effect of concentration on density, the 100 μmol/L (median) and 100 mmol/L groups (for other concentrations, see supplementary Figures 3B-D online).
No distinct changes were found in the distribution properties and intensity of retinal synaptophysin. These findings indicated that lead exposure in the early period did not induce apparent plasticity of retinal synapses(Figure 6).

Figure 6 Synaptophysin expression in the normal rat retina is located in the inner plexiform layer (IPL) and the inner nuclear layer (INL). The expression showed no obvious changes with different concentrations of lead acetate treatment. GCL: Ganglion cell layer; OPL: outer plexiform layer; ONL: outer nuclear layer. Scale bar:20 μm.
DlSCUSSlON
The retina is a suitable model for studying AD-related molecules
In the embryonic period, the retina is a constituent part of the central nervous system, which originates from the neural tube. The main types of neurons and glial cells of retina exhibit clear orientation morphology characteristics at the cellular and synapse levels, like the cells in the central nervous system. However, their organization and function are simple compared with brain tissue[17]. AD is a neurodegenerative disease that affects the central nervous system (particularly the cerebral cortex and hippocampus), exhibiting pathological features including β-amyloid deposition, neurofibrillary tangles and abnormal neuron loss[8]. A number of previous studies have demonstrated the existence of amyloid precursor protein in retinal neurons and the nerve fiber layer.
Furthermore, BACE-1, along with other molecules,contributes to the formation of amyloid plaques, and this has been observed in the inner and outer plexiform layers[14,18-19]. Recent studies have provided evidence of a significant reduction of ganglion cells, decreased thickness of the nerve fiber layer, and extensive degeneration of the optic nerve axis cylinder among AD patients. These findings indicate that the retina becomes impaired with the progressive development of AD[20-22].
Therefore, the retina can be considered a novel window for research into the molecular correlates of AD[12-13]. The retina is entirely surrounded by the wall of the eyeball,and substances injected into the vitreous body are confined to the retina. In the current study, we injected different concentrations of lead acetate to the vitreous body. We found that lead levels in retinal tissue showed a distinct dose-dependent increase. In addition, BACE-1 and Aβ molecules are thought to contribute to the development of AD, and exhibit predominant alterations.
Thus the present findings demonstrated that we successfully established a retinal model of AD based on the intervention of lead exposure.
Lead exposure induces early upregulation of BACE-1 expression in adult retinal neurons
Lead is widely distributed in low concentrations in the natural environment[2]. Long-term exposure to low concentrations of lead can cause chronic lesions in the central nervous system. There is evidence that this process involves interference of neurotransmitter release(such as dopamine, enkephalin and glutamate), changes in calmodulin protein kinase activity, and damage to the blood-brain barrier system[23]. A previous study proposed that persistent concentration to low levels of lead over a long period may be a risk factor for AD[24]. Age-related Aβ deposition and neurofibrillary tangles can also be observed in the brains of animals and humans exposed to high concentrations of lead, as well as in AD patients[25-26]. The amyloid deposition cascade hypothesis, proposing that Aβ plays a key role in the disease process, is currently widely accepted as the dominant theory of AD etiology[9]. As the most important type of β-secretase, BACE-1 functions as a critical and rate-limiting enzyme in the process of cleaving APP into Aβ. Furthermore, excessive Aβ can be produced as a result of increased expression and activity of BACE-1[11].
Thus a thorough understanding of the regulation of BACE-1 is an important step in elucidating AD pathogenesis. A number of studies have confirmed various risk factors of AD, including oxidative stress, free radical disorders, disturbance of blood circulation,neuronal injury, repression/depression of neuronal activity/metabolism, and mitochondrial dysfunction, all of which can produce excessive Aβ after upregulation of BACE-1, which results in AD[27-30]. The present results indicated that BACE-1 expression in the retina is upregulated (as well as its cleavage products β-CTF and Aβ1-40) 48 hours after injecting different concentrations of lead acetate to the vitreous body in a dose-dependent manner (except at the lowest concentration). Zhao et al[15]reported that microglia cells were involved in BACE-1 expression after activation in transgenic AD model animals. However, the current results did not indicate activation of retinal microglia cells, suggesting that lead exposure may disrupt BACE-1 regulation in the neuron itself, rather than the microglia. Several studies have demonstrated that persistent exposure to high concentrations of lead may destroy configurations of neurons[31]. Nevertheless, our findings provide evidence that there are no obvious synaptic changes in the retina in the early period of lead exposure. This result suggests that although lead exposure exerts negative effects on intracellular molecular regulation, it does not cause changes in neuronal synaptic plasticity directly. We propose that once these negative factors exceed the tolerance limit of neurons, causing irreversible lesions to neural synapses in the whole retina[32-36]. In summary,the current results suggest that lead exposure can cause excessive production of Aβ in the early period.
Additionally, the molecular mechanism may involve the regulation of BACE-1. These results extend current understandings of the relationship between lead exposure and AD.
MATERlALS AND METHODS
Design
Randomized, controlled, animal experiment.
Time and setting
This experiment was performed at the Department of Anatomy and Neurobiology, Xiangya School of Medicine,Central South University in China, from March to September in 2010.
Materials
A total of 56 healthy, Sprague-Dawley rats of either sex,weighing 200-250 g, aged 2-3 months, and with no external eyeball deformation or injury, exhibiting isocoria,and transparency, were obtained from the Experimental Animal Center of Xiangya School of Medicine, Central South University in China. The rats were placed into an animal house with 12-hour light/dark cycles at 24°C for 2-3 days. All of the procedures were conducted in accord with the experimental animal use and welfare requirements of the Ministry of Health of China.
Methods
Animal model preparation
Adult Sprague-Dawley rats were intraperitoneally anesthetized with 10% chloral hydrate (0.4 mL/kg), and fastened with a stereotaxic instrument (Jingyi, Shanghai,China) to fully expose the eyeball. Subsequently,different concentrations of 5 μL lead acetate were slowly injected directly into the left vitreous body. After the operation, they were caged individually in an air-conditioned environment at 24°C, with free access to food and water. Rats that died during the operation were replaced. Equal amounts of PBS were injected into the left vitreous body in the vehicle control group. No treatment was performed on rats in the normal control group. The contralateral eyeballs were not treated in any groups.
Tissue preparation
For morphological examination, four rats from each group were randomly selected for deep anesthesia with 10% chloral hydrate after surviving for 48 hours following the operation. The animals were perfused transcardially with 4% paraformaldehyde. Eyeballs were removed to produce optic cups, and postfixed with 4%paraformaldehyde for 24 hours. The tissue was cut in a cryostat at -20°C at 15 μm. All of the sections were adhered directly on gelatin-covered glass slides, which were preserved in the refrigerator at -20°C for preparation.
Biochemistry
Four rats from each group were anesthetized with 10%chloral hydrate after surviving for 48 hours. Eyeballs were then removed and placed on crushed ice, and the retina was quickly disconnected into a 1.5 mL centrifuge tube. Cell lysis buffer (Pierce, Rockford, IL, USA) was added to the retina in each tube according to the mass ratio (1: 10), homogenized by ultrasound and kept for 1 hour on crushed ice. After centrifugation at 4°C at 12 000 × g for 15 minutes, the supernatant was obtained and the protein concentration was adjusted equally by Coomassie brilliant blue (Sigma, St. Louis, MO, USA)staining. All settled fresh tissues were packaged according to their equivalent. Half of the tissues were kept in the refrigerator at -20°C, while the other half were added to 5 × loading buffer (Fermentas, Foster City, CA,USA) according to a volume ratio of 4: 1. The tissues were kept in refrigerator at 4°C, and used after boiling for 10 minutes.
Retinal lead level
Degenerative fresh retina tissues (40 μL per tube) were obtained from the different groups and defrosted. These tissues were tested for retinal lead levels using graphite furnace atomic absorption spectrophotometry[37-38](Bohui,Beijing, China) at the inspection division, Third Xiangya Hospital of Central South University in China. The final concentration was expressed as μg/L retina homogenate.
Western blot assay
The retina homogenates were examined with 10%sodium dodecyl sulfate polyacrylamide gel electrophoresis gel electrophoresis (constant voltage 100 V). Protein electrophoresis was transferred to nitrocellulose membrane (250 mA, 120 minutes). The primary antibodies used were rabbit anti-BACE-1(polyclone, AB5940; Chemicon, Temecula, CA, USA;1: 400), rabbit anti-APP (polyclone, AHP538; Serotec,Hercules, NC, USA; 1: 1 000; detect band β-CTF, see a previous sudy[14]) and rabbit anti-β-Tubulin (polyclone;Sigma; 1: 10 000; as inner control). The secondary antibody was goat anti-rabbit IgG/horseradish peroxidase (Bio-Rad, Hercules, CA, USA; 1: 10 000),enhanced chemiluminescence western blot kit (GE Inc,NJ, USA) was chromogenic. Western blot bands were measured with a Motic pathology picture HD analysis system (Motic, Xiamen, China) to analyze the average gray value. The average gray values of BACE-1 and β-CTF with β-Tubulin were compared, and the average relative value was obtained.
Aβ1-40 ELISA
A retinal Aβ1-40concentration assay was performed using a commercial Aβ1-40ELISA kit (Invitrogen, Carlsbad, CA,USA). The detailed processes were conducted according to the manual included in the kit. Positive control: the antibody tested in the kit was replaced by mouse anti-Aβ(monoclone, 4G8; Signet, Dedham, MA, USA; 1: 4 000).Equal quantities of protein (50 μg) were analyzed in every tested well. The final concentration was considered a pg/mg retina homogenate. All experiments were repeated at least twice.
Immunofluorescence staining
Retinal frozen sections were washed with 0.01 mol/L PBS three times for 5 minutes each and then enclosed in 10% bovine serum albumin-0.3 % Triton X-100 for 1 hour.
We added different primary antibodies (rabbit anti-BACE-1, polyclone, AB5940, Chemicon, Temecula,CA, USA, 1: 400; rabbit anti-GFAP, polyclone, 1: 1 000;mouse anti-synaptophysin, monoclone, Sigma, 1: 2 000),which were incubated in the refrigerator at 4°C overnight.The sections were washed in 0.01 mol/L PBS (3 × 15 minutes). Fluorescent secondary antibodies (Invitrogen;Alexa Fluor 568-donkey anti-rabbit; Alexa Fluor 568-donkey anti-mouse, 1: 200) were applied separately,with incubation at room temperature for 2 hours. Hoechst nuclear dye (Sigma) was applied to the sections, which were protected from light for 30 minutes, then washed with PBS three times for 15 minutes each time, before placement on glycerin-covered slides. Fluorescence sections were imaged using a 40 × objective lens with a fluorescence microscope (Olympus, Tokyo, Japan).
Statistical analysis
The data were analyzed using SPSS 10.0 (SPSS,Chicago, IL, USA). One-way analysis of variance was performed to test differences between group averages.All results were presented as mean ± SEM. A value of P < 0.05 was considered statistically significant.
Author contributions:This experiment was designed by Kun Xiong, performed by Jufang Huang, Kai Huang, Lei Shang and Xiaoxin Yan, and evaluated by Hui Wang.
Conflicts of interest:None declared.
Funding:This work was supported by the National Natural Science Foundation of China (The preliminary study of immature neurons in the adult guinea pigs neocortex layer II),No. 30900773; and the National University Basic Research Foundation of China (Dementia and glaucoma were characteristic of early diagnosis and outcome measure research), No. 2010QZZD022.
Ethical approval:This study was permitted by the Animal Ethics Committee of Xiangya School of Medicine, Central South University in China.
Supplementary information:Supplementary data associated with this article can be found, in the online version, by visiting www.nrronline.org, and entering Vol. 6, No. 14, 2011 after selecting the “NRR Current Issue” button on the page.
[1]Pizzol M, Thomsen M, Andersen MS. Long-term human exposure to lead from different media and intake pathways. Sci Total Environ. 2010;408(22):5478-5488.
[2]Schwartz BS, Stewart WF. Lead and cognitive function in adults: a questions and answers approach to a review of the evidence for cause, treatment, and prevention. Int Rev Psychiatry. 2007;19(6):671-692.
[3]Basha R, Reddy GR. Developmental exposure to lead and late life abnormalities of nervous system. Indian J Exp Biol. 2010;48(7):636-641.
[4]Zawia NH, Lahiri DK, Cardozo-Pelaez F. Epigenetics, oxidative stress, and Alzheimer disease. Free Radic Biol Med. 2009;46(9):1241-1249.
[5]Stewart WF, Schwartz BS. Effects of lead on the adult brain: a 15-year exploration. Am J Ind Med. 2007;50(10):729-739.
[6]Migliore L, Coppedè F. Genetics, environmental factors and the emerging role of epigenetics in neurodegenerative diseases.Mutat Res. 2009;667(1-2):82-97.
[7]Yun SW, Hoyer S. Effects of low-level lead on glycolytic enzymes and pyruvate dehydrogenase of rat brain in vitro: relevance to sporadic Alzheimer's disease? J Neural Transm. 2000;107(3):355-368.
[8]Blennow K, De Leon MJ, Zetterberg H. Alzheimer's disease.Lancet. 2006;368(9533):387-403.
[9]Tomiyama T. Involvement of beta-amyloid in the etiology of Alzheimer's disease. Brain Nerve. 2010;62(7):691-699.
[10]Basha MR, Murali M, Siddiqi HK, et al. Lead (Pb) exposure and its effect on APP proteolysis and Abeta aggregation. FASEB J.2005;19(14):2083-2084.
[11]Cole SL, Vassar R. The basic biology of BACE1: a key therapeutic target for Alzheimer's disease. Curr Genomics. 2007;8(8):509-530.
[12]Oliveira LT, Louzada PR, de Mello FG, et al. Amyloid-β decreases nitric oxide production in cultured retinal neurons: a possible mechanism for synaptic dysfunction in Alzheimer's disease?Neurochem Res. 2011;36(1):163-169.
[13]Greenberg BM, Frohman E. Optical coherence tomography as a potential readout in clinical trials. Ther Adv Neurol Disord. 2010;3(3):153-160.
[14]Xiong K, Clough RW, Struble RG, et al. Mitochondrial respiratory inhibition and oxidative stress elevate beta-secretase (BACE-1)proteins and activity in vivo in the rat retina. Exp Brain Res. 2007;181(3):435-446.
[15]Zhao J, Fu YF, Yasvoina M, et al. Beta-site amyloid precursor protein cleaving enzyme 1 levels become elevated in neurons around amyloid plaques: Implications for Alzheimer's disease pathogenesis. J Neurosci. 2007;27(14):3639-3649.
[16]Chen D, Wang H, Tong JB, et al. Expression of synaptophysin in rat retina following acute high intraocular pressure. Acta Academiae Medicinae Militaris Tertiae. 2008;30(11):1040-1042.
[17]Dowling JE. Retina. Shanghai: Shanghai Medical University Press. 1989.
[18]L?ffler KU, Edward DP, Tso MO. Immunoreactivity against tau,amyloid precursor protein, and beta-amyloid in the human retina. Invest Ophthalmol Vis Sci. 1995;36(1):24-31.
[19]Shimazawa M, Inokuchi Y, Okuno T, et al. Reduced retinal function in amyloid precursor protein-over-expressing transgenic mice via attenuating glutamate-N-methyl-d-aspartate receptor signaling. J Neurochem. 2008;107(1):279-290.
[20]Guo L, Duggan J, Cordeiro MF. Alzheimer's disease and retinal neurodegeneration. Curr Alzheimer Res. 2010;7(1):3-14.
[21]Lua Y, Lia Z, Zhang XQ, et al. Retinal nerve fiber layer structure abnormalities in early Alzheimer's disease: Evidence in optical coherence tomography. Neurosci Letters. 2010;480(1):69-72.
[22]Greenberg BM, Frohman E. Optical coherence tomography as a potential readout in clinical trials. Ther Adv Neurol Disord. 2010;3(3):153-160.
[23]Wei DL, Fu X, Jiang YM. Lead exposure and Alzheimer's disease.Gongye Weisheng yu Zhiyebing. 2006;32(6):379-382.
[24]Prince M. Is chronic low-level lead exposure in early life an etiologic factor in Alzheimer's disease? Epidemiology. 1998;9(6):618-621.
[25]Niklowitz WJ. Neurofibrillary changes after acute experimental lead poisoning. Neurology. 1975;25(10):927-934.
[26]Niklowitz WJ, Mandybur TI. Neurofibrillary changes following childhood lead encephalopathy. J Neuropathol Exp Neurol.1975;34(5):445-455.
[27]Tohda M, Suwanakitch P, Jeenapongsa R, et al. Expression changes of the mRNA of Alzheimer's disease related factors in the permanent ischemic rat brain. Biol Pharm Bull. 2004;27(12):2021-2023.
[28]Uryu K, Chen XH, Martinex D, et al. Multiple proteins implicated in neurodegenerative diseases accumulate in axons after brain trauma in humans. Exp Neurol. 2007;208(2):185-192.
[29]Yan XX, Xiong K, Struble RG, et al. β-secretase expression in normal and functionally deprived rat olfactory bulbs: inverse correlation with oxidative metabolic activity. J Comp Neurol.2007;501(1):52-69.
[30]Xie ZC, Dong YL, Maeda U, et al. The inhalation anesthetic isoflurane induces a vicious cycle of apoptosis and amyloid β-protein accumulation. J Neurosci. 2007;27(6):1247-1254.
[31]Yang F, Li JS, Yang F. The effect of different lead acetate concentration on rat primary culture cortical neurons. Zhonghua Laodong Weisheng Zhiyebing Zazhi. 2004;22(3):217-218.
[32]Neal AP, Guilarte TR. Molecular neurobiology of lead (Pb 2+):effects on synaptic function. Mol Neurobiol. 2010;42(3):151-160.
[33]Flora GJ, Seth PK. Alterations in some membrane properties in rat brain following exposure to lead. Cytobios. 2000;103(403):103-109.
[34]Curer H, Ercal N. Can antioxidants be beneficial in the treatment of lead poisoning. Free Radic Biol Med. 2000;29(10):927-945.
[35]He T, Hirsch HV, Ruden DM, et al. Chronic lead exposure alters presynaptic calcium regulation and synaptic facilitation in Drosophila larvae. Neurotoxicology. 2009;30(5):777-784.
[36]White LD, Cory-Slechta DA, Gilbert ME. New and evolving concepts in the neurotoxicology of lead. Toxicol Appl Pharmacol.2007;225(1):1-27.
[37]Wills NK, Ramanujam VM, Chang J, et al. Cadmium accumulation in the human retina: effects of age, gender, and cellular toxicity.Exp Eye Res. 2008;86(1):41-51.
[38]Liu WD, Li TX. Determination of blood lead with graphite furnace atomic absorption spectrometry. Zhongguo Zhiye Yixue. 2007;34(5):419,422.