Effect of sedation on short-term and long-term outcomes of critically ill patients with acute respiratory insuff ciency
Department of Intensive Care Unit, Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China
Effect of sedation on short-term and long-term outcomes of critically ill patients with acute respiratory insuff ciency
Xue-zhong Xing, Yong Gao, Hai-jun Wang, Shi-ning Qu, Chu-lin Huang, Hao Zhang, Hao Wang, Qing-ling Xiao, Ke-lin Sun
Department of Intensive Care Unit, Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China
BACKGROUND:The present study aimed to determine the short-term and long-term outcomes of critically ill patients with acute respiratory insuff ciency who had received sedation or no sedation.
METHODS:The data of 91 patients who had received mechanical ventilation in the first 24 hours between November 2008 and October 2009 were retrospectively analyzed. These patients were divided into two groups: a sedation group (n=28) and a non-sedation group (n=63). The patients were also grouped in two groups: deep sedation group and daily interruption and /or light sedation group.
RESULTS:Overall, the 91 patients who had received ventilation ≥48 hours were analyzed. Multivariate analysis demonstrated two independent risk factors for in-hospital death: sequential organ failure assessment score (P=0.019,RR1.355, 95%CI1.051–1.747,B=0.304,SE=0.130,Wald=50483) and sedation (P=0.041,RR5.015, 95%CI1.072–23.459,B=1.612,SE=0.787,Wald=4.195). Compared with the patients who had received no sedation, those who had received sedation had a longer duration of ventilation, a longer stay in intensive care unit and hospital, and an increased in-hospital mortality rate. The Kaplan-Meier method showed that patients who had received sedation had a lower 60-month survival rate than those who had received no sedation (76.7% vs. 88.9%, Log-rank test=3.630,P=0.057). Compared with the patients who had received deep sedation, those who had received daily interruption or light sedation showed a decreased in-hospital mortality rate (57.1% vs. 9.5%,P=0.008). The 60-month survival of the patients who had received deep sedation was signif cantly lower than that of those who had daily interruption or light sedation (38.1% vs. 90.5%, Log-rank test=6.783,P=0.009).
CONCLUSIONS:Sedation was associated with in-hospital death. The patients who had received sedation had a longer duration of ventilation, a longer stay in intensive care unit and in hospital, and an increased in-hospital mortality rate compared with the patients who did not receive sedation. Compared with daily interruption or light sedation, deep sedation increased the in-hospital mortality and decreased the 60-month survival for patients who had received sedation.
Sedation; Respiratory insuff ciency; Prognosis; Critical illness
INTRODUCTION
Acute respiratory insufficiency (ARI) occurs frequently after major operations with an incidence of 37.2%–57.0%.[1,2]Most of the patients with ARI received intubation although the rest survived with the help of noninvasive positive pressure ventilation.[3,4]But patients may suffer from discomfort and pain caused by endotracheal intubation. Pain and agitation can precipitate accidental removal of endotracheal tubes or intravascular catheters used for monitoring or administration of life-sustaining medications. Therefore, sedatives and analgesics are the most commonly used agents in the intensive care unit (ICU).[5]
Studies[6,7]showed that inappropriate sedation increased the duration of mechanical ventilation and the length of ICU stay. But few studies reported the different clinical outcomes between patients who received sedation and those who received no sedation.[8]Hence, the present study was undertaken to determine the short-term and long-term outcomes of patients who had received sedation or no sedation.
METHODS
Patients
This retrospective study was conducted at the Department of ICU of the Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, China, which is a 10-bed surgical unit. The definition of ARI was based on a previous study.[2]In the present study, 91 patients were divided into two groups: sedation group (n=28) and non-sedation group (n=63).
Methods
The following data of the patients who had received mechanical ventilation in the first 24 hours between November 2008 and October 2009 were retrospectively analyzed. The variables of the patients included age, gender, type of admission (elective or emergent), presence of sepsis, presence of acute kidney injury, presence of shock, presence of acute lung injury/acute respiratory distress syndrome (ALI/ARDS), acute physiology and chronic health evaluation II (APACHE II) score, and sequential organ failure assessment (SOFA). The duration of ventilation, length of ICU stay, ICU mortality, length of hospital stay, and hospital mortality were also collected. The patients who stayed in the ICU less than 48 hours were excluded from the study owing to early extubation and no sedation given after operative anesthesia.
Daily interruption of Kress et al[6]was performed by infusion of midazolam or propofol and morphine until the patients awoke and could follow instructions or they became uncomfortable or agitated and were deemed to require the resumption of sedation. Light sedation initiated by Treggiari et al[7]was performed for patients with a Ramsay level of 1 (awaking but tranquil and cooperative) or a Ramsay level of 2 (asleep but opening eyes to surroundings). Deep sedation referred to a Ramsay level of 3 or 4.[9]
Sepsis was def ned by the Chinese Society of Critical Care Medicine of the Chinese Medical Association as the presence of clinical signs of systemic inflammatory response syndrome (SIRS) associated with infection confirmed by culture. The SIRS was defined as the presence of two or more of the following variables: temperature greater than 38 °C or less than 35 °C, heart rate greater than 90 beats/minute, respiratory rate greater than 20 beats/minute or PaCO2less than 32 mmHg, white blood cell count greater than 12×109/ L or less than 4.0×109/L or relative count of immature cells greater than 10% of total leukocytes.[10]Shock was defined as mean blood pressure being less than 65 mmHg despite an adequate amount of fluids (at least 1 000 mL of crystalloids or 500 mL of colloids) had been administered.[11]Acute kidney injury was defined as an absolute increase of serum creatinine by ≥0.3 mg/ dL (≥26.4 μmol/L), an increase of serum creatinine by ≥50%, or a reduction of urine output, i.e. <0.5 mL/ kg per hour, for more than 6 hours.[12]ALI/ARDS was defined according to the 2006 guidelines for the diagnosis and treatment of ALI/ARDS by the Chinese Society of Critical Care Medicine of the Chinese Medical Association.[13]APACHE II was defined by several measurements (age, physiologic status and underlying health) as integer scores varying from 0 to 59, higher scores corresponding to more severe disease, and a higher risk of death.[14]SOFA score was based on six different scores, one each for the respiratory, cardiovascular, hepatic, coagulatory, renal and neurological systems, the extent of organ function or the rate of failure.[15]Overall survival was def ned as the time from the ICU admission to death from any cause during the follow up.
The institutional review board of the hospital approved the research, and informed consent was waived because of the observational nature of this study.
Statistical analysis
The SPSS software package 13.0 for Windows was used for statistical analysis. The data of the study were presented as mean±SD or median (25%–75% inter-quartile range) for continuous variables, and percentages for dichotomous variables. Continuous variables were analyzed using Student's t test, and categorical variables were analyzed using the Chi-square test. Univariate and multivariate analyses were performed to define the risk factors of in-hospital mortality. The survival was estimated by the Kaplan-Meier method, and compared using the Log-rank test. A P value<0.05 was considered statistically signif cant.
RESULTS
Of the 190 patients with ARI, 90 patients received ventilation for less than 48 hours, and 9 had no complete records, thus 91 patients were left for f nal analysis.
Univariate and multivariate analysis of risk factors of in-hospital death for patients receiving ventilation more than 48 hours
Univariate and multivariate analyses of the risk factors of in-hospital death were made in patients who had received ventilation more than 48 hours. Compared with patients who were alive, those who died in the hospital had more shocks, more episodes of sepsis, more organ failures as reflected from SOFA scores, more emergency admissions to the ICU, and sedation (Table 1).
Multivariate analysis demonstrated two independent risk factors for in-hospital death: SOFA score (P=0.019, RR 1.355, 95%CI 1.051–1.747, B=0.304, SE=0.130, Wald=50 483) and sedation (P=0.041, RR 5.015, 95%CI 1.072–23.459, B=1.612, SE=0.787, Wald=4.195) (Table 2).
Short-term and long-term outcomes of patients who received sedation or no sedationCompared with patients who had received no sedation, those who had received sedation experienced more episodes of sepsis, more emergency admissions to the ICU, a longer duration of ventilation, a longer length of ICU and hospital stay, and an increased in-hospital mortality rate (Table 3). The Kaplan-Meier methodshowed that the 60-month survival of the patients who had received sedation was lower than that of the patients who had received no sedation, although there was no signif cant difference between the two groups (76.7% vs. 88.9%, Log-rank test=3.630, P=0.057) (Figure 1).
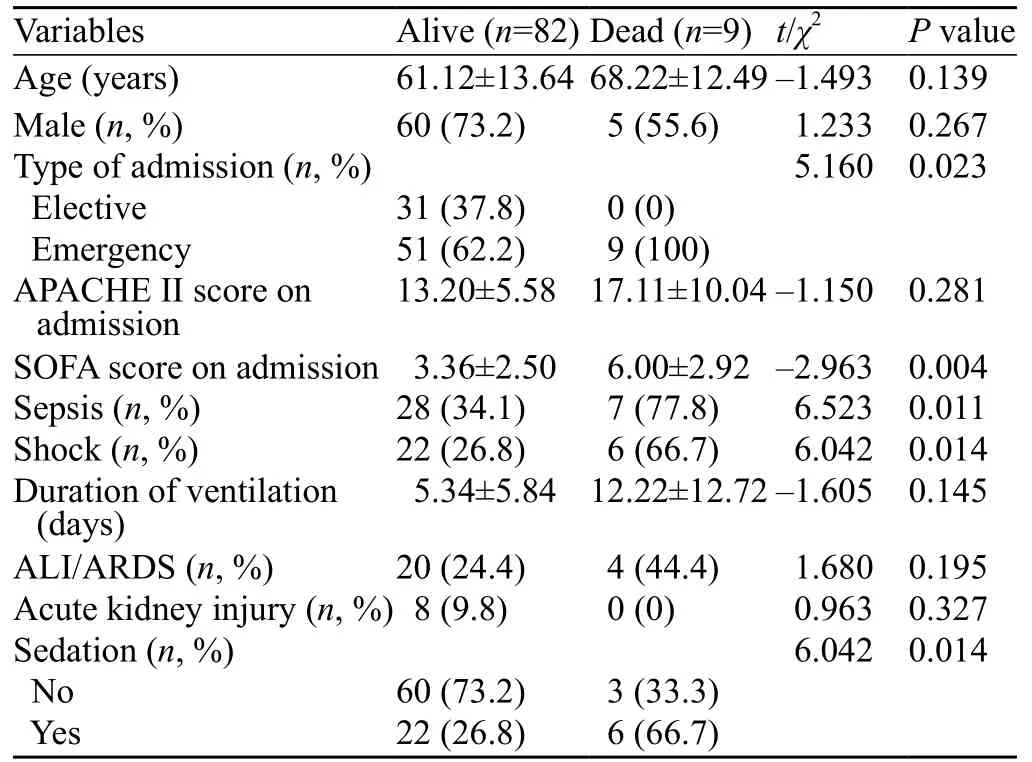
Table 1. Univariate analysis of risk factors of in-hospital death for patients receiving ventilation more than 48 hours
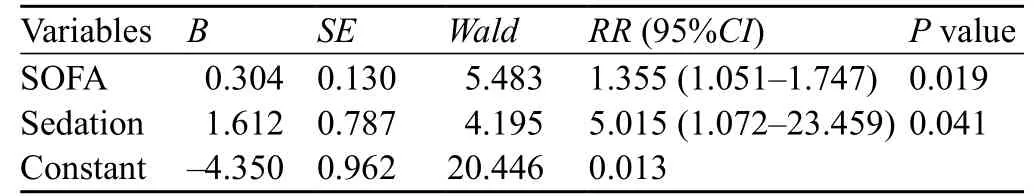
Table 2. Multivariate analysis of predictors of in-hospital death
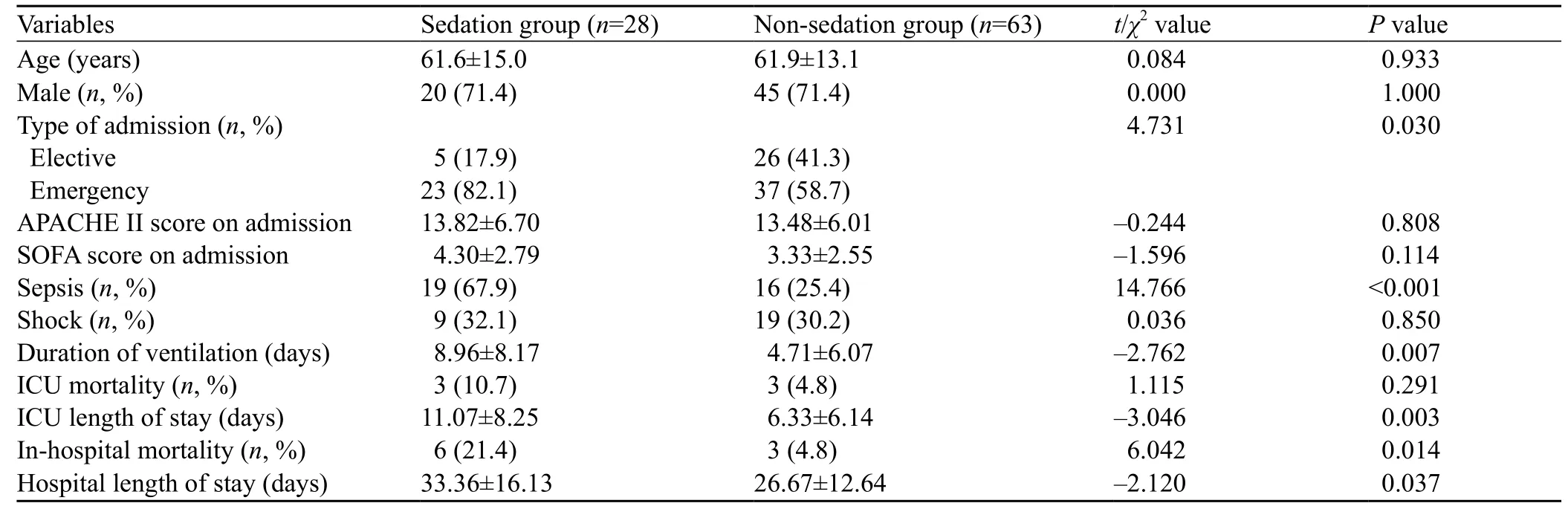
Table 3. Comparison of short-term outcome of patients who received sedation or not
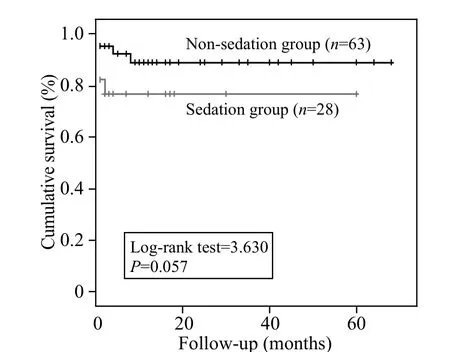
Figure 1. Long-term outcomes of patients who had received sedation or no sedation

Table 4. Short-term outcomes of patients who had received different type of sedation
Short-term and long-term outcomes of the patients who had received different types of sedations
Compared with the patients who had received deep sedation, patients who had received daily interruption or light sedation had a decreased in-hospital mortality rate (Table 4). The Kaplan-Meier method showed that the 60-month survival of the patients who had received deep sedation was significantly lower than that of the patients who had received daily interruption or light sedation (38.1% vs. 90.5%, Log-rank=6.783, P=0.009) (Figure 2).
DISCUSSION
In this study we found that sedation was a risk factor of in-hospital mortality. The patients who had received sedation had a longer duration of ventilation, a longer length of ICU and hospital stay and an increased inhospital mortality rate compared with those who did not receive any sedation. Compared with daily interruption or light sedation, deep sedation increased the in-hospital mortality rate, but decreased the 60-month survival rate.
Sedation was associated with the in-hospital mortality. Str?m et al[8]found that no sedation of critically ill patients who received mechanical ventilation was associated with significantly decreased ventilator-free days and non-significantly decreased ICU mortality rate. In their study, patients in the sedation group received morphine only, whereas those in the sedation group received both morphine and sedatives such as propofol and midazolam. Although morphine has a sedative effect and both groups received some sedation, use of morphine was very low in both groups with no signif cant difference. Therefore, use of morphine did not affect the result of the study. Severity scores both in their study and our study were not different between the two groups. Thus, other factors may account for the difference in the in-hospital mortality rate. More studies are needed to clarify the mechanisms between the association of sedation and the increased mortality rate.
Our study also showed that types of sedation affected on the short-term and long-term outcomes of patientswho had received ventilation. Kress et al[6]performed the first randomized trial comparing daily interruption with continuous infusion of sedatives. The study demonstrated that daily interruption of infusions of sedative drugs decreases the duration of mechanical ventilation and the length of ICU stay. Another randomized trial comparing light versus deep sedation also showed a decreased duration of mechanical ventilation and the short length of ICU stay.[7]However, a recent review found that daily interruption did not alter the duration of mechanical ventilation, mortality, length of ICU or hospital stay, adverse event rate, drug consumption, or quality of life for critically ill adults who received mechanical ventilation compared with those who had sedation without daily interruption.[16]There were no randomized controlled trials on the comparison between continuous infusion of sedatives and light sedation. Therefore, strong evidence of randomized controls comparing daily interruption with light sedation is needed to def ne which strategy is better.
The results of the present study demonstrated that deep sedation is associated with an increased hospital mortality rate and a decreased 6-month survival. In recent years, two multicenter prospective studies have shown that early deep sedation (def ned as deep sedation in the f rst 48 hours of ventilation) was a risk factor for delayed extubation and increased mortality.[17,18]Shehabi et al[17]studied 251 patients and found that early deep sedation was an independent predictor for extubation (HR=0.90; P<0.001), hospital death (HR=1.11; P=0.01), and 180-day mortality (HR=1.08; P=0.026). Another multicenter prospective study demonstrated that early deep sedation (OR=2.36; P=0.004) was associated with increased hospital mortality.[18]Literature review and our results showed that early intervention of sedation may be a target to improve the short-term and long-term outcomes of ventilated patients.
Our study has several limitations. First, this study is a single center study. Second, since the sample size was relatively small, the results of this study can not be generalized to other centers. Third, delirium was not studied.
In conclusion, we found that sedation was associated with in-hospital death. Patients who had received sedation had a longer duration of ventilation, a longer length of ICU and hospital stay, and an increased inhospital mortality rate compared with those who had not received sedation. Compared with daily interruption or light sedation, deep sedation increased in-hospital mortality and decreased 60-month survival for patients who had received sedation.
Funding:None.
Ethical approval:The ethical board of the hospital approved this study, and informed consent was waived because of the observational nature of the study.
Conflicts of interest:The authors declare that there are no conf icts of interest relevant to the content of the article.
Contributors:Xing XZ proposed the study, analyzed the data and wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts. The authors declare no conf icts of interest.
1 Franca SA, Toufen C Jr, Hovnanian AL, Albuquerque AL, Borges ER, Pizzo VR, et al. The epidemiology of acute respiratory failure in hospitalized patients: a Brazilian prospective cohort study. J Crit Care 2011; 26: 330.e1–8.
2 Xing XZ, Gao Y, Wang HJ, Yang QH, Huang CL, Qu SN, et al. Risk factors and prognosis of critically ill cancer patients with postoperative acute respiratory insufficiency. World J Emerg Med 2013; 4: 43–47.
3 Thille AW, Contou D, Fragnoli C, Córdoba-Izquierdo A, Boissier F, Brun-Buisson C. Non-invasive ventilation for acute hypoxemic respiratory failure: intubation rate and risk factors. Crit Care 2013; 17: R269.
4 Yu KY, Zhao L, Chen Z, Yang M. Noninvasive positive pressure ventilation for the treatment of acute respiratory distress syndrome following esophagectomy for esophageal cancer: a clinical comparative study. J Thorac Dis 2013; 5: 777–782.
5 Reade MC, Finfer S. Sedation and delirium in the intensive care unit. N Engl J Med 2014; 370: 444–454.
6 Kress JP, Pohlman AS, O'Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342: 1471–1477.
7 Treggiari MM, Romand JA, Yanez ND, Deem SA, Goldberg J, Hudson L, et al. Randomized trial of light versus deep sedation on mental health after critical illness. Crit Care Med 2009; 37: 2527–2534.
8 Str?m T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet 2010; 375: 475–480.
9 Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. BMJ 1974; 2: 656–659.
10 Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Def nitions Conference. Crit Care Med 2003; 31: 1250–1256.
11 Xing XZ, Wang HJ, Huang CL, Yang QH, Qu SN, Zhang H, et al. Prognosis of patients with shock receiving vasopressors. World J Emerg Med 2013; 4: 59–62.
12 Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 2007; 11:R31.
13 Chinese Society of Critical Care Medicine; Chinese Medical Association. Guidelines for management of acute lung injury/ acute respiratory distress syndrome: an evidence-based update by the Chinese Society of Critical Care Medicine (2006). Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2006; 18: 706–710. [Article inChinese]
14 Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985; 13: 818–829.
15 Vincent JL, Moreno R, Takala J, Willatts S, De Mendon?a A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996; 22: 707–710.
16 Burry L, Rose L, McCullagh IJ, Fergusson DA, Ferguson ND, Mehta S. Daily sedation interruption versus no daily sedation interruption for critically ill adult patients requiring invasivemechanical ventilation. Cochrane Database Syst Rev 2014; 7: CD009176.
17 Shehabi Y, Bellomo R, Reade MC, Bailey M, Bass F, Howe B, et al. Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med 2012; 186: 724–731.
18 Tanaka LM, Azevedo LC, Park M, Schettino G, Nassar AP, Réa-Neto A, et al. Early sedation and clinical outcomes of mechanically ventilated patients: a prospective multicenter cohort study. Crit Care 2014; 18: R156.
Received June 6, 2014
Accepted after revision December 22, 2014
Yong Gao, Email: 2354839907@qq.com
World J Emerg Med 2015;6(2):147–152
10.5847/wjem.j.1920–8642.2015.02.011
 World journal of emergency medicine2015年2期
World journal of emergency medicine2015年2期
- World journal of emergency medicine的其它文章
- Progress in research into the genes associated with venous thromboembolism
- Advances in clinical studies of cardiopulmonary resuscitation
- Instructions for Authors
- Thrombolysis during extended cardiopulmonary resuscitation for autoimmune-related pulmonary embolism
- Eff cacy of fascia iliaca compartment nerve block as part of multimodal analgesia after surgery for femoral bone fracture
- Noninvasive monitoring of intra-abdominal pressure by measuring abdominal wall tension
