Does the presence of a percutaneous renal access influence fluoroscopy time during percutaneous nephrolithotomy?
Yasser A.Noureldin,Mohamed A.Elkoushy, Sero Andonian*
aDivision of Urology,McGill University Health Centre,Montreal,Que′bec,Canada
bDepartment of Urology,Benha University Hospital,Benha University,Benha,Egypt
cDepartment of Urology,Suez Canal University,Ismailia,Egypt
Does the presence of a percutaneous renal access influence fluoroscopy time during percutaneous nephrolithotomy?
Yasser A.Noureldina,b,Mohamed A.Elkoushya,c, Sero Andoniana,*
aDivision of Urology,McGill University Health Centre,Montreal,Que′bec,Canada
bDepartment of Urology,Benha University Hospital,Benha University,Benha,Egypt
cDepartment of Urology,Suez Canal University,Ismailia,Egypt
Fluoroscopy;
Objective:The aim of this study was to assess whether the presence of a preformed percutaneous renal access(PCA)had any effects on fluoroscopy time(FT)during percutaneous nephrolithotomy(PCNL).
Methods:After ethics approval was obtained,medical records of all patients who underwent PCNL between 2009 and 2013 at a tertiary stone referral centre were retrospectively reviewed. Patients with and without pre-formed PCA undergoing PCNL were compared.Patients who underwent second-look PCNL and those who had their access inserted by interventional radiology constituted the group with pre-formed PCA.
Results:A total of 185 PCNLs were reviewed.The mean patient age was 55.2±1.0 years with mean body mass index(BMI)of 27.8±0.5 kg/m2and male gender of 63.8%.The mean stone size was 618.4±47.0 mm2with mean Guy’s grade of 2.3±0.7 and mean S.T.O.N.E.score of 7.6±0.1.The mean operative time was 98.7±2.6 min with mean FT of 113.4±4.5 s.The overall stone-free rate was 71.9%with complication rate of 16.2%.When compared with PCNLs without pre-formed PCA,PCNLs with pre-formed PCA were associated with significantly shorter FT(120.6±5.1 vs.77.5±6.7 s;p<0.001)and significantly lower estimated blood loss(EBL) (p=0.01).On multivariate analysis,PCNLs with pre-formed PCA were associated with significantly shorter FT(B.coefficient=-43.2(95%CI:-66.4 to-20);p<0.001)and lower EBL (p=0.02).
Conclusion:PCNLs with pre-formed PCA were associated with significantly lower FT and EBL when compared with PCNLs without pre-formed PCA.
?2015 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier (Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
1.Introduction
According to the latest American Urological Association guidelines on staghorn stones,fluoroscopically-guided percutaneous nephrolithotomy(PCNL)is still the cornerstone of treatment of large renal stones[1].However,it is associated with the highest radiation exposure compared with other endourological procedures[2,3].Although ionizing radiation offers advantages over other imaging modalities,patients and medical personnel may be exposed to significant levels of radiation.Some authors have even reported potential oncologic consequences from exposure to excessive ionizing radiation[4-6].Thus,the need for following radiation safety measures including minimizing amount of fluoroscopy during PCNL and wearing appropriate radiation protective gear[3,7].
Several studies have already determined factors associated with increased radiation exposure during PCNL[8-10]. However,there is a paucity of literature regarding the effect of presence or absence of percutaneous renal access (PCA)on fluoroscopy time during PCNL.Therefore,the aim of this study was to assess whether PCNLs with pre-formed PCA are associated with significantly shorter fluoroscopy time(FT)when compared with PCNLs without pre-formed PCA.
2.Patients and methods
2.1.Study design
This study was conducted in concordance with the declaration of Helsinki 2013 and after approvals from the Director of Professional Services and Ethics Board of McGill University Health Centre(No.14-050-GEN)were obtained. A retrospective review of all consecutive PCNLs between 2009 and 2013 was performed.Both Guy’s and S.T.O.N.E. nephrolithometry scores were calculated.All PCNLs were performed by a single fellowship-trained endourologist(SA) under general anesthesia.Except for seven PCNLs performed in the supine position,all PCNLs were performed in the prone position according to what has been previously published[11,12].At the end of the procedure,an antegrade indwelling 6F double-pigtail ureteral stent was inserted.In addition,a 20F council-tip Foley catheter was used as a nephrostomy tube for standard PCNL cases.For tubeless PCNL cases,the skin was closed with 4-0 absorbable suture.Immediately post-operatively,the attending endourologist filled out PCNL datasheets containing patients’pre-operative information and intra-operative procedural details.All of the PCNL datasheets and patients’medical charts were reviewed.Patients were followed up with plain radiographs(kidney-ureter-bladder)at 1 and 3 months.Non-contrast computed tomography(NCCT)scans were obtained for patients with radiolucent stones.Stonefree was considered in cases with absence of any stones or presence of clinically insignificant residual fragments (<4 mm)at follow-up.The intra-operative estimated blood loss(EBL)was categorized as<250 mL or≥250 mL.FT was calculated from the beginning till the end of the case including cystoscopy and retrograde pyelography.The calculation method for the FT has been previously reported [10].Post-operative complications were reported according to the modified Clavien classification system[13].PCNLs were categorized into two groups according to the presence or absence of pre-formed PCA.Therefore,the first group included PCNLs without pre-formed PCA,where the PCA was performed using fluoroscopic-guidance by the attending endourologist at the time of PCNL.The second group included PCNLs with pre-formed PCA,where the PCA had been inserted prior to the PCNL during either a previous PCNL procedure for patients undergoing second-look PCNLs or the PCA was inserted by an interventional radiologist(IR) under ultrasound-or CT-guidance.There were several indications for patients having their PCA by an IR prior to PCNL.These indications included patients with:renal transplant stones;severe scoliosis;ankylosing spondylitis; encrusted indwelling ureteral stents with renal,ureteral and bladder stones;quadriplegia and spinal fixation with metal rods overlying the kidneys;urinary diversions;pelvic kidneys;and patients with retro-renal colons.
2.2.Statistical analysis
Both groups were compared in terms of baseline demographics and peri-operative outcomes.FT and continuous variables were compared between the two groups using the Mann Whitney-U test.Categorical variables were compared using Fisher’s exact test or Chi-square test.Two tailed p-values<0.05 were considered statistically signif icant.Multivariate logistic regression analysis and general linear models were performed to estimate the effect size and correct for any possible confounders.SPSS for Windows version 20(SPSS Inc.,Chicago,IL,USA)was used for statistical analysis.
3.Results
A total of 185 PCNLs were identified and reviewed.The mean patient age was 55.2±1.0 years with a mean body mass index(BMI)of 27.8±0.5 kg/m2and male gender of 63.8%(118/185).The mean stone size was 618.4±47.0 mm2with mean Guy’s grade of 2.3±0.7 andmean S.T.O.N.E.score of 7.6±0.1.The mean operative time was 98.7±2.6 min with mean FT of 113.4±4.5 s.The overall stone-free rate was 71.9%(133/185)with complication rate of 16.2%(30/185).According to the modified Clavien classification,complications are reported as follows:Grade 1:6(3.2%);Grade 2:9(4.9%);Grade 3a:2 (1.1%);Grade 3b:11(5.9%);and Grade 4b:1(0.5%).There were no Grade 4a or Grade 5 complications.EBL of≥250 mL occurred in 53(28.6%)PCNLs.Tubeless PCNL was performed in 47.0%(87/185)of PCNLs.The mean length of hospital stay(LOS)was 4.09±0.2 days.
When compared with PCNLs without pre-formed PCA, PCNLs with pre-formed PCA were completed with signif icantly shorter FT(120.6±5.1 vs.77.5±6.7 s;p<0.001) and there were significantly less patients with EBL of≥250 mL(50(32.3%)vs.3(10.0%);p=0.01)(Table 1). However,there was no significant difference between the two groups in terms of patient age(56.3±2.6 vs. 55.0±1.2 years;p=0.74),female gender(12(40.0%)vs. 55(35.0%);p=0.68),BMI(29.8±1.5 vs.27.4±0.5 kg/m2; p=0.16),stone size(662±149 vs.610±48 mm2; p=0.58),right-sided stones(15(50.0%)vs.66(42.6%); p=0.55),mean Guy’s grade(2.1±0.2 vs.2.3±0.1; p=0.58),mean S.T.O.N.E.score(7.5±0.3 vs.7.7±0.1; p=0.62),operative time(92.0±5.9 vs.100.1±2.3 min; p=0.25),stone-free status(22(73.3%)vs.111(71.6%); p=0.99)and post-operative complications(6(20.0%)vs. 24(15.5%);p=0.59)(Table 1).In addition,there was no significant difference between tubeless and standard PCNLs in terms of FT(120.3±7.4 vs.107.7±5.5 s;p=0.17).On multivariate analysis,PCNLs with pre-formed PCA were associated with significantly shorter FT(B. coefficient=-43.2(95%CI:-66.4 to-20);p<0.001)and significantly lower risk of having EBL of≥250 mL(OR=0.2 (95%CI:0.07 to 0.8);p=0.02).
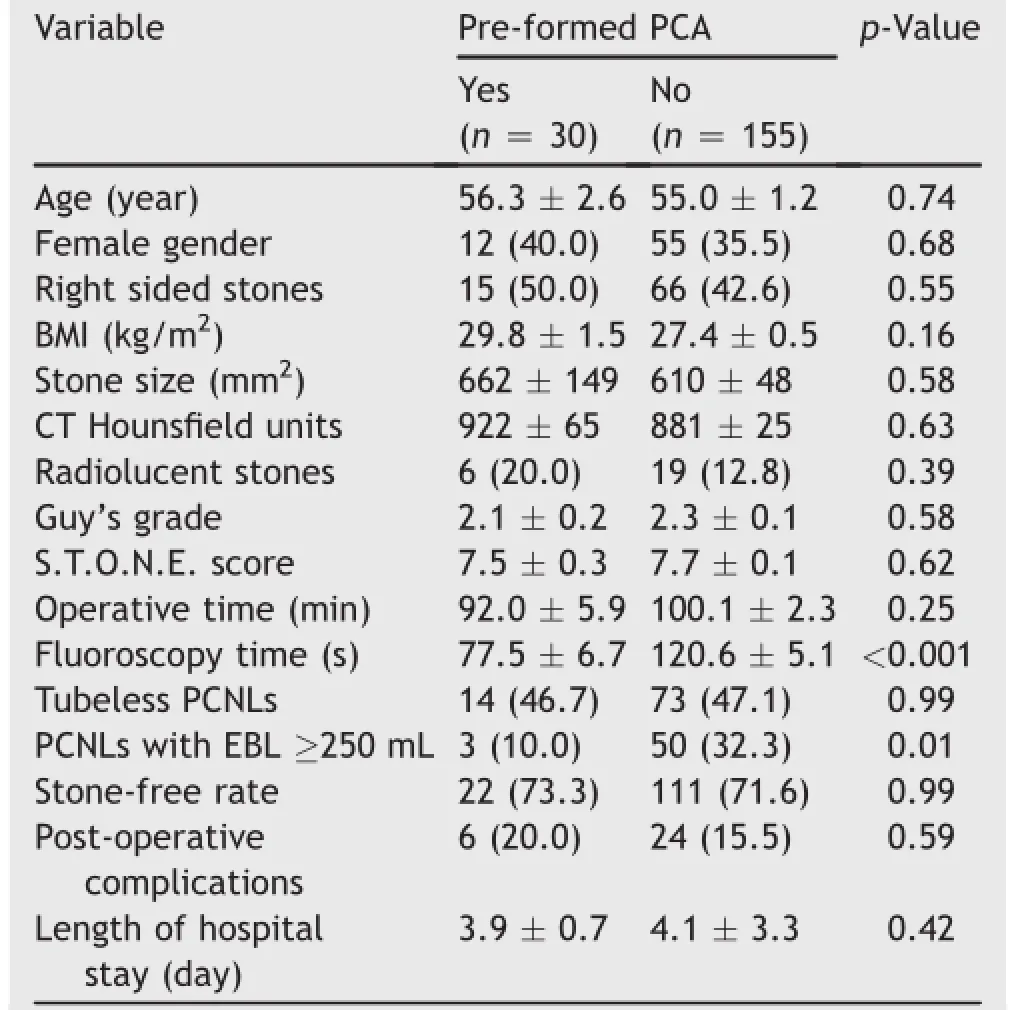
Table 1Comparison of baseline demographic characteristics and peri-operative outcomes between the two groups.
4.Discussion
In the current study,when compared with PCNLs without pre-formed PCA,PCNLs with pre-formed PCA were associated with significantly shorter FT(120.6±5.1 vs. 77.5±6.7 s;p<0.001)and there were significantly less patients with EBL of≥250 mL(50(32.3%)vs.3(10.0%); p=0.01).Although this may seem obvious,this study is the first to document the effect of pre-formed PCA being associated with significantly less fluoroscopy and thus radiation when performing fluoroscopically-guided PCA during PCNL.While previous studies have looked at several determinants of FT during PCNL,the presence or absence of a PCA has not been previously examined.For example, increased stone burden and multiple access tracts have been associated with significantly prolonged FT while elevated BMI,increased stone burden and multiple access tracts have been associated with significantly higher effective radiation doses[8,9].Furthermore,a recent study by Noureldin et al.[10]found that operative time,EBL and number of punctures were the only predictors of FT during PCNL on multivariate analysis.However,the effect of preformed PCA on FT was not studied.Since in the present study patients with pre-formed PCA were compared with patients without pre-formed PCA,it was not logical to compare the number of punctures between the two groups; the group with pre-formed PCA would have zero punctures. Therefore,the two other predictors of PCA,namely operative time and EBL,were examined.While there was no significant difference between the two groups in operative time,patients with pre-formed PCA were associated with significantly less EBL(Table 1).Others have concentrated their efforts of minimizing FT using the different functions of the C-arm fluoroscopy unit.For example,it has been reported that by using pulsed fluoroscopy at 4 frames per second was associated with 65%decrease in FT during PCNLs(341.1 vs.121.5 s;p=0.001)when compared with PCNLs performed using standard fluoroscopy at 30 frames per second[14].In the present study,all PCNL cases since November 2010 were performed using pulsed fluoroscopy to minimize FT.Another group of investigators have further adjusted the settings of the C-arm unit to further reduce FT during PCNLs.Using visual and tactile cues,fixed lower mAs and kVp,a designated fluoroscopy technician on a laserguided C-arm,and pulsed fluoroscopy at 1 frame per second was associated with 80.9%reduction in FT during PCNLs (175.6 vs.33.7 s;p<0.001)[15].Finally,endoscopicguided PCA has been recently described to be associated with significantly lower FT during PCNL[16,17].
The second finding of the current study was that PCNLs with pre-formed PCA were associated with significantly less patients with EBL of≥250 mL.This is consistent with the findings of the study by Kukreja et al.[18],where they found that EBL was significantly lower in patients with mature nephrostomy tracts.
Limitations of the present study could be addressed as follows.First,the retrospective nature is a point of weakness.However,FT for every PCNL was collected prospectively and documented in PCNL datasheets immediately post-operatively by the attending endourologist.Second, FT during the PCA portion of PCNL was not specifically marked on the datasheets.Third,the EBL was estimated as a categorical variable<250 mL vs.≥250 mL.Nevertheless, this is the first study to report the size effect of a preformed PCA on both FT and EBL during PCNL.
5.Conclusion
PCNLs with pre-formed PCA were associated with signif icantly lower FT and EBL when compared with PCNLs without pre-formed PCA.This highlights the significant impact of the presence of a PCA on both FT and EBL.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
This work was partially sponsored by Fonds de la Recherche Sante′du Que′bec(FRSQ)Chercheur Boursier grant to Dr Sero Andonian and by a grant from the Urology Care Foundation Research Scholars Program and the Boston Scientific Corporation,The Endourological Society,and the“Friends of Joe”to Dr Yasser Noureldin and the CUASF-SIU International Scholarship grant to Dr Yasser Noureldin.
[1]Preminger GM,Assimos DG,Lingeman JE,Nakada SY, Pearle MS,Wolf Jr JS,AUA Nephrolithiasis Guideline Panel. Chapter 1:AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations.J Urol 2005;173: 1991-2000.
[2]Hellawell GO,Mutch SJ,Thevendran G,Wells E,Morgan RJ. Radiation exposure and the urologist:what are the risks?J Urol 2005;174:948-52.
[3]Andonian S,Atalla MA.Radiation safety in urology.AUA update series,vol.28;2009.lesson 26.
[4]Pierce DA,Preston DL.Radiation-related cancer risks at low doses among atomic bomb survivors.Radiat Res 2000;154: 178-86.
[5]Brenner DJ,Hall EJ.Computed tomography-an increasing source of radiation exposure.N Engl J Med 2007;357: 2277-84.
[6]Choi KH,Ha M,Lee WJ,Hwang SS,Jeong M,Jin YW,et al. Cancer risk in diagnostic radiation workers in Korea from 1996-2002.Int J Environ Res Public Health 2013;10:314-27.
[7]Elkoushy MA,Andonian S.Prevalence of orthopedic complaints among endourologists and their compliance with radiation safety measures.J Endourol 2011;25:1609-13.
[8]Tepeler A,Binbay M,Yuruk E,Sari E,Kaba M, Muslumanoglu AY,et al.Factors affecting the fluoroscopic screening time during percutaneous nephrolithotomy.J Endourol 2009;23:1825-9.
[9]Mancini JG,Raymundo EM,Lipkin M,Zilberman D,Yong D, Ban?ez LL,et al.Factors affecting patient radiation exposure during percutaneous nephrolithotomy.J Urol 2010;184: 2373-7.
[10]Noureldin YA,Elkoushy MA,Andonian S.Predictors of fluoroscopy time during percutaneous nephrolithotomy:impact of postgraduate urology trainees and S.T.O.N.E.nephrolithometry score.J Endourol 2015;29:542-7.
[11]Shahrour W,Andonian S.Ambulatory percutaneous nephrolithotomy:initial series.Urology 2010;76:1288-92.
[12]Noureldin YA,Elkoushy MA,Andonian S.Which is better?Guy’s versus S.T.O.N.E.nephrolithometry scoring systems in predicting stone-free status post-percutaneous nephrolithotomy. World J Urol 2015 Feb 13[Epub ahead of print].
[13]de la Rosette JJ,Opondo D,Daels FP,Giusti G,Serrano A, Kandasami SV,et al.,CROES PCNL Study Group.Categorization of complications and validation of the Clavien score for percutaneous nephrolithotomy.Eur Urol 2012;62:246-55.
[14]Elkoushy MA,Shahrour W,Andonian S.Pulsed fluoroscopy in ureteroscopy and percutaneous nephrolithotomy.Urology 2012;79:1230-5.
[15]Blair B,Huang G,Arnold D,Li R,Schlaifer A,Anderson K,et al. Reduced fluoroscopy protocol for percutaneous nephrostolithotomy:feasibility,outcomes and effects on fluoroscopy time.J Urol 2013;190:2112-6.
[16]Isac W,Rizkala E,Liu X,Noble M,Monga M.Endoscopic-guided versus fluoroscopic-guided renal access for percutaneous nephrolithotomy:a comparative analysis.Urology 2013;81: 251-6.
[17]Lantz AG,O’Malley P,Ordon M,Jason Y,Lee JY.Assessing radiation exposure during endoscopic-guided percutaneous nephrolithotomy.Can Urol Assoc J 2014;8:347-51.
[18]Kukreja R,Desai M,Patel S,Bapat S,Desai M.Factors affecting blood loss during percutaneous nephrolithotomy: prospective study.J Endourol 2004;18:715-22.
Received 7 April 2015;received in revised form 2 August 2015;accepted 4 August 2015 Available online 18 August 2015
*Corresponding author.
E-mail address:sero.andonian@muhc.mcgill.ca(S.Andonian).
Peer review under responsibility of Shanghai Medical Association and SMMU.
http://dx.doi.org/10.1016/j.ajur.2015.08.001
2214-3882/?2015 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier(Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Percutaneous
nephrolithotomy;
Renal access
 Asian Journal of Urology2015年4期
Asian Journal of Urology2015年4期
- Asian Journal of Urology的其它文章
- GUIDE FOR AUTHORS
- Ureteral stent technology:Drug-eluting stents and stent coatings
- Stellate scar sign of renal cell carcinoma
- Laparoscopic ureterolysis with simultaneous ureteroscopy and percutaneous nephroscopy for treating complex ureteral obstruction after failed endoscopic intervention:A technical report
- Implication of ultrasound bladder parameters on treatment response in patients with benign prostatic hyperplasia under medical management
- Prostate chronic inflammation type IV and prostate cancer risk in patients undergoing first biopsy set:Results of a large cohort study
