Clinical effect observation on acupuncture for chronic obstructive pulmonary disease
Liu Lu-jiong (劉魯炯), Shi Miao-yan (史苗顏), Song Xiu-ming (宋秀明), Zhang Wei (張煒), Jiang Chun-juan (江淳涓)
Pulmonary Disease Department, Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
Clinical Study
Clinical effect observation on acupuncture for chronic obstructive pulmonary disease
Liu Lu-jiong (劉魯炯), Shi Miao-yan (史苗顏), Song Xiu-ming (宋秀明), Zhang Wei (張煒), Jiang Chun-juan (江淳涓)
Pulmonary Disease Department, Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
Objective:To observe the clinical effect of acupuncture on chronic obstructive pulmonary disease (COPD), and the improvements of patients’ pulmonary ventilation function and 6-minute walk test (6-MWT) distance.
Acupuncture Therapy; Pulmonary Disease, Chronic Obstructive; Respiratory Function Tests; Heart Function Tests
Chronic obstructive pulmonary disease (COPD) is a lung condition characterized by persistent progressive airflow limitation and lung function decline. It’s often associated with excessive inflammatory reaction of the airway and lung to harmful dust and gas. The COPD incidence is increasing and currently the fourth leading cause of death worldwide. In China, COPD affects 8.2% population above the age of 40, more men (12.4%) than women (5.1%)[1]. It’s estimated by the World Health Organization (WHO) that it’s likely to become the third leading cause of death worldwide in 2020[2].
At present, COPD treatment is based on overall evaluation on the patients’ symptoms, airflow limitation severity (pulmonary function test), acute exacerbation risk and complication[3]. We’ve treated patients with COPD due to qi deficiency of the lung and kidney with Salmeterol Xinafoate and Fluticasone Propionate powder (Seretide) inhaler and acupuncture. The results are now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Chinese medicine
This was based on theTraditional Chinese medicine Diagnostic and Therapeutic Protocols for 105 Diseases in 24 Disciplines[4]andCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[5]. Qi deficiency of the lung and kidney: coughing, dyspnea, wheezing, shortness of breath that aggravate upon physical exertion; fatigue or spontaneous sweating that aggravates upon physical exertion; susceptible to common cold, intolerance of wind; low back and knee soreness and weakness; tinnitus, dizziness or facial puffiness; a swollen tongue with teeth marks and a thin white or greasy coating and a deep thready or deep moderate or thready weak pulse. A diagnosis can be made in patients with 2 of the first 3 symptoms and 2 of the last 3 signs.
1.1.2 Diagnostic criteria in Western medicine
This was based on the COPD diagnosis and staging criteria stipulated in theCOPD Diagnosis and Treatment Guidelines[6]and theGlobal Initiative for Chronic Obstructive Lung Disease (GOLD): Global Strategy for Diagnosis, Management and Prevention of COPD(2015 revised edition)[7].
Diagnostic criteria: Clinical manifestations include difficulty breathing, chronic coughing and chronic phlegm expectoration that may exacerbate. Pulmonary function test showed the forced expiratory volume in 1 second to forced vital capacity ratio (FEV1/FVC) <0.70 upon inhalation of bronchodilator, which indicates persistent airflow limitation.
The COPD airflow limitation severity was graded according to the forced expiratory volume in 1 second percentage of predicted value (FEV1%) and FEV1/FVC (Table 1).
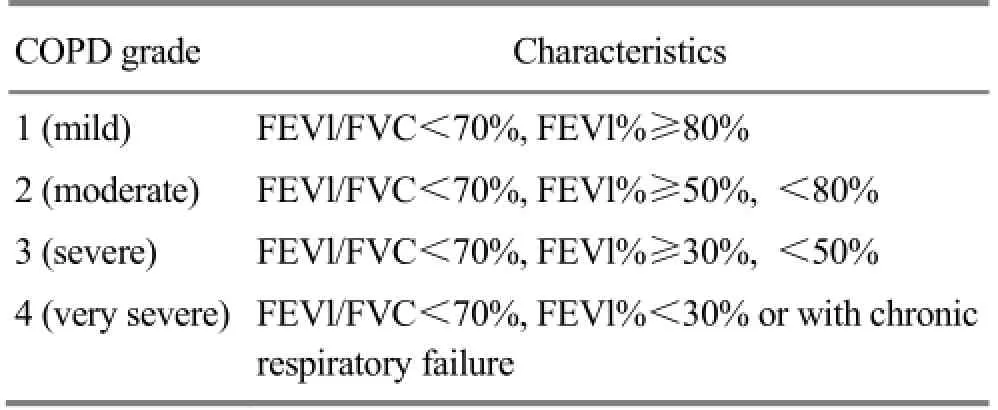
Table 1. GOLD staging for COPD (based on FEV1 value)
The score on difficulty breathing was measured using the modified Medical Research Council scale (mMRC)[8]. The COPD assessment test (CAT) was used to assess the patients’ quality of life[9-10]. The total scores of CAT range from 0 to 40, higher score indicating more severe health status impairment or a poorer control of COPD. Risk assessment was based on GOLD staging or exacerbation frequencies (Table 2).
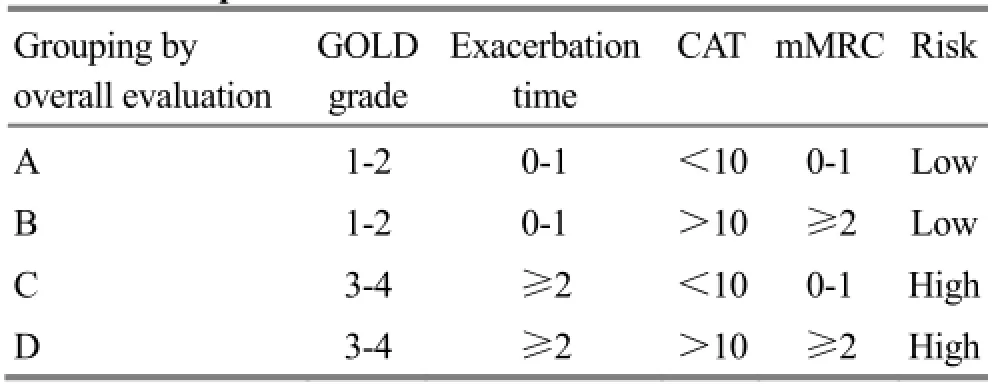
Table 2. Comprehensive evaluation of COPD
1.2 Inclusion criteria
Those who met the diagnosis criteria for COPD; having been diagnosed as qi deficiency of the lung and kidney; having GOLD grade 3-4 of pulmonary function; group C or D by overall evaluation of COPD; agreed to accept and cooperate during the treatment and signed the informed consent.
1.3 Exclusion criteria
Those who didn’t meet the above diagnostic criteria in Chinese and Western medicine and inclusion criteria; having persistent or critical COPD; having severe complications of cardiac dysfunction; having severe complications of cardiovascular, liver, kidney and hemopoietic systems; having mental disorders; pregnant or breast-feeding women; having allergic reactions to this therapy; and those who failed to follow the treatment protocol or having incomplete data.
1.4 Statistical method
The Windows Excel software was used for experimental data sheet. The SPSS 17.0 version software was used for statistical analysis. Thewas used to express normally distributed numerical variables, whereas median and interquartile ranges were used to express skew distribution. Two independent-samplest-test were used to compare normally distributed before-after differences, whereas rank sum test was used for inter-group comparison. All hypothesis tests employedα=0.05 and aPvalue of less than 0.05 indicated a statistical significance.
1.5 Bias control
Study objects were screened by inclusion and exclusion criteria during design and on-site investigation. The on-site investigation employed a uniform format and face-to-face interview. In addition, the data were double checked to make sure they are accurate.
1.6 General data
A total of 80 COPD outpatients treated between January 2013 and December 2014 were randomly allocated into a treatment group (n=40) and a control group (n=40). There were no between-group statistical differences in gender, age, disease severity and total scores of signs & symptoms (allP>0.05), indicating that the two groups are comparable (Table 3).
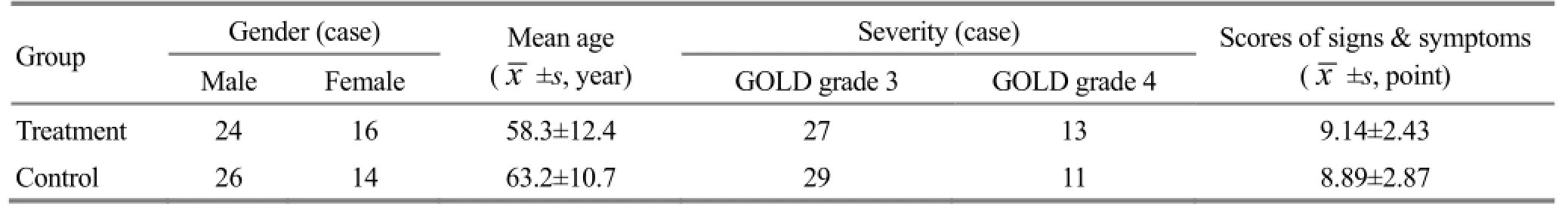
Table 3. Between-group comparison on baseline data
2 Treatment Methods
2.1 Treatment group
2.1.1 Western medicine
Seretide inhaler (Glaxo Operations UK Ltd., Batch No R632239), 50 μg/250 μg for each dose, two doses a day (once in the morning and once in the evening), for 3 months.
2.1.2 Acupuncture
Points: Feishu (BL 13), Shenshu (BL 23), Qihai (CV 6), Guanyuan (CV 4), Dingchuan (EX-B 1), Danzhong (CV 17), and Zusanli (ST 36).
Method: Disposable filiform needles of 0.25 mm in diameter and 40 mm in length were used to puncture patients in a supine lying position. Qihai (CV 6) and Guanyuan (CV 4) were punctured 1.0-1.3 cun perpendicularly, followed by even reinforcing-reducing manipulation upon arrival of qi. The needles were removed after 10 min. Then the patient was asked to sit and bend the head. Feishu (BL 13), Shenshu (BL 23), Dingchuan (EX-B 1), Danzhong (CV 17) and Zusanli (ST 36) were punctured. Feishu (BL 13) was punctured 0.5-0.8 cun obliquely toward the spine; Shenshu (BL 23) was punctured 0.5-1 cun perpendicularly; Dingchuan (EX-B 1) was punctured 0.5-1 cun obliquely toward the spine; Danzhong (CV 17) was punctured 0.5-0.8 cun subcutaneously; and Zusanli (ST 36) was punctured 1-1.3 cun perpendicularly. Even reinforcing-reducing manipulation was applied upon arrival of qi. The needles were retained for 10 min. The treatment was done twice a week for a total of 3 months.
2.2 Control group
The same Western medicine (same method, dose, and course of treatment) as the treatment group was used for patients in the control group.
3 Therapeutic Efficacy Observation
3.1 Observation indices
3.1.1 Clinical signs and symptoms
Scores and total scores of clinical signs and symptoms (coughing, phlegm, dyspnea, wheezing and shortness of breath) in both groups were recorded before and after treatment. Then the signs and symptoms were graded as four levels based upon theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[5]: absent (0 point), mild (1 point), moderate (2 points) and severe (3 points). The therapeutic efficacy indices and total scores were calculated according to scores of each sign and symptom (Table 4).
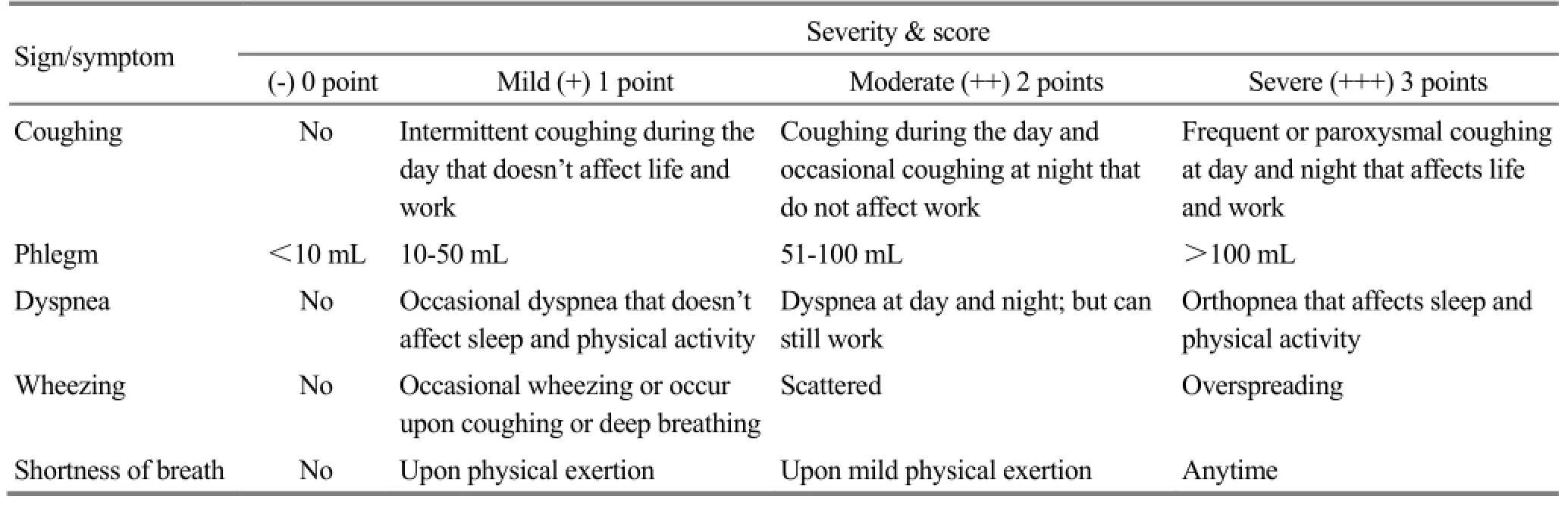
Table 4.Scoring criteria for clinical signs and symptoms
3.1.2 6-minute walk test (6-MWT)
Method: To paint a 30-meter straight line distance on a flat, hard road surface and place two chairs on both ends; then ask the patient to walk and return as fast as possible. The examiner reported every 2 min and monitored the patients’ discomfort (shortness of breath, chest tightness or chest pain). Patients can pause or stop the test in case they cannot carry on. Their walk distances were calculated after 6 min.
3.1.3 Pulmonary ventilation function test
It’s of great significance to test pulmonary ventilation function for COPD diagnosis and treatment. Pulmonary ventilation function is considered the gold standard in tracing the COPD development, evaluating the COPD severity and monitoring COPD progression[11]. FEV1% and FEV1/FVC% were used as two main indices in this study.
3.2 Therapeutic efficacy criteria
Based upon theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[5], the therapeutic efficacy indices were calculated using the Nimodipine method according to signs and symptoms. Then the efficacy was evaluated by the efficacy indices.
Therapeutic efficacy index = (Before treatment score - After treatment score) ÷ Before treatment score × 100%.
Clinical recovery: Therapeutic efficacy index ≥95%.
Marked effect: Therapeutic efficacy index ≥70% but<95%.
Improvement: Therapeutic efficacy index ≥30% but<70%.
Failure: Therapeutic efficacy index <30%.
3.3 Treatment results
3.3.1 Overall efficacy evaluation in two groups
A total of 80 patients in two groups completed the treatment. After 3 months of treatment, the total effective rate in the treatment group was 95%, versus 80% in the control group, showing a statistical significance (P<0.05) and indicating a better effect in the treatment group than that in the control group (Table 5).
3.3.2 Between-group comparison on signs and symptoms of traditional Chinese medicine (TCM)
After treatment, the total scores of TCM signs and symptoms including coughing, phlegm, dyspnea, wheezing and shortness of breath were both significantly improved in both groups (P<0.05,P<0.01). However, the scores in each item were more significantly reduced in the treatment group than those in the control group (P<0.05,P<0.01), indicating that both treatment protocols can improve clinical symptoms in COPD patients; however, Seretide inhaler combined with acupuncture showed better results in alleviating phlegm, dyspnea and shortness of breath than Seretide alone (Table 6).

Table 5.Between-group comparison of therapeutic efficacy (case)
Table 6. Between-group comparison of TCM signs and symptoms before and after treatment (point)
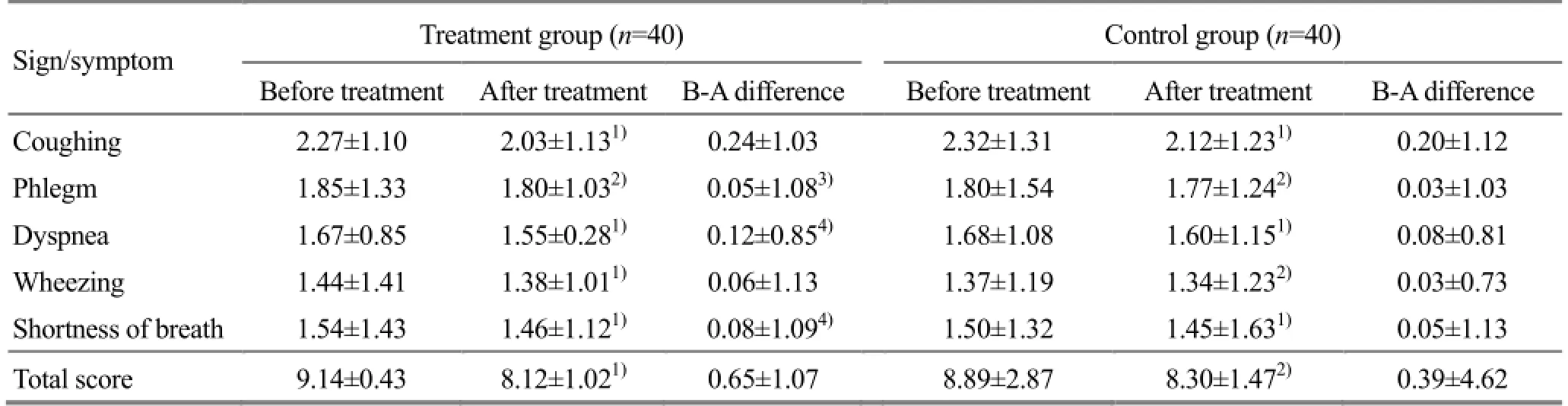
Table 6. Between-group comparison of TCM signs and symptoms before and after treatment (point)
Note: B-A=Before-after; intra-group comparison before and after treatment, 1) P<0.01, 2) P<0.05; compared with the control group, 3) P<0.01, 4) P<0.05
3.3.3 Between-group comparison on 6-MWT distance
The Guidelines for the 6-MWT by American Thoracic Society (ATS) in 2012 was used to measure the 6-MWT distance[12]and evaluate exercise endurance in COPD patients.
After treatment, the 6-MWT distances were significantly improved in both groups (P<0.05,P<0.01); the improvement in 6-MWT distance in the treatment group was more significant than that in the control group (P<0.05). This indicates that both treatment protocols can improve the exercise endurance in COPD patients; however, Seretide inhaler combined with acupuncture obtained better results than Seretide alone (Table 7).
Table 7. Between-group comparison on 6-MWT distance before and after treatment
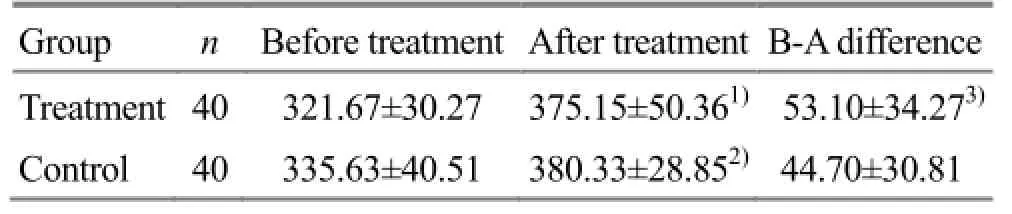
Table 7. Between-group comparison on 6-MWT distance before and after treatment
Note: B-A=Before-after; intra-group comparison before and after treatment, 1) P<0.01, 2) P<0.05; compared with the control group, 3) P<0.05
?
3.3.4 Between-group comparison on pulmonary ventilation function before and after treatment
After treatment, the FEV1% in both groups were significantly improved (P<0.01,P<0.05); the FEV1% improvement was more noticeable than that in the control group (P<0.05), showing a statistical significance. After treatment, the FEV1/FVC% in both groups were improved, showing no statistical significances (bothP>0.05). This indicates that Seretide inhaler alone or in combination with acupuncture can both improve FEV1% in COPD patients; however, combining Seretide inhaler and acupuncture showed better results than Seretide inhaler alone. The two methods worked better for FEV1% than FEV1/FVC% (Table 8).
Table 8. Between-group comparison on pulmonary functions before and after treatment
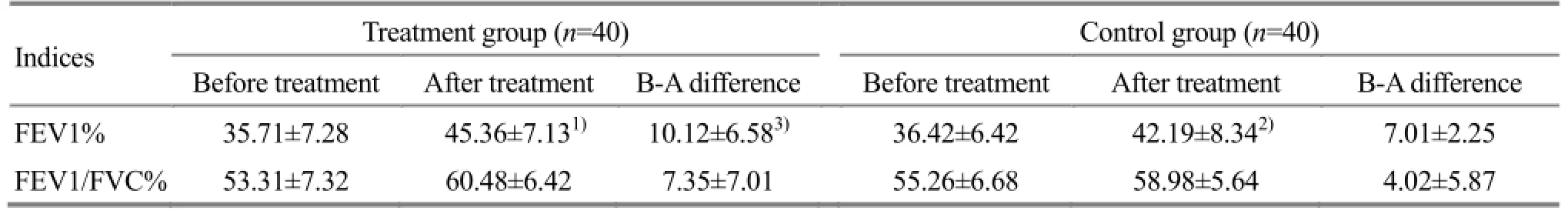
Table 8. Between-group comparison on pulmonary functions before and after treatment
Note: Intra-group comparison before and after treatment, 1) P<0.01, 2) P<0.05; compared with the control group, 3) P<0.01
?
4 Discussion
In TCM, COPD falls under the category of ‘lung distension’ and ‘dyspnea syndrome’. It is a chronic lung condition characterized by repeated lung distension and fullness and inability of lung qi to descend. Factors contributing to or aggravating include lung deficiency, retention of turbid-phlegm and external contraction of pathogens.
This condition is first located in the lung and, over time, involving the spleen and kidney. In later stage, it may also affect the heart. External pathogenic factors often attack the lung first via the mouth, nose and skin and affect the dispersing and descending function of the lung. This may cause lung qi to ascend and result in cough and dyspnea. This can further lead to lung qi deficiency coupled with lung distension and fullness. Over time, lung problems may affect the spleen (son’s disease affecting the mother) and result in deficiency of the lung and spleen.
Since the root cause of COPD is deficiency and it may manifest as excessive symptoms, the treatment strategies are to supplement healthy qi and remove pathogenic factors. In remission stage, the treatment is mainly focused on tonifying the lung, spleen and kidney. Liu LY, et al believe pathogenesis of COPD lies in deficiencies of the lung, spleen and kidney and qi stagnation due to qi deficiency[13]. Tian ZJ, et al believe deficiencies of the lung, spleen and kidney occur in different COPD stages, particularly dysfunctions of the lung and kidney; excessive symptoms of COPD are mainly associated with phlegm, stasis and six external pathogenic factors, particularly phlegm and stasis[14]. Survey on 410 COPD cases in Xinjiang Uyghur Autonomous Region by Xu D, et al showed that COPD can be differentiated into 14 patterns: simple excess pattern in 126 cases, simple deficiency pattern in 167 cases and mixed deficiency and excess in 117 cases; most common patterns include kidney yang deficiency, lung qi deficiency, turbid-phlegm obstructing the lung, wind-cold attacking the lung, kidney yin deficiency, cold dryness (in northwestern region of China), and spleen qi deficiency. Except for cold dryness (characteristic pattern in northwestern region of China), the rest patterns are deficient in root cause but manifested as phlegm in symptoms[15].
Chronic COPD can cause deficiencies of the lung, spleen and kidney. Qi deficiency can cause stagnation of fluid and blood, leading to turbid-phlegm, water-fluid retention and stagnant blood[16]. As a result, the treatment strategies are to tonify the lung, reinforce the kidney and strengthen the spleen. In this study, Feishu (BL 13), Shenshu (BL 23), Qihai (CV 6), Guanyuan (CV 4), Dingchuan (EX-B 1), Danzhong (CV 17), and Zusanli (ST 36) were used to tonify the lung, spleen and kidney, resolve phlegm and disperse lung qi. Of the above points, combining Qihai (CV 6), Guanyuan (CV 4) and Zusanli (ST 36) can stop sinking of spleen qi; combined Guanyuan (CV 4), Shenshu (BL 23) and Qihai (CV 6) can tonify kidney qi; and combining Dingchuan (EX-B 1) and Danzhong (CV 17) can coordinate yin and yang, warm yang and dissipate cold[17-19].
This study has proven that Seretide combined with acupuncture can improve clinical signs, symptoms and 6-MWT distance as well as FEV1% in COPD patients.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by Shanghai Key Laboratory for Clinical Chinese Medicine (上海市中醫(yī)臨床重點(diǎn)實(shí)驗(yàn)室, No. 14DZ2273200).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 25 March 2015/Accepted: 28 April 2015
[1] Ministry of Health of the People’s Republic of China. 2007 China Health Statistical Yearbook. Beijing: Peking Union Medical College Press, 2007.
[2] Barnes PJ. Chronic obstructive pulmonary disease. N Engl J Med, 2000, 343(4): 269-280.
[3] Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ, Nishimura M, Stockley RA, Sin DD, Rodriguez-Roisin R. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med, 2013, 187(4): 347-365.
[4] The State Administration of Traditional Chinese Medicine. Traditional Chinese Medicine Diagnostic and Therapeutic Protocols for 105 Diseases in 24 Disciplines. Beijing: Division of Medical Administration, State Administration of Traditional Chinese Medicine, 2011: 103-104.
[5] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Beijing: China Medical Science Press, 2002: 54-58.
[6] Group of Chronic Obstructive Pulmonary Disease, Chinese Thoracic Society. COPD diagnosis and treatment guidelines (2013 revised edition). Zhongguo Yixue Qianyan Zazhi: Electronic Version, 2014, 6(2): 67-80.
[7] Chen YH, Wang C. GOLD global strategy for diagnosis, management and prevention of COPD. Zhongguo Yixue Qianyan Zazhi: Electronic Version, 2015, 7(2): 34-39.
[8] Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest, 1988, 93(3): 580-586.
[9] Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD assessment test. Eur Respir J, 2009, 34(3): 648-654.
[10] Chai JJ, Liu T, Cai BQ. Evaluation of clinical significance of chronic obstructive pulmonary disease assessment test. Chin J Tuberc Respir Dis, 2011, 34(4): 256-258.
[11] Rabe KF, Wedzicha JA. Controversies in treatment of chronic obstructive pulmonary disease. Lancet, 2011, 378 (9795): 1038-1047.
[12] American Thoracic Society Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories.ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med,2002, 166(1): 111-117.
[13] Liu LY, Zou ZW, Li ZJ. Research advance on spleen/ kidney-tonifying method for chronic obstructive lung disease. Jilin Yixue, 2011, 32(23): 3-6.
[14] Tian ZJ, Xu YM, Li YQ. TCM pathogenesis of chronic obstructive lung disease. Hubei Zhongyi Xueyuan Xuebao, 2001, 3 (1): 29-30.
[15] Xu D, Gao Z, Jing J, Yang CH, Li Z, Liao CY, Li FS. 410 cases of patients with chronic obstructive pulmonary disease syndromes distribution in Xinjiang. Zhongguo Shiyan Fangjixue Zazhi, 2012, 18(3): 45-47.
[16] Chen XJ, Zhang BL. Chinese Internal Medicine. Shanghai Scientific & Technical Publishers, 2004: 64.
[17] Luo Q, Wang LS, Wu Z, Zhang ZP, Wang Y, Peng L. Observations on the efficacy of moxibustion and acupuncture point injection as main treatment for stable chronic obstructive pulmonary disease. Shanghai Zhenjiu Zazhi, 2012, 31(12): 871-873.
[18] Shi MY, Shu ZT, Zhang W, Tian J. Effect of rapid point pressure on therapeutic efficacy and pulmonary function in patients with chronic persistent bronchial asthma. J Acupunct Tuina Sci, 2015, 13 (1): 36-43.
[19] Liu XH, Liu Q. Effect of earth-supporting and metal-generating therapy for chronic obstructive pulmonary disease during remission stage. Xin Zhongyi, 2002, 34(10): 18-19.
Translator: Han Chou-ping (韓丑萍)
針刺治療慢性阻塞性肺疾病的臨床療效觀察
目的:觀察針刺治療慢性阻塞性肺疾病(chronic obstructive pulmonary disease, COPD)的臨床療效及對(duì)患者肺通氣功能、6分鐘步行測(cè)試(6-minute walk test, 6-MWT)距離的影響。方法:共納入80例COPD患者(肺功能GOLD 3-4級(jí), 中醫(yī)辨證為肺腎氣虛證), 按就診順序隨機(jī)分為治療組與對(duì)照組, 每組40例。兩組均以沙美特羅替卡松粉吸入劑(舒利迭, 50 μg/250 μg, 早晚各一次吸入)作為基礎(chǔ)治療。治療組在此基礎(chǔ)上加用針刺肺俞、腎俞、氣海、關(guān)元、定喘、膻中、足三里, 每星期2次, 連續(xù)治療3個(gè)月后觀察兩組治療臨床療效及肺通氣功能、6-MWT距離等指標(biāo)變化。結(jié)果:治療3個(gè)月后, 治療組總有效率為95.0%, 對(duì)照組為80.0%, 兩組差異有統(tǒng)計(jì)學(xué)意義(P<0.05); 治療組咯痰、喘息、氣短積分改善優(yōu)于對(duì)照組且有統(tǒng)計(jì)學(xué)差異(P<0.01,P<0.05); 治療組6-MWT距離和第一秒用力呼氣容積占預(yù)計(jì)值比值(forced expiratory volume in 1 second percentage of predicted value, FEV1%)增加優(yōu)于對(duì)照組且有統(tǒng)計(jì)學(xué)差異(P<0.05,P<0.01)。結(jié)論:舒利迭加用針刺療法能改善COPD患者臨床癥狀及體征, 增加6-MWT距離, 提高FEV1%, 其療效優(yōu)于單用舒利迭。
針刺療法; 肺疾病, 慢性阻塞性; 呼吸功能測(cè)試; 心功能測(cè)試
R246.1 【
】A
Author: Liu Lu-jiong, attending physician
Jiang Chun-juan, vice chief physician.
E-mail: shantapeace@163.com
Methods:A total of 80 COPD patients [grade 3-4 in Global Initiative for Chronic Obstructive Lung Disease (GOLD), qi deficiency of the lung and kidney in traditional Chinese medicine (TCM) pattern] were randomly allocated into a treatment group (n=40) and a control group (n=40). Salmeterol Xinafoate and Fluticasone Propionate powder (Seretide, 50 μg/250 μg) for inhalation was used for basic treatment in both groups (once in the morning and once in the evening). Patients in the treatment group received acupuncture at Feishu (BL 13), Shenshu (BL 23), Qihai (CV 6), Guanyuan (CV 4), Dingchuan (EX-B 1), Danzhong (CV 17) and Zusanli (ST 36) twice a week for 3 months. After 3 months of treatment, clinical effects, lung ventilation functions and 6-MWT distance were observed and compared in the two groups.
Results:After 3 months of treatment, the total effective rate was 95.0% in the treatment group, versus 80.0% in the control group, showing a statistical difference (P<0.05); the phlegm expectoration, dyspnea and shortness of breath were more significantly improved in the treatment group than those in the control group (P<0.01,P<0.05); and the 6-MWT distance and forced expiratory volume in 1 second percentage of predicted value (FEV1%) were more significantly improved in the treatment group than those in the control group (P<0.05,P<0.01).
Conclusion:Seretide inhaler combined with acupuncture can improve signs and symptoms in COPD patients, increase the 6-MWT distance, improve FEV1% and obtain better results than Seretide alone.
 Journal of Acupuncture and Tuina Science2015年5期
Journal of Acupuncture and Tuina Science2015年5期
- Journal of Acupuncture and Tuina Science的其它文章
- Electroacupuncture at Houxi (SI 3) for acute lumbar sprain: a meta-analysis of randomized controlled trials
- Clinical observation on warm needling therapy for scapulohumeral periarthritis: a randomized controlled trial
- Clinical observation on acupuncture plus chiropractic treatment for cervical spondylosis
- Observation on clinical effect of acupuncture for cervical spondylosis of vertebral artery type
- Scalp acupuncture combined with body acupuncture for 32 cancer cases with intractable hiccups after radiochemotherapy
- Clinical observation on acupuncture combined with Chinese medicine and rehabilitation training for subacute stroke patients
