Nurses'perception of risk factors for infusion phlebitis:A cross-sectional survey
Xiang-Feng Li,Wei Liu,Ying QinInternational Medical Service,Peking Union Medical College Hospital,Beijing,100730,China
Original article
Nurses'perception of risk factors for infusion phlebitis:A cross-sectional survey
Xiang-Feng Li,Wei Liu,Ying Qin*
International Medical Service,Peking Union Medical College Hospital,Beijing,100730,China
ARTICLEINFO
Article history:
Received in revised from
9 April 2015
Accepted 25 December 2015
Available online 21 March 2016
Cross-sectional survey
Nurses
Perception
Phlebitis
Risk factors
ABSTRACT
Objective:The aim of the present study was to investigate Chinese nurses'perception of risk factors for phlebitis.
Methods:A convenience sample of hospital nurses was recruited in Beijing,China.Data were collected using a demographic information questionnaire and a questionnaire measuring nurses'perception of risk factors for infusion phlebitis.
Results:It was found that knowledge of risk factors for infusion phlebitis was incomplete,even among experienced nurses in the study participants.A high rate of incorrect answers to questions about the pH of fluid(89.9%),gauze or polyurethane catheter dressings(79.1%),and steel needles for drug infusion (76.3%)was observed.
Conclusions:These findings suggest that nurses should be trained about the risk factors for infusion phlebitis.
?2016 Shanxi Medical Periodical Press.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
1.Introduction
Among hospital inpatients,intravenous fluid therapy is the most common invasive procedure.More than 90%of patients in hospitals receive IV therapies through certain forms of intravenous device.1The most common complication is infusion phlebitis,which is defined by pain,erythema(redness of the skin),swelling,and palpable thrombosis of the cannulated vein.2Patients with infusion phlebitis mayexperience morepain,longer wait for therapy,slower recovery,and extended stays in the hospital.3
A number of studies of risk factors for infusion phlebitis have been published recently.According to these studies,risk factors for infusion phlebitis include the infusion set and catheter material,location of the catheter,duration of catheterization,pH and osmolality of the fluid and presence of contaminants in the infusion solutions.4The role of drugs,rate of flow,using continuous infusion to maintain catheter patency and host factors such as gender,age,and medical history have also been explored.5
In 1984,Tomford observed that the skill of the IV nurses who insert the catheter affects the incidence of phlebitis.6Severalstudies have also indicated that well-trained IV therapists and routine documentation are associated with a lower risk of catheter infection than is seen with regular nurses.5
Evidence suggests that nurses'knowledge of infusion phlebitis and its risks factors may influence the risk for infusion phlebitis in hospitals.7So our study,performed in Beijing,China,investigated nurses'perception of the risk factors for infusion phlebitis.
2.Methods
This cross-sectional study was carried out from July 2013 to September 2013 in the International Medical Service of Peking Union Medical College Hospital,China.PUMC Hospital is a large tertiary hospital with 1800 beds.The International Medical Service is a setting that includes surgical and medical departments,maternal child health sections,and outpatient and emergency departments.We used a convenience sample.All(140)nurses of the IMS who provided informed consent were included.
The questionnaire assessing perception of risk factors for infusion phlebitis was developed by Lanbeck and colleagues.8As it was not copyrighted,permission was not necessary to use and modify some of their items for our study.A preliminary forward-back translation of this original version was performed to establish semantic and conceptual equivalence in the Chinese context.The new instrument consisted of two sections:(1)demographic information,including gender,age,years of experience,and education level,and (2)nurses'perception of risk factors for infusion phlebitis.14 questions in this questionnaire addressed perceived risk factors for infusion phlebitis,listing several answer options.Completion of the questionnaire took approximately 15-20 min.The questionnaire's face validity was 1.0.To assess the reliability of the questionnaire,a pilot test-retest study with a three-week interval was performed. Item reliability was good,with Cohen's K>0.6.
http://dx.doi.org/10.1016/j.cnre.2016.03.002
2095-7718/? 2016 Shanxi Medical Periodical Press.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Statistical analysis was performed using SPSS 17.0.All data were recorded as average± standard deviation or percentage.The Pearson correlation and Fisher's exact test for differences between groups were used for inferential statistics.Values of P<0.05 were considered significant.
3.Results
3.1.Sample characteristics
Of the 140 enrolled participants,139(99.3%)responded.Only one nurse declined to return the questionnaire.100%of the participants were clinical nurses and 99.3%of them were female.The population was young,with a median age of 30.09 years.Participants averaged 8.44±5.50 years of experience.Approximately 33.1%of the study population held a junior college diploma and 2.2%of the study population had graduated from a secondary nursing school;62.6%of the nurses held a bachelor's degree,while 2.2%held a master's degree.Regarding job rank,27.3%of the respondents were nurses,59.7%were nurse practitioners,and 12.9% were nurses in charge or at higher level.Most participants worked in maternal child health sections and surgical departments(34.5% and 28.1%,respectively).Demographics and participants'characteristics are summarized in Table 1.
3.2.The results of the survey
The multiple-choice questions,response options and observed answers are shown in Table 2.The results showed that 47.5%of the nurses thought that phlebitis is a large problem,while 51.1% thought that it is a medium problem;96.4%of the nurses agreed that a peripheral venous catheter should not be in place for longer than 72 h;70.5%of the nurses thought that a skilled vein puncture decreases the risk for phlebitis and 69.1%also agreed that routines for documenting the insertion of a peripheral venous catheter decreases the risk for phlebitis.79.1%of the participant answered that the dressing affects the risk for phlebitis.Almost half of the nurses (56.8%)thought a bolus injection can decrease the risk for phlebitis.
By analyzing the 14 answers to the questionnaire,a high rate of incorrect answers were found to be related to the questions about the pH of fluids(89.9%)and about the use of gauze or polyurethane catheter dressings(79.1%)and steel needles for drug infusion (76.3%)(Table 2).After analyzing nurses'perceptions about the risk factors for phlebitis,we observed a difference as a function of the respondents'level of education and work experience.
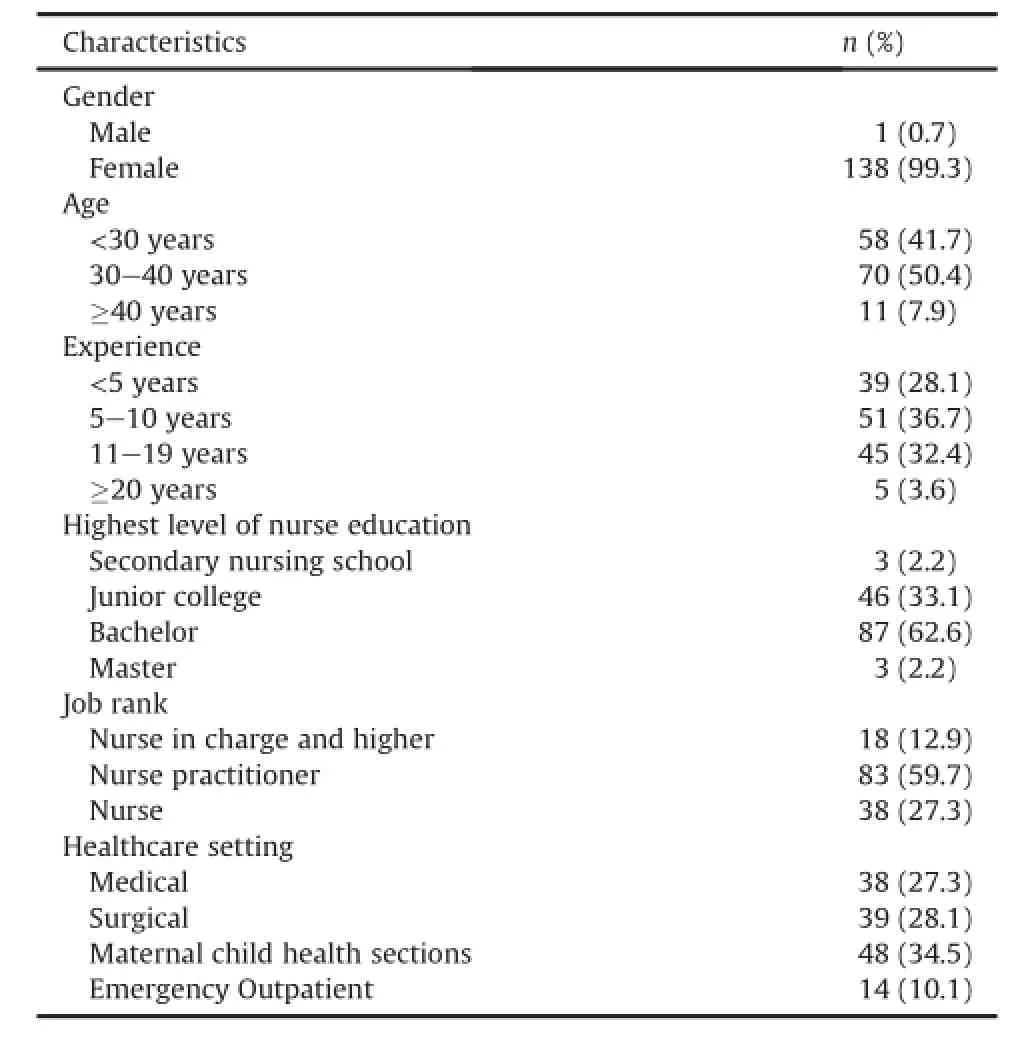
Table 1Sample characteristics of 139 nurses of PUMC hospital in Beijing,China.
4.Discussion
Phlebitis is the most common complication of intravenous catheters,and it can lead to many problems,including higher costs of therapy and longer hospital stays.In our study,almost all of the nurses believed that phlebitis was a large or medium problem.The results indicated that phlebitis is the most common side effect in clinical practice and the nurses have to pay enough attention to it.
4.1.Patient-specific factors
Female sex,old age,“poor quality”peripheral veins and the presence of underlying medical disease(cancer,immunodeficiency)appear to increase the risk of peripheral vein infusion phlebitis.9,10However,only 5.7%of the nurses in our study knew that female sex is a risk factor.70.7%of the nurses knew the risk increases with old age,64.1%knew the risk increases in patients with cancer and 87.1%knew that immobilization increases the risk.
4.2.Duration catheter retention
Currently,routine replacement of the catheter is thought to reduce the risk of phlebitis and bloodstream infection.11CDC guidelines recommend replacement of peripheral intravenous(IV)catheters no more frequently than every 72-96 h,and most hospitals in China follow this recommendation.In our study,almost all of the nurses believed that a catheter should be replaced no less frequently than 72-96 h,and peripheral catheters are replaced every 72 h to prevent irritation of the vein in our hospital.However,Webster's study in 201311found no evidence to support the current practice of routinely changing catheters every three to four days.
4.3.Catheter type
It has been reported that fine-bore catheters can decrease the risk of phlebitis.The use of newer plastic materials has reduced the importance of this factor.12In this study,the nurses'answers did not reflect current knowledge.Only 23.6%of the nurses believed that plastic materials could reduce the incidence of phlebitis.This finding may explain why nurses still use metal needles for infusion in clinical practice in China,while many countries use needles only for taking blood.54.3%of the nurses knew of the risk associated with fine-bore catheters,while 46.4%of the nurses knew of the risk associated with long catheters.
Nurses with college education,as opposed to nurses with higher education(Bachelor's and Master Degree),were less aware that the cannula's material could affect the incidence of phlebitis(Fisher's exact test=20.22,P=0.00).
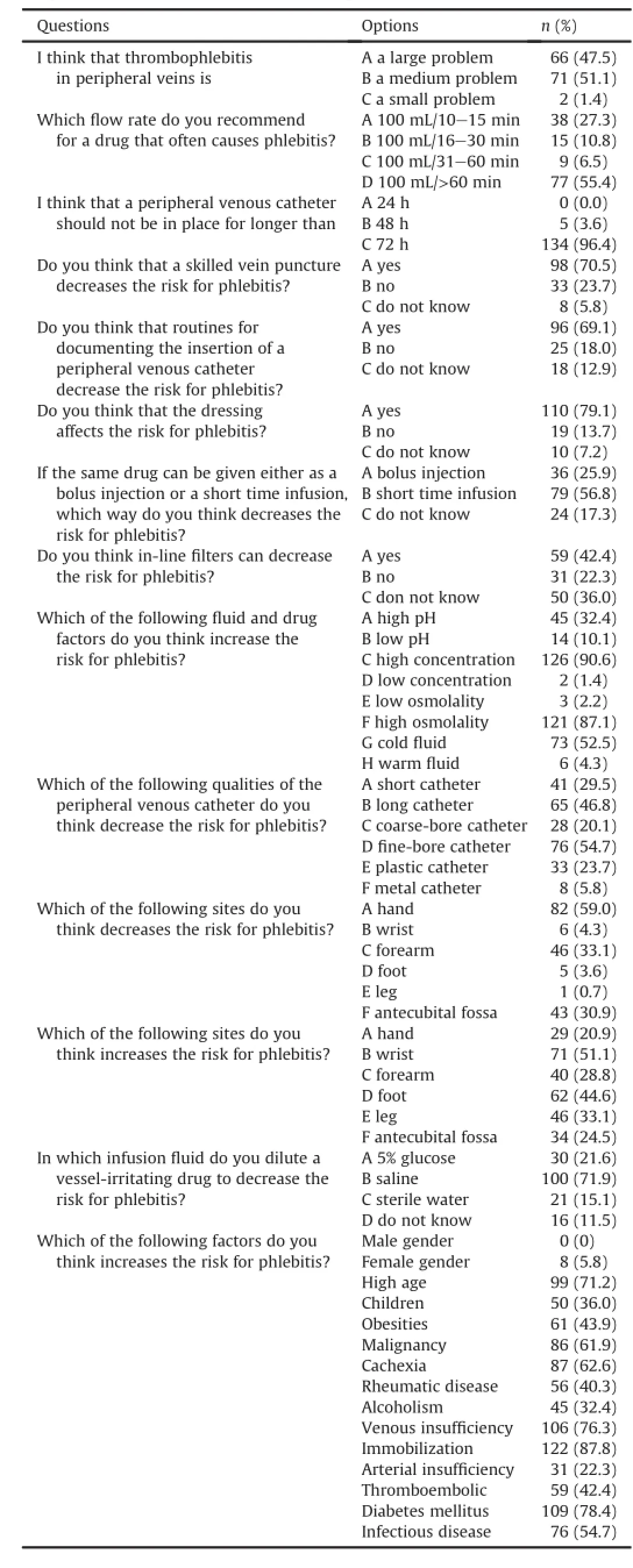
Table 2Frequency of answers to the risk factors for phlebitis.
4.4.Insertion sites
There is still another dilemma to be resolved for successful intravenous management.Namely,the use of the upper extremities for peripheral catheter insertion is recommended by current guidelines.13Insertion of the catheter in the forearm or the antecubital fossa is associated with a higher risk than in the hand or the wrist according to the updated CDC guidelines.In our study,59.0%of the nurses thought the hand was the preferred site,while 50%thought the wrist was an undesirable choice.So,the level of nurses'knowledge of practices recommended by guidelines was not high.However,Giancarlo conducted a multi-center prospective study in 2014.In his study,he found that the antecubital fossa and forearm veins may be the preferredanatomicalsitesforperipheralintravenous cannulation.14
There was a significant difference in the nurses'perception of the appropriate insertion site for an intravenous cannula to reduce the incidence of phlebitis as a function of work experience(Pearson chi square=29.69,P=0.00).Nurses who had between six and ten years of experience chose a better vein,in comparison with colleagues with less experience,who predominantly selected hand veins.
4.5.Fluid and drugs
It is well known that high as well as low pH and osmolality of a drug or fluid can increase the risk of phlebitis.15However,in this study,only 32.1%knew high pH can increase the risk and 10.0%knew low pH can increase the risk.86.4%of the nurses knew of the risk associated with high osmolality,and 90%knew the risk associated with high concentration.Half of the nurses knew the temperature of a fluid can reduce the vessel-irritating effectofdrugs.Obviously,thesenurseslackknowledge regarding the impact on phlebitis of the characteristics of fluid and drugs.
4.6.In-line filter
Studies have indicated that in-line IV filters could be an effective approach to remove contaminants from IV solutions,thus reducing the rate of phlebitis.16However,Barbara reviewed eleven RCTs (1633 peripheral catheters)in 2009,and his study indicated that inline filters in peripheral IV catheters could not be recommended routinely because evidence for their benefit was uncertain.4In our study,42.1%of the nurses believed that in-line filters can reduce the risk of phlebitis,while 35.7%indicated they were uncertain about their effect.
4.7.Flow rate
Kiyotaka et al conducted a prospective randomized trial to determine whether a 1-min bolus injection of vinorelbine reduced the incidence of local venous toxicity compared with a 6-min drip infusion.They found that the administration of the 1-min bolus of vinorelbine did not significantly reduce the incidence of local venous toxicity compared with the 6-min infusion.17In our study,56.8%of the participants believed that a shorter infusion time would decrease the risk.
According to Simamora,a shorter infusion time for a drug that often causes phlebitis can decrease the risk for phlebitis.18Furthermore,shortening the infusion time of vinorelbine has also been reported to reduce the incidence of drug induced-phlebitis.19However,55.4%of the nurses chose a longer infusion time to decrease the risk in our study,as did 63%of the Swedish nurses inLanbeck and colleagues'study.8These findings indicate that nurses' knowledge needs to be updated.
4.8.Other factors
CDC guidelines report that no evidence supports the idea that the dressing affects the risk for phlebitis.The majority of nurses (86.3%)in this study answered this question incorrectly,and Lanbeck and colleagues found the same result in their study.
Several studies have indicated that well-trained IV therapists and routine documentation are associated with a lower risk of catheter infection than regular nurses.11In our study,most of the nurses endorsed this relation.
5.Conclusions
In conclusion,several of the recommended procedures for preventing infusion phlebitis were not known by most of the participating nurses.It is especially alarming that factors proven to be harmful,such as the use of metal needles,are still frequently used.Improvement in nurses'knowledge regarding risk factors for infusionphlebitis is needed.A periodic check of nurses'perceptions about the risk factors for the development of phlebitis,using the questionnaire that was administered in our study,can help nurse managersdeterminewherenursesshouldreceivetraining. Providing sufficient education,creating a positive attitude and addressing barriers are all important strategies for improving knowledge among nursing staff.
6.Limitations
Our results may be affected by selection bias.The participants in this study were selected by convenience sampling.It is quite possible that nurses of other hospitals have evenworse knowledge. If so,the results of the survey could lead to underestimated.
Author contribution
Xiangfeng Li conceived the study and designed the trial.Wei Liu and Ying Qin supervised the implementation of the trial and data collection.
Conflicts of interest
All contributing authors declare no conflicts of interest. Acknowledgments
The authors would like to acknowledge the clinicians who participated in this study.This research received no specific grant from any funding agency in the public,commercial or not-for-profit sectors.
References
1.Moureau N.Vascular safety:it's all about PICCs.Nurs Manage.2006;37:22-27.
2.Maki DG,Mermel LA.Infections due to infusion therapy.In:Bennett JV,Brachman PS,eds.Hospital Infections.Philadelphia,Pennsylvania:Lippincott-Raven Publishers;1998:689-724.
3.Filippon LM.Diagnosis:superficial phlebitis.Emerg Med News.2005;27:29.
4.Ni.el-Weise BS,Stijnen T,van den Broek PJ.Should in-line filters be used in peripheral intravenous catheters to prevent infusion-related phlebitis?a systematic review of randomized controlled trials.Anesth Analg.2010;110:1624-1629.
5.Lee WL,Chen HL,Tsai TY,et al.Risk factors for peripheral intravenous catheter infection in hospitalized patients:a prospective study of 3165 patients.Am J Infect Control.2009;37:683-686.
6.Tomford JW,Hershey CO,McLaren CE,Porter DK,Cohen DI.Intravenous therapy team and peripheral venous catheter-associated complications:a prospective controlled study.Arch Intern Med.1984;144:1191-1194.
7.Gorski LA.Infusion nursing standards of practice.J Infus Nurs.2007;30:151-152.
8.Lanbeck P,Odenholt I,Paulsen O.Perception of risk factors for infusion phlebitis among Swedish nurses:a questionnaire study.J Infus Nurs.2004;27:25-30.
9.Tagalakis V,Kahn SR,Libman M,Blostein M.The epidemiology of peripheral vein infusion thrombophlebitis:a critical review.Am J Med.2002;113:146-151.
10.Cicolini G,Bonghi AP,Di Labio L,Mascio Di.Position of peripheral venous cannulae and the incidence of thrombophlebitis:an observational study.J Adv Nurs.2009;65:1268-1273.
11.Webster J,Osborne S,Rickard CM,New K.Clinically-indicated replacement versus routine replacement of peripheral venous catheters.Cochrane Database Syst Rev.2013;4:CD007798.
12.Everitt NJ,McMahon MJ.Influence of fine-bore catheter length on infusion thrombophlebitis in peripheral intravenous nutrition:a randomised controlled trial.Ann R Coll Surg Engl.1997;79:221-224.
13.O'Grady NP,Alexander M,Burns LA,et al.Summary of recommendations:guidelines for the prevention of intravascular catheter-related infections.Clin Infect Dis.2011;52:1087-1099.
14.Cicolini G,Manzoli L,Simonetti V,et al.Phlebitis risk varies by peripheral venous catheter site and increases after 96 hours:a large multi-centre prospective study.J Adv Nurs.2014;70:2539-2549.
15.Chee S,Tan W.Reducing infusion phlebitis in Singapore hospitals using extended life end-line filters.J Infus Nurs.2002;25:95-104.
16.Ball PA.Intravenous in-line filters:filtering the evidence.Curr Opin Clin Nutr Metab Care.2003;6:319-325.
17.Yoh K,Niho S,Goto K,et al.Randomized trial of drip infusion versus bolus injection of vinorelbine for the control of local venous toxicity.Lung Cancer. 2007;55:337-341.
18.Simamora P,Pinsuwan S,Alvarez JM,Myrdal PB,Yalkowsky SH.Effect of pH on injection phlebitis.J Pharm Sci.1995;84:520-522.
19.Yoh K,Niho S,Goto K,et al.A randomized trial of 6-minutes drip infusion versus 1-minute bolus injection of vinorelbine(VNR)for the control of drug induced-phlebitis.J Clin Oncol.2004;9:758.
2 February 2015
*Corresponding author.
E-mailaddresses:283333905@qq.com(X.-F.Li),qinying_2809@163.com (Y.Qin).
Peer review under responsibility of Shanxi Medical Periodical Press.
- Frontiers of Nursing的其它文章
- GUIDE FOR AUTHORS
- Aims and Scope
- Study of the effect of humanistic nursing care model wards in Children Caring Ward School on the nurses'caring ability☆
- Analysis of risk factors and the establishment of a risk model for peripherally inserted central catheter thrombosis
- Applying healthcare failure mode and effect analysis to patient pain management in the anesthesia recovery period
- Tai Chi as an intervention to reduce falls and improve balance function in the elderly:A meta-analysis of randomized controlled trials

