Bacteremia or pseudobacteremia? Review of pseudomonas fl uorescens infections
Takeshi Nishimura, Kenji Hattori, Akihiko Inoue, Taiji Ishii, Tetsuya Yumoto, Kohei Tsukahara, Astunori Nakao, Satoshi Ishihara, Shinichi Nakayama
1Hyogo Emergency Medical Center, 1-3-1 Wakinohamakaigando-ri, Chuo-ku, Kobe, Hyogo 651-0073, Japan
2Department of Emergency and Critical Care Medicine, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, 2-5-1 Shikatacho, Kitaku, Okayama City, Okayama, 700-8558, Japan
Bacteremia or pseudobacteremia? Review of pseudomonas fl uorescens infections
Takeshi Nishimura1, Kenji Hattori1, Akihiko Inoue1, Taiji Ishii1, Tetsuya Yumoto2, Kohei Tsukahara2, Astunori Nakao2, Satoshi Ishihara1, Shinichi Nakayama1
1Hyogo Emergency Medical Center, 1-3-1 Wakinohamakaigando-ri, Chuo-ku, Kobe, Hyogo 651-0073, Japan
2Department of Emergency and Critical Care Medicine, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, 2-5-1 Shikatacho, Kitaku, Okayama City, Okayama, 700-8558, Japan
World J Emerg Med 2017;8(2):151–154
INTRODUCTION
P. fluorescens is an aerobic, Gram-negative bacillus related to Pseudomonas aeruginosa. Like other species of Pseudomonas, the organism is widespread in nature and is found in water, moist soil, and vegetation. Due to its low virulence, P. fluorescens is an infrequent cause of infections except for catheter-related bloodstream infections in cancer patients.
From August 1, 2003 to May 31, 2016, Hyogo Emergency Medical Center and the Kobe Red Cross Hospital treated three cases of bloodstream infection caused by P. fluorescens. Were these cases true bacteremia or pseudobacteremia? Would it be a risk to induce nosocomial infection, possibly leading to an infection outbreak? We retrospectively examined these three cases in detail.
METHODS
We reviewed the database at the Hyogo Emergency Medical Center and the Kobe Red Cross Hospital for cases of P. fl uorescens bloodstream infection treated from August 2003 to May 2016. Baseline characteristics, basal disease, clinical course, laboratory data, use of bloodassociated products, and laboratory examinations were retrospectively analyzed in these cases.
RESULTS
Three patients who met these criteria and had P. fluorescens in their blood cultures were analyzed. Data was retrospectively collected from their medical records (Table 1).
Case 1
A 77-year-old man with a history of esophageal carcinoma was admitted to the hospital complaining of esophageal stenosis. Parenteral nutrition support was started via a central venous catheter. On post-admissionday fi ve, he presented with severe malaise and chilliness. P. fluorescens was recovered from his blood culture. An antibiotic (cefozopran) was administered, and his conditions improved rapidly.
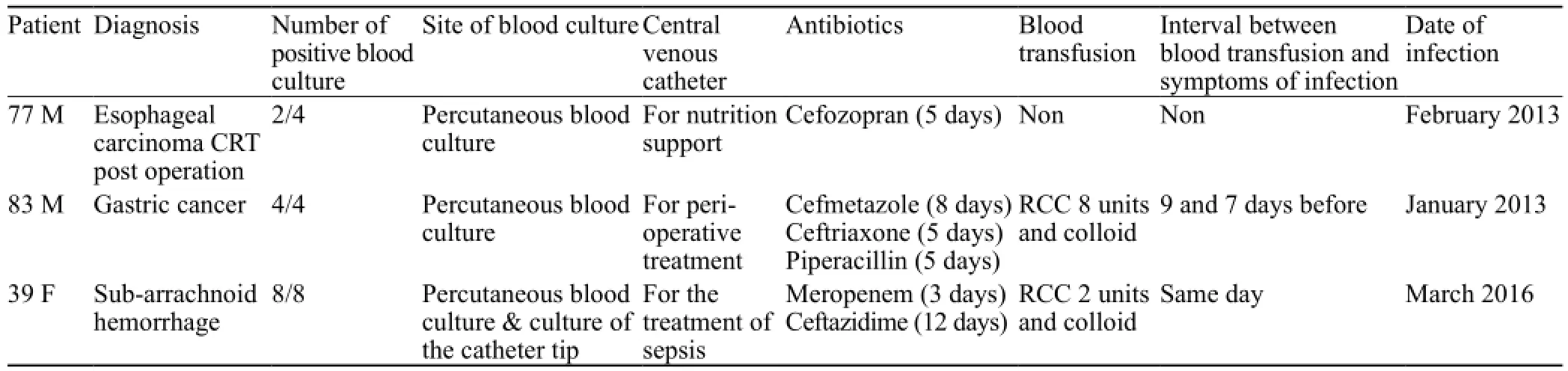
Table 1. Medical record of the patients
Case 2
An 83-year-old man with gastric cancer underwent gastric resection. On post-operative day seven, he suddenly presented with chilliness and shivering. A central venous catheter was also placed to support parenteral nutrition. An antibiotic (cefmetazole) had already been administered in the perioperative period. P. fluorescens was recovered from his blood culture. Removal of the central venous catheter prevented exacerbation of his conditions. Afterwards, he recovered uneventfully.
Case 3
A 39-year-old female was admitted to the hospital complaining of severe headache. She was diagnosed with subarachnoid hemorrhage due to rupture of an internal carotid-posterior communicating artery aneurysm. Emergent intracatheter treatment was performed to detect aneurysm rupture and embolize the vessels. Albumin and crystalloid were administered in the perioperative period. By post admission day 13, her vital signs had gradually deteriorated. Along with her exacerbating conditions, laboratory data was worsening. A central venous catheter was inserted on the same day. P. fl uorescens was recovered in her blood culture on post admission day 15. An antibiotic (ceftazidime) was rapidly administered. No events occurred after recovery from septic shock. She was referred from the intensive care unit (ICU) to the neurosurgery department on post admission day 32.
According to the case 3 patient, P. fluorescens was detected from percutaneous blood culture and catheter tip. This result could fit the criteria of catheter-related bloodstream infection.[1]
DISCUSSION
P. fluorescens is an aerobic Gram-negative bacillus related to Pseudomonas aeruginosa. This organism has an aspect as psychrophilic, therefore it can grow in refrigerated temperatures (4 °C) and use citrate as a carbon source for growth.[2]Like other members of the genus Pseudomonas, P. fl uorescens is widespread in nature with a predilection for moist environments. P. fl uorescens is considered as an infrequent cause of human infection due to its low virulence and has been implicated mainly in pseudobacteremia outbreaks.[3,4]Immune-compromised patients with cancer are sometimes afflicted with infection. Because blood products are maintained in refrigeration for long periods of time, P. fl uorescens can potentially cause critically severe problems. Scales et al[5]published a paper describing about the review of P. fluorescens. They described that most common site of P. fluorescens infection is the bloodstream, and most reported cases have been iatrogenic. Although most true blood transfusion-associated P. fluorescens bloodstream infections have been reported in the 1980s,[6–9]specific reports have not been published in recent decades, owing to high purif i cation skills.
To our best knowledge, three reports of P. fl uorescens infections among patients associated with intrinsically contaminated infusions,[10–14]and one report of an oncology patient from unknown origin[15]have been published. Gershman et al[12]and Benito et al[11]reported contaminated heparinized saline flush syringes and contaminated ice baths used to cool syringes for cardiac output determination in the cardiac care unit respectively. Wong et al[10]reported the spread of P. fluorescens derived from contaminated drinking water with bone marrow transplant patients. In the first published case associated with a P. fluorescens outbreak among cancer patients by Hsueh, the cause of infection and pathway of outbreak could not be determined.
Dalamaga et al[16]reported the fi rst recorded case of infection with P. fluorescens strain, causing cutaneous abscess and recurrent bacteremia in a patient following a dog bite. P. fl uorescens has also been reported to induce critical conditions such as endotoxic shock,[17]neonate sepsis,[18]meningitis,[19]and respiratory infections.[20]Although case reports of P. fl uorescens bacteremia have been published, reports in recent decades have been rare.
Because of its low virulent infection, it is rare that P. fluorescens causes bacteremia leading to septic shock. Pseudobacteremia may be defined as the presence of bacteria in the blood culture in the absence of clinical or other bacteriologic evidence of bloodstream infection. Contaminations of blood culture may occur during venipuncture, in the preparation of culture media, or during laboratory processing of the culture. Contaminated lithium heparin bottles have also played a role as a source of pseudobacteremia due to P. fl uorescens.[21,22]
All three of our cases were treated with central venous catheters and blood transfusion. While two had histories of cancer, one patient who sufferedfrom subarachnoid hemorrhage had no compromised history. Although we suspected that pseudobacteremia might occur, P. fluorescens was detected again in blood culture after administration of antibiotics. They all presented with malaise and chilliness; therefore, antibiotic treatments were administered respectively. In all cases, clinicians could not examine the pathway of infection. In cases 1 and 2, we examined the result from medical records retrospectively. An outbreak could be suspected because the 2 cases did occur in January and February 2013. However, that could not be confirmed and pathways of infection were not clarified. In case 3, we suspect that the blood products used might have been related to septic shock due to P. fluorescens infection; thus, we made inquiries to the blood product's company regarding infection. However, there is no evidence that bacteria had grown from blood products. Unfortunately, inappropriate dealing of central venous catheter might contribute to blood stream infection. Contamination of organisms into the blood stream can induce sepsis even when the organism is low virulent in nature. As a result, we could not detect the source of infection.
P. fluorescens is rare, but might cause infection in patients with cancer or immune-suppression. Based on our experience, central venous catheters should also be considered as a risk of infection leading to sepsis. We should examine closely whether an infection is truly bacteremia or pseudobacteremia when P. fluorescens is recovered from blood culture. Furthermore, we had to survey the circumstances to detect the infectious pathway and prevent outbreaks if the infection was truly bacteremia in healthy patients.
We believe that all three of our cases were truly bacteremia because they presented infectious symptoms such as malaise, chilliness, and inflammation. Fortunately, outbreaks did not occur. When P. fl uorescens is detected, we should detect the organism's infection pathway and consider potential infectious outbreaks in ICUs or cancer patient wards.
CONCLUSION
Although P. fl uorescens infections in recent decades have been rare due to clean blood products, the organism has the potential to induce sepsis, especially in patients with cancer or central venous catheters. We clinicians should be aware of these features when P. fluorescens is recovered in blood culture. Determining whether P. fluorescens is a true bacteremia or pseudobacteremia is important to prevent misunderstandings. Clinicians should reexamine the pathway of infection to prevent outbreaks if P. fl uorescens has truly occurred.
ACKNOWLEDGMENT
Authors appreciate for the medical staff of the department of Hyogo Emergency Medical Center and the Department of Emergency and Critical Care Medicine at Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences for improvement of this manuscript.
Funding: None.
Ethical approval: The study was approved by the Institutional Review Board.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations. Contributors: Nishimura T proposed the study and wrote the fi rst draft. All authors read and approved the fi nal version of the paper.
REFERENCES
1 Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O'Grady NP, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;49(1):1–45.
2 Pittman M. A study of bacteria implicated in transfusion reactions and of bacteria isolated from blood products. J Lab Clin Med. 1953;42(2):273–88.
3 Smith J, Ashhurst-Smith C, Norton R. Pseudomonas fl uorescens pseudobacteraemia: a cautionary lesson. J Paediatr Child Health. 2002;38(1):63–5.
4 Simor AE, Ricci J, Lau A, Bannatyne RM, Ford-Jones L. Pseudobacteremia due to Pseudomonas fluorescens. Pediatr Infect Dis. 1985;4(5):508–12.
5 Scales BS, Dickson RP, LiPuma JJ, Huffnagle GB. Microbiology, genomics, and clinical significance of the Pseudomonas fluorescens species complex, an unappreciated colonizer of humans. Clin Microbiol Rev. 2014;27(4):927–48.
6 Collignon P, Dreimanis D, Beckingham W. Pseudobacteraemia due to Pseudomonas fl uorescens. J Hosp Infect. 1999;43(4):321–2.
7 Murray AE, Bartzokas CA, Shepherd AJ, Roberts FM. Blood transfusion-associated Pseudomonas fl uorescens septicaemia: is this an increasing problem? J Hosp Infect. 1987;9(3):243–8.
8 Khabbaz RF, Arnow PM, Highsmith AK, Herwaldt LA, Chou T, Jarvis WR, et al. Pseudomonas fluorescens bacteremia from blood transfusion. Am J Med. 1984;76(1):62–8.
9 Gibaud M, Martin-Dupont P, Dominguez M, Laurentjoye P, Chassaing B, Leng B. Pseudomonas fluorescens septicemia following transfusion of contaminated blood. Presse Med. 1984;13(42):2583–4.
10 Wong V, Levi K, Baddal B, Turton J, Boswell TC. Spread of Pseudomonas fluorescens due to contaminated drinking water in a bone marrow transplant unit. J Clin Microbiol. 2011;49(6):2093–6
11 Benito N, Mirelis B, Luz Galvez M, Vila M, Lopez-Contreras J, Cotura A, et al. Outbreak of Pseudomonas fluorescens bloodstream infection in a coronary care unit. J Hosp Infect. 2012;82(4):286–9.
12 Gershman MD, Kennedy DJ, Noble-Wang J, Kim C, Gullion J, Kacica M, et al. Multistate outbreak of Pseudomonas fl uorescens bloodstream infection after exposure to contaminated heparinized saline fl ush prepared by a compounding pharmacy. Clin Infect Dis. 2008;47(11):1372–9.
13 Centers for Disease C, Prevention. Update: Delayed onset Pseudomonas fl uorescens bloodstream infections after exposure to contaminated heparin flush—Michigan and South Dakota, 2005–2006. MMWR Morb Mortal Wkly Rep. 2006;55(35):961–3.
14 Centers for Disease C, Prevention. Pseudomonas bloodstream infections associated with a heparin/saline fl ush—Missouri, New York, Texas, and Michigan, 2004–2005. MMWR Morb Mortal Wkly Rep. 2005;54(11):269–72.
15 Hsueh PR, Teng LJ, Pan HJ, Chen YC, Sun CC, Ho SW, et al. Outbreak of Pseudomonas fluorescens bacteremia among oncology patients. J Clin Microbiol. 1998;36(10):2914–7.
16 Dalamaga M, Karmaniolas K, Chavelas C, Liatis S, Matekovits H, Migdalis I. Pseudomonas fluorescens cutaneous abscess and recurrent bacteremia following a dog bite. Int J Dermatol. 2005;44(4):347–9.
17 Foreman NK, Wang WC, Cullen EJ Jr, Stidham GL, Pearson TA, Shenep JL. Endotoxic shock after transfusion of contaminated red blood cells in a child with sickle cell disease. Pediatr Infect Dis J. 1991;10(8):624–6.
18 Rais-Bahrami K, Platt P, Naqvi M. Neonatal pseudomonas sepsis: even early diagnosis is too late. Clin Pediatr (Phila). 1990;29(8):444.
19 Sarubbi FA Jr, Wilson B, Lee M, Brokopp C. Nosocomial meningitis and bacteremia due to contaminated amphotericin B. JAMA. 1978;239(5):416–8.
20 Thangkhiew I. Successful treatment with ceftazidime of a Pseudomonas fl uorescens chest infection in a myasthenic patient. J Antimicrob Chemother. 1986;18(3):428–9.
21 Whyte A, Lafong C, Malone J, Golda BP. Contaminated lithium heparin bottles as a source of pseudobacteraemia. J Hosp Infect. 1999;42(4):342–3.
22 Namnyak S, Hussain S, Davalle J, Roker K, Strickland M. Contaminated lithium heparin bottles as a source of pseudobacteraemia due to Pseudomonas fluorescens. J Hosp Infect. 1999;41(1):23–8.
Received November 12, 2016
Accepted after revision March 5, 2017
10.5847/wjem.j.1920–8642.2017.02.013
Takeshi Nishimura, Email: kogushi1@msn.com
 World journal of emergency medicine2017年2期
World journal of emergency medicine2017年2期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Information for Readers
- World Journal of Emergency Medicine
- Acute airway emergency caused by an organic foreign body located in the laryngeal mucosa
- An unusual case of renal calculi leading to myocardial infarction and cardiogenic shock
- Diverse coagulopathies in a rabbit model with different abdominal injuries
