基底節區急性腦梗死M1段血管斑塊的T1W-3D-VISTA診斷研究
趙慶龍,劉天怡,楊詩琪,李露露,劉鵬飛*,李國忠,王巍,崔英哲
基底節區急性腦梗死M1段血管斑塊的T1W-3D-VISTA診斷研究
趙慶龍1,劉天怡2,楊詩琪2,李露露1,劉鵬飛1*,李國忠2,王巍1,崔英哲1
目的利用T1W 3D-VISTA磁共振成像序列對基底節區急性缺血性腦卒中患者大腦中動脈M1段血管斑塊分布、信號以及相關臨床特點進行分析。材料與方法對MR DWI診斷為大腦中動脈供血區急性缺血性腦卒中的患者行顱內動脈MRA、大腦中動脈T1W 3D-VISTA掃描,根據梗死部位將患者分為基底節組(基底節區/基底節區合并基底節區外腦梗死)和非基底節組(不包含基底節區腦梗死),研究兩組患者梗死同側斑塊在M1段血管壁的分布,斑塊與胼胝體相對信號強度比值(contrast ratio,CR),以及相關臨床特點分析。結果52例急性大腦中動脈供血區腦梗死伴有同側中動脈粥樣硬化斑塊患者(基底節組:30例,非基底節組:22例),一共1560幅圖像被研究,其中251幅圖像包含斑塊,基底節組的上側壁斑塊所占比例(37.74%)較非基底節組(10.26%)大,差異有統計學意義(P=0.004),基底節組的下側(26.42%)及腹側(13.21%)斑塊所占比例較非基底節組的下側(48.72%)及腹側(33.33%)斑塊所占比例小,差異有統計學意義(P值分別為0.047,0.039)。基底節組斑塊相對信號強度(CR)較非基底節組小(均值分別為0.84,0.92),差異有統計學意義(P=0.001)。兩組之間相關臨床因素(年齡、性別、高血壓、糖尿病、血脂異常、吸煙、飲酒、BMI、入院24 h NIHSS評分、卒中家族史)比較差異無統計學意義(P>0.05)。結論T1W-3D-VISTA序列可以檢測大腦中動脈斑塊的分布及相對信號強度,與非基底節區急性腦梗死患者相比,基底節區急性腦梗死患者腦中動脈M1段斑塊更多分布于上側壁,下側及腹側壁相對較少,基底節區急性腦梗死患者中動脈斑塊相對更穩定。
腦梗塞;磁共振成像;大腦中動脈;斑塊,動脈粥樣硬化
趙慶龍, 劉天怡, 楊詩琪, 等. 基底節區急性腦梗死M1段血管斑塊的T1W-3DVISTA診斷研究. 磁共振成像, 2017, 8(1): 17-21.
急性缺血性腦卒中是一種好發于中老年患者的具有高致死率和致殘率的疾病。研究顯示,與歐美國家的常由顱外血管疾病引起腦卒中不同,亞洲人群由于人種、環境、飲食等多種原因,致使顱內動脈粥樣硬化引起的缺血性腦卒中占有更大的比重[1]。醫學影像技術的進步,特別是磁共振血管高分辨技術的快速發展[2],使從病因學角度評估顱內動脈粥樣硬化的各種特征成為可能。筆者利用T1W 3D-VISTA磁共振成像序列來研究基底節區急性腦梗死患者大腦中動脈M1段斑塊的具體分布、信號特點以及對相關臨床特點進行分析。
1 材料與方法
1.1 研究對象
連續搜集哈爾濱醫科大學附屬第一醫院神經內科2015年10月至2016年9月間52例經DWI診斷為急性大腦中動脈供血區腦梗死,且經MRA及T1W 3D-VISTA證實梗死同側伴有大腦中動脈M1段動脈硬化斑塊存在的患者,其中男性37例,女性15例,平均年齡(59.21±10.96)歲。52例患者中,包含基底節區組30例(基底節區/基底節區合并基底節區外腦梗死),非基底節區組22例(不包含基底節區梗死),共有1560幅圖像被研究,其中251幅圖像包含斑塊(基底節組147幅,非基底節組104幅),相關臨床特征信息被采集分析(表1),斑塊以分布在中動脈M1段的上側壁,下側壁,腹側壁及背側壁在兩組中分別被對比分析,每個斑塊以在各象限分布情況分別計入上、下、腹、背各組,當斑塊分布在兩個或兩個以上象限時,則該斑塊所在的每個象限計數均加一(圖1);因為胼胝體組織結構相對穩定,斑塊的信號強度按其與同次檢查中同一患者胼胝體信號間的比值(CR)來表示。所有患者都進行了頭部DWI、MRA、T1W-3D-VISTA及頸內動脈超聲掃描。所有患者都簽署了知情同意書。
1.2 入組條件
(1) DWI確診為急性大腦中動脈供血區腦梗死;(2)梗死同側頸內動脈經超聲檢查狹窄率<50%;(3)排除心臟疾病患者;(4)圖像質量能夠滿足斑塊診斷要求。
1.3 檢查方法
所有患者均使用Philips公司生產的Achieva 3.0 T磁共振掃描儀,16通道標準頭部正交線圈。所有患者均在入院3 d內進行了DWI掃描,然后先行3D-TOF MRA掃描,之后利用MRA圖像定位進行大腦中動脈T1W 3D-VISTA掃描。DWI參數如下:TR 2170 ms,TE 45 ms,FOV 230 mm× 230 mm×119 mm,層厚4 mm,矩陣112×89;3D-TOF MRA參數:TR 25 ms,TE 3.5 ms,FOV 180 mm×180 mm×85 mm,層厚 1.4 mm,矩陣256×256;T1W 3D-VISTA參數:TR 800 ms,TE 18 ms,FOV 130 mm×130 mm×40 mm,層厚0.6 mm,矩陣330×300。
1.4 圖像分析
圖像采集完成后傳輸到Achieva副臺后處理工作站進行處理,T1W 3D-VISTA圖像沿大腦中動脈M1段短軸方向進行重建。每一名患者的圖像均由2名從事MRI診斷工作10年以上的影像診斷醫師進行盲法評片,兩個人都不知道患者的臨床信息,觀測梗死位置,斑塊在血管壁上側、下側、腹側及背側的具體分布。在斑塊信號最高處選取0.1 mm2感興趣區,每處測三次取均值,沿胼胝體輪廓選取感興趣區(圖2),計算斑塊與胼胝體信號的比值(contrast ratio,CR)。意見不一致時協商解決。T1W 3D-VISTA圖像質量分為4級:1級,圖像不能顯示血管壁;2級,血管壁可見,但管壁結構和管壁、管腔輪廓模糊;3級,管壁結構顯示清楚,僅局部略模糊;4級,管壁結構及管腔、管壁輪廓均顯示清晰。圖像質量分級≤2級的患者予以排除。排除2例圖像質量分級≤2級患者;排除一例梗死同側伴有大腦中動脈夾層患者。
1.5 統計分析
計數資料采用百分比的表達形式,計量資料采用平均值±標準差的形式,計數資料組間比較采用卡方檢驗,計量資料組間比較采用獨立樣本t檢驗,P<0.05為差異有統計學意義。應用SPSS 19.0統計軟件進行數據處理。
2 結果
最終符合標準的患者共52例,基底節組患者有30例,非基底節組有22例,本研究中僅有1例大腦中動脈狹窄率大于50%。所有52例患者一共1560幅圖像被研究,其中251幅圖像包含斑塊(基底節組:147幅,非基底節組:104幅),基底節組的上側壁斑塊所占比例(37.74%)較非基底節組(10.26%)大,差異有統計學意義(P=0.004),基底節組的下側(26.42%)及腹側(13.21%)斑塊所占比例較非基底節組的下側(48.72%)及腹側(33.33%)斑塊所占比例小,差異有統計學意義(P值分別為0.047,0.039),基底節組及非基底節組背側壁斑塊所占比例分別為22.64%及7.69%,差異無統計學意義(P=0.085)。基底節組及非基底節組斑塊相對信號強度(CR)均值分別為0.84 (0.76~0.99),0.92 (0.81~1.06),基底節組斑塊相對信號強度低于非基底節組,差異有統計學意義(P=0.001;圖3)。所有52例患者中,男性(37例,71.2%)及高血壓患者(32例,61.5%)所占比例較大,其余臨床相關因素(糖尿病14例,26.9%;血脂異常21例,40.4%;吸煙19例,36.5%;飲酒18例,34.6%;卒中家族史13例,25.0%)所占比例較小,基底節組與非基底節組之間相關臨床因素(年齡、性別、高血壓、糖尿病、血脂異常、吸煙、飲酒、BMI、入院24 h NIHSS評分、卒中家族史)比較差異無統計學意義(P>0.05)(表1)。
3 討論
大腦中動脈供血區缺血性腦梗死病因復雜,而腦血管病在其發病的病因中占有越來越大的比重[3]。驗尸報告表 明 ,90% 的 動脈粥樣硬化性腦梗死患者都伴有顱內血管的粥樣硬化斑塊存在,43.2%的腦梗死患者伴有動脈粥樣硬化所致管腔狹窄[4],這說明腦動脈粥樣硬化斑塊的形成、發展和破裂很可能是誘發其相應供血區缺血性腦卒中的重要原因之一[5]。
以現有的影像診斷技術來研究腦卒中患者顱內血管動脈粥樣硬化性改變,有MRA、CTA、DSA、超聲等檢查手段,在這些檢查中,超聲由于顱骨的存在,所以在顱內血管檢測上受到了極大的限制;MRA及CTA只能根據血流的流動變化來檢測管腔內情況,對血管腔狹窄程度較輕的或者斑塊正性重構較好[6]的血管壁病變則難以發現;CTA對于斑塊的鈣化及新鮮出血敏感[7],而對不含鈣化或新鮮出血的斑塊則難以分辨,而且顱內動脈管徑較細,斑塊較小,以CTA的分辨率往往難以做出明確診斷。DSA在判斷是否狹窄及小血管顯示上更加精確[8],而無法從病因學上診斷狹窄處的具體變化,如斑塊在血管壁橫斷面的具體分布、偏心性還是向心性、斑塊的穩定性以及與附近穿支血管的關系等,這些因素與腦梗死發生之間都存在關聯,對臨床診斷與治療具有指導性的意義。T1W 3D-VISTA序列由于自身特性,能夠抑制血流信號,對斑塊及血管壁輪廓顯示清晰,同時易于發現動脈夾層及動脈瘤等其他病因[9-10],相對于傳統的MRA、CTA及DSA等檢查手段,能夠從病因角度更好地對腦血管病作出診斷。顯微解剖學研究表明,大腦中動脈穿支動脈多呈直角自大腦中動脈M1段的上壁和后側壁發出,從主干發出后呈梳齒狀平行排列進入前穿質[11]。本研究結果顯示斑塊主要位于下側管壁,即腦穿支開口的對側,這與以往的文獻報道接近[12],且這種分布與身體中其他大血管動脈斑塊分布情況類似,如頸動脈分叉處,由于血流動力學變化,擾流和低壁面切應力形成等因素更容易形成斑塊及促進斑塊的進展[13]。本研究中,基底節組腦梗死患者上側壁斑塊比例明顯多于非基底節組,這可能是由于這些斑塊離穿支動脈口近,而位于穿支動脈開口附近的斑塊無論引起血流異常或者繼續生長、破裂都更易造成穿支的血流變化,繼而造成基底節區腦梗死。Zhao等[14]也報道與非癥狀患者相比,出現癥狀患者的斑塊會更多地位于大腦中動脈管壁的上側。
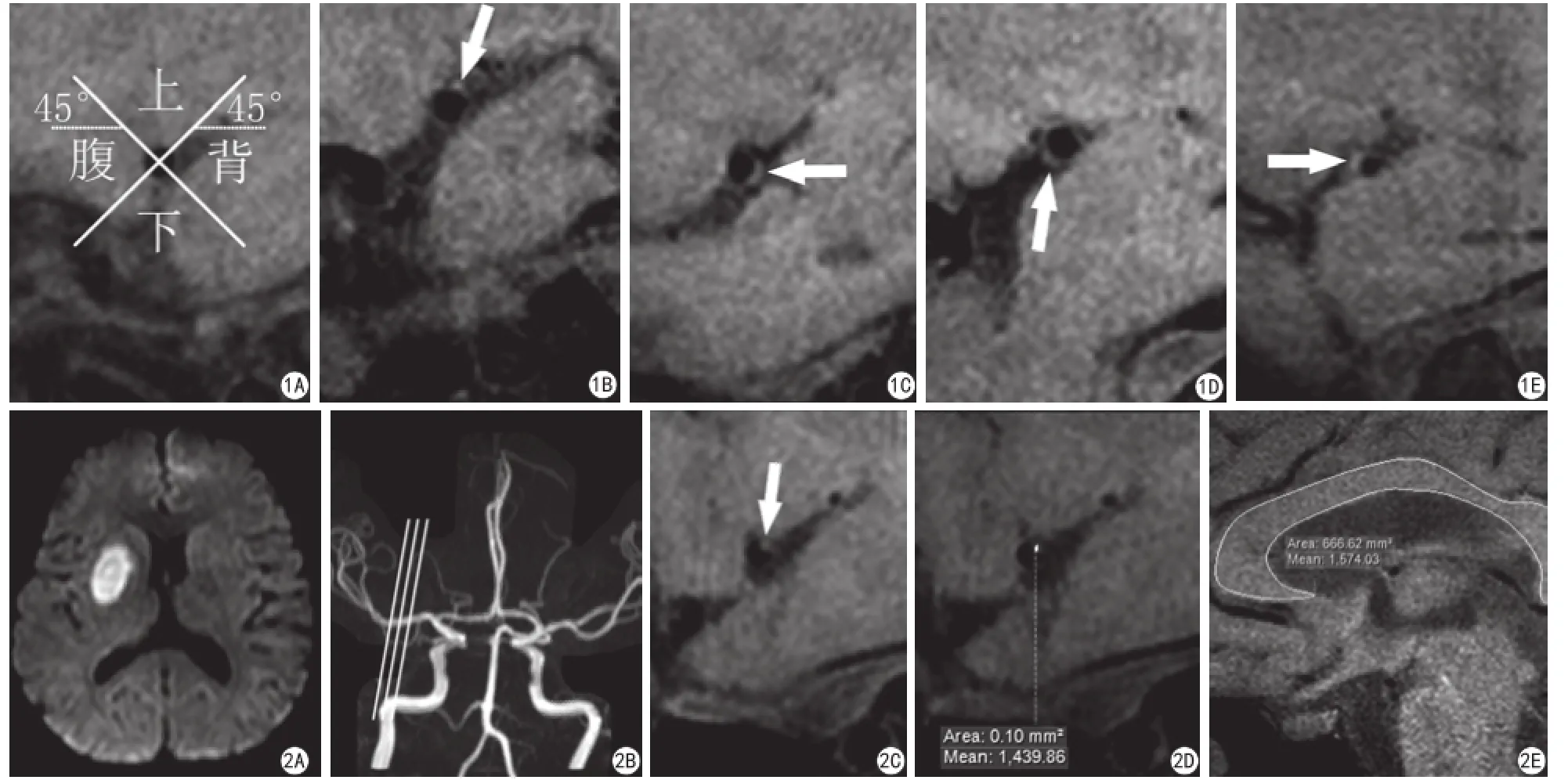
圖1 大腦中動脈斑塊在上、下、腹、背側的分布劃分(A),箭所示為分別在上、背、下、腹側的典型斑塊(B~E) 圖2 典型右側基底節區急性腦梗死患者,女,51歲,DWI上右側基底節區明顯高信號(A),3D-TOF MRA像未見異常狹窄征象(B),梗死同側右側大腦中動脈M1段T1W-3DVISTA掃描可見管壁上側斑塊,CR=0.91(C~E);動脈管壁斑塊及胼胝體信號測量:分別選取感興趣區(D~E)Fig. 1 The alignment grid demonstrates the dividing method of the distribution of middle cerebral artery plaques (A) and the arrow shows examples of plaques involving the superior, dorsal, inferior, or ventral wall, respectively (B—E). Fig. 2 A typical patient with acute cerebral infarction of right basal ganglia region, female, 51 years old. The infarction is revealed on diffusion-weighted images (A). 3D-TOF MRA shows no obvious abnormal signs of stenosis (B). A ipsilateral plaque of the superior wall whose CR is 0.91 is observed on T1W-3D-VISTA (C—E). The method of measurement of plaques and the corpus callosum: select the ROI, respectively (D—E).
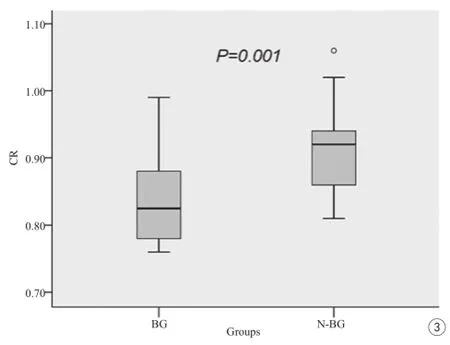
圖3 基底節組與非基底節組大腦中動脈M1段斑塊在T1WI 3D-VISTA上的相對信號強度(CR)。在T1WI 3D-VISTA上,基底節組斑塊相對信號強度(CR)均值低于非基底節組Fig. 3 The relative signal intensity of plaques of BG and N-BG on T1WI 3D-VISTA at M1. On T1WI 3D-VISTA, the mean of CRs of the plaques of BG was lower in the M1 segment than that in the N-BG.
血管壁斑塊是否穩定決定于其組織成分,含有斑塊內出血及脂質核心的斑塊相對更不穩定[15]。相對于顱外血管斑塊,顱內血管斑塊成分分析的影像診斷過去一直是難題。近年來磁共振高分辨序列對顱內動脈斑塊組織成分的信號表現的研究發展迅速[2], 之 前 文 獻 報 道 磁 共 振 高 分辨血管成像T1WI上斑塊信號強度越高往往更易合并斑塊內出血或脂質核心[16-17],這是易損斑塊的常見特征,本研究結果顯示基底節組患者M1段血管壁斑塊相對信號強度小于非基底節區組,這表明本研究中基底節組腦梗死患者斑塊相對更穩定。
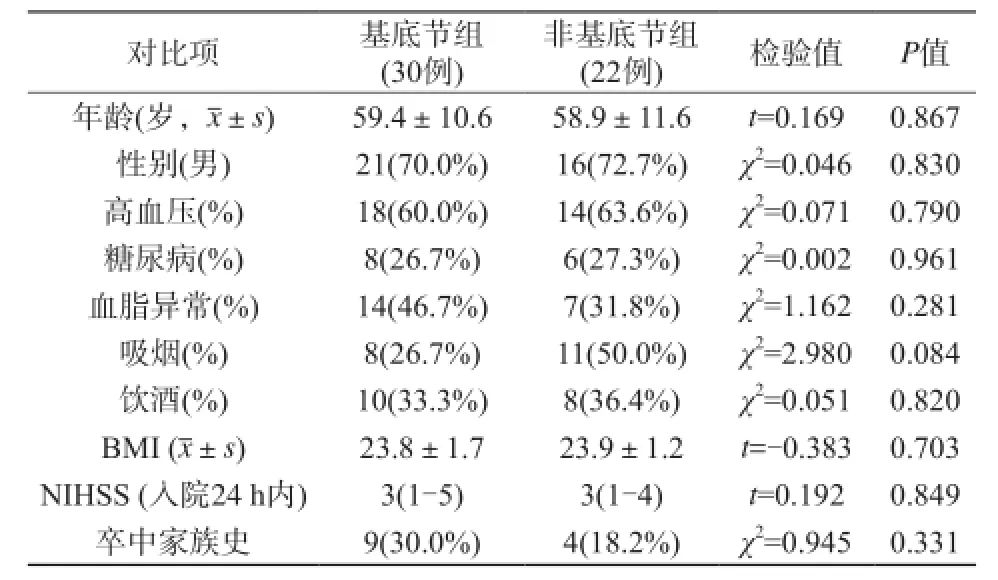
表1 基底節組和非基底節組相關臨床特點比較Tab.1 The comparison of clinical characteristics between BG and N-BG
本研究顯示高血壓患者所占比例較大,以往研究發現高血壓引起的腦血管病可引起腦卒中、腔梗及腦微出血[18-19]等多種急慢性腦組織損害,是動脈粥樣硬化及斑塊形成的高危風險因素,而血壓的突然升高或降低可能是引起急性腦血管病的病因之一。Mia-Jeanne等[20]也指出高血壓、血脂異常及吸煙是動脈粥樣硬化斑塊形成及心腦血管病發生的重要危險因素,然而本研究中血脂異常及吸煙患者所占比例較小,這可能與樣本量較小和患者出現癥狀后調節自身生活習慣及用藥治療有關。本研究中男性患者占有較大比例,糖尿病、肥胖、飲酒患者比例較小,這可能是由地域、環境及生活習慣導致的。筆者發現基底節組與非基底節組兩組患者之間相關臨床因素比較無明顯差異。
這項研究還有一些不足:(1)研究患者例數少;(2)沒有病理學結果的支持;(3)沒有專業的后處理軟件對圖像進行處理分析。將來我們將繼續入組新的患者,爭取取得相關病理學結果,并計劃引進專業的血管處理軟件,不斷完善研究,這將是我們進一步研究的方向。
總之,T1W 3D-VISTA可以檢測急性中動脈供血區腦卒中患者大腦中動脈的斑塊分布特點與相對信號強度。與非基底節區急性腦梗死患者相比,基底節區急性腦梗死患者腦中動脈M1段斑塊更多分布于上側壁,下側及腹側壁相對較少,基底節區急性腦梗死患者中動脈斑塊相對更穩定。
[References]
[1]Ryu CW, Kwak HS, Jahng GH, et al. High-resolution MRI of intracranial atherosclerotic disease. Neurointervention, 2014, 9(1): 9-20.
[2]Li YD, Zhou ZC, Li R, et al. Current status and progress in magnetic resonance vessel wall imaging. Chin J Magn Reson Imaging, 2016, 7(2): 142-148.李赟鐸, 周賾辰, 李睿, 等. 磁共振血管壁成像技術現狀及進展. 磁共振成像, 2016, 7(2): 142-148.
[3]Yamauchi H, Higashi T, Kagawa S, et al. Chronic hemodynamic compromise and cerebral ischemic events in asymptomatic or remotesymptomatic large-artery intracranial occlusive disease. AJNR Am J Neuroradiol, 2013, 34(9): 1704-1710.
[4]Mazighi M, Labreuche J, Gongora-Rivera F, et al. Autopsy prevalence of intracranial atherosclerosis in patients with fatal stroke. Stroke, 2008, 39(4): 1142-1147.
[5]Gao T, Yu W, Liu C. Mechanisms of ischemic stroke in patients with intracranial atherosclerosis: a high-resolution magnetic resonance imaging study. Exp Ther Med, 2014, 7(5): 1415-1419.
[6]Ryoo S, Lee MJ, Cha J, et al. Differential vascular pathophysiologic types of intracranial atherosclerotic stroke: a high-resolution wall magnetic resonance imaging study. Stroke, 2015, 46(10): 2815-2821.
[7]van den Bouwhuijsen QJ, Bos D, Ikram MA, et al. Coexistence of calcification, intraplaque hemorrhage and lipid core within the asymptomatic atherosclerotic carotid plaque: the Rotterdam study. Cerebrovasc Dis, 2015, 39(5-6): 319-324.
[8]Lescher S, Zimmermann M, Konczalla J, et al. Evaluation of the perforators of the anterior communicating artery (AComA) using routine cerebral 3D rotational angiography. J Neurointerv Surg, 2016, 8(10): 1061-1066.
[9]Sakurai K, Miura T, Sagisaka T, et al. Evaluation of luminal and vessel wall abnormalities in subacute and other stages of intracranial vertebrobasilar artery dissections using the volume isotropic turbospin-echo acquisition (VISTA) sequence: a preliminary study. J Neuroradiol, 2013, 40(1) : 19-28.
[10]Dai SP, Pang J, Dai JR. Findings in magnetic resonance vessel wall imaging of basilar artery dissecting aneurysm. Chin J Magn Reson Imaging, 2016, 7(7): 491-495.戴世鵬, 龐軍, 戴景儒, 等. 基底動脈夾層動脈瘤的磁共振血管壁成像表現. 磁共振成像, 2016, 7(7): 491-495.
[11]Han XH, Li XP, Li P, et al. Microanatomy and angiography control observation of M1 segment of middle cerebral artery and its clinical significance. Chin J Clin Anatomy, 2013, 31(2): 154-157.韓曉紅, 李小鵬, 李培, 等. 大腦中動脈 M1 段的顯微解剖與血管造影對照觀測及臨床意義. 中國臨床解剖學雜志, 2013, 31(2): 154-157.
[12]Xu WH, Li ML, Gao S, et al. Plaque distribution of stenotic middle cerebral artery and its clinical relevance. Stroke, 2011, 42(10): 2957-2959.
[13]Li ZY, Felicia PP, Giulia S, et al. Flow pattern analysis in a highly stenotic patient-specific carotid bifurcation model using a turbulence model. Comp Methods Biomech Biomed Engin, 2015, 18(10): 1099-1107.
[14]Zhao DL, Deng G, Xie B, et al. High-resolution MRI of the vessel wall in patients with symptomatic atherosclerotic stenosis of the middle cerebral artery. J Clin Neurosci, 2015, 22(4): 700-704.
[15]Skagen K1, Skjelland M, Zamani M, et al. Unstable carotid artery plaque: new insights and controversies in diagnostics and treatment. Croat Med J, 2016, 57(4): 311-320.
[16]Yang WQ, Huang B, Liu XT, et al. Reproducibility of high-resolution MRI for the middle cerebralartery plaque at 3 T. Eur J Radiol, 2014, 83(1): e49-e55.
[17]Kashiwazaki D, Akioka N, Kuwayama N, et al. Pathophysiology of acute cerebrovascular syndrome in patients with carotid artery stenosis: amagnetic resonance imaging/single-photon emission computed tomography study. Neurosurgery, 2015, 76(4): 427-433.
[18]Aziz ZA, Lee YY, Ngah BA, et al. Acute Stroke Registry Malaysia, 2010-2014: results from the National Neurology Registry. J Stroke Cerebrovasc Dis, 2015, 24(12): 2701-2709.
[19]Liu PF, Cui YZ, Gao PY, et al. MR-image screening of cerebral microbleeds and analysis of related factors in cerebrovascular disease patients. Chin J Geriat Heart Brain Vessel Dis, 2009, 11(2): 104-107.劉鵬飛, 崔英哲, 高培毅, 等. 腦血管病患者腦微出血磁共振成像篩查及相關因素的分析. 中華老年心腦血管病雜志, 2009, 11(2): 104-107.
[20]Mia-Jeanne VR, Pretorius E. Obesity, hypertension and hypercholesterolemia as risk factors for atherosclerosis leading to ischemic events. Curr Med Chem, 2014, 21(19): 2121-2129.
The diagnostic study of T1-weighted 3D volumetric isotropic TSE acquisition in evaluating characteristics of plaques of middle cerebral artery in acute ischemic stroke of basal ganglia
ZHAO Qing-long1, LIU Tian-yi2, YANG Shi-qi2, LI Lu-lu1, LIU Peng-fei1*, LI Guozhong2, WANG Wei1, CUI Ying-zhe11Department of Magnetic Resonance, the First Affiliated Hospital of Harbin Medical University, Harbin 150001, China
2Department of Neurology, the First Affiliated Hospital of Harbin Medical University, Harbin 150001, China
*
Liu PF, E-mail: liup.fei@163.com
Received 12 Nov 2016, Accepted 10 Dec 2016
Objective:To evaluate the characteristics of plaques of middle cerebral artery (MCA) in acute ischemic stroke of basal ganglia using T1-weighted 3D Volumetric Isotropic TSE Acquisition (T1W 3D-VISTA) and its clinical relevance.Materials and Methods:Patients with acute ischemic stroke of middle cerebral artery territory, which were diagnosed by DWI, underwent both MRA and T1W 3D-VISTA examinations. Patients were divided into two groups according to the distribution of infarction, one contained basal ganglia (BG, basal ganglia/ basal ganglia as well as the area outside of it) and the other did not contain basal ganglia (N-BG). Distribution of blood vessel walls and the contrast ratio (CR) of signal intensity of the plaques to that of the corpus callosum were compared between BG and N-BG and their clinical characteristics were evaluated.Results:Among 52 patients with cerebral infarction and ipsilateral plaques in M1 (BG 30 and N-BG 22), a total of 1560 image slices were studied. Overall, of the 251 slices with identified plaques, the plaques located at superior wall of BG (37.74%) accounted for a higher proportion as compared with N-BG (10.26%)(P=0.004), and the plaques located at inferior wall (26.42%) and ventral wall (13.21%) of BG accounted for a lower proportion as compared with the plaques located at inferior wall (48.72%) and ventral wall (33.33%) of N-BG (P=0.047 and 0.039,respectively). The average signal intensity (CRs) of plaques of BG was lower as compared with plaques of N-BG (mean, 0.84 and 0.92, respectively, P=0.001). The clinical characteristics (including age, gender, hypertension, diabetes, dyslipidemia, smoking, drinking, BMI, NIHSS score within 24 hours after admission, family history of stroke) had no significant difference between BG and N-BG (P>0.05).Conclusion:T1W-3D-VISTA can detect the distribution of arterial atherosclerotic plaques and the relative signal intensity. As compared with plaques of N-BG, the plaques of BG are relatively more stable and account for a higher proportion at superior wall and a lower proportion at inferior wall and ventral wall of MCA M1 segment.
Brain Infarction; Magnetic resonance imaging; Middle cerebral artery; Plaque, atherosclerotic
1. 哈爾濱醫科大學附屬第一臨床醫學院磁共振科,哈爾濱 150001
劉鵬飛,E-mail:liup.fei@163.com
2016-11-12
R445.2;R743.33
A
10.12015/issn.1674-8034.2017.01.005
2. 哈爾濱醫科大學附屬第一臨床醫學院神經內科,哈爾濱 150001
接受日期:2016-12-10

