Effect of motivational interviewing on postoperative weight control in patients with obstructive sleep apnea-hypopnea syndrome
Xiang-Hong Sun, Peng-Shi Xue, Xiang-Xiu Qi, Ling Fan
Xiang-Hong Sun, Department of Critical Care Medicine, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China
Peng-Shi Xue, Department of Cardiology, Shengjing Hospital of China Medical University,Shenyang 110004, Liaoning Province, China
Xiang-Xiu Qi, Ling Fan, Department of Nursing, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China
Abstract
Key words:Obstructive sleep apnea-hypopnea syndrome;Postoperative;Weight control;Motivational interview;Quality of sleep;Patients
INTRODUCTION
Obstructive sleep apnea-hypopnea syndrome (OSAHS) is a disease characterized by recurrent apnea and hypopnea during sleep[1-3].Clinical manifestations include snoring, sleep disturbances, asphyxia or awakening at night, and daytime drowsiness.In severe cases, cognitive decline and behavioral abnormalities may occur[4].The latest research shows that OSAHS is closely related to the occurrence of various diseases,such as hypertension, coronary heart disease, and stroke, which seriously affect the quality of life and longevity of patients[5].Obesity is recognized as one of the important risk factors for the occurrence of OSAHS.The incidence of OSAHS in obese patients is as high as 40% to 75%, and the higher the degree of obesity, that is, the body mass index (BMI), the higher the severity of OSAHS[6-8].At present, noninvasive ventilatorassisted treatment or surgical treatment to remove stenosis or dilation is usually used to relieve the symptoms of repeated complete or incomplete obstruction of the upper airway during the sleep of OSAHS patients[9].However, research has found that surgical treatment can only improve the patient’s anatomical abnormalities to a certain extent and cannot achieve the goal of thorough treatment[10].Additionally, the treatment efficiency of OSAHS patients can gradually decrease over time after surgery[11].Obesity can cause neck crowding, hypertrophy of the tongue, and excessive fat deposition in the uvula and pharyngeal wall[10].If postoperative weight control is not good, some patients with OSAHS will experience rebound symptoms after surgery.Obesity requires comprehensive treatment based on exercise and diet, and if necessary, medication, surgery, or endoscopic ultrasound interventions are required[12-15].Thus, effective lifestyle interventions play an important role in the treatment of OSAHS.
At present, due to the lack of fixed-time intervention and follow-up measures, the compliance of patients with OSAHS is poor[16], resulting in unsatisfactory postoperative weight control.Motivational interviewing (MI) was first proposed by Hettemaet al[17]in 1983.The MI is a patient-centered and guided treatment method.By exploring the internal state of the patient, the patient is made aware of his/her ambivalence, which causes the patient to change his/her behavior, emphasizing respect for the patient’s autonomy[18].Its four core guiding principles involve expressing empathy, developing conflict, avoiding resistance, and supporting selfefficacy[19].At present, MI has been widely used in the management of chronic diseases, such as diabetes, hypertension, weight loss, and pain control, and has achieved good results[20].Our study applied an MI intervention to OSAHS patients’postoperative weight control and achieved good results.
MATERIALS AND METHODS
Research subjects
One hundred obese patients with OSAHS who underwent surgical treatment at Shengjing Hospital of China Medical University from March 2018 to March 2019 were selected as the research subjects.The inclusion criteria were:(1) Patients aged ≥ 18 years and <65 years old;(2) Patients who met the OSAHS diagnostic criteria referring to the "Guidelines for the Diagnosis and Treatment of Obstructive Sleep Apneahypopnea Syndrome (2011 Revised Edition)" by the Sleep-disordered Breathing Group of Chinese Thoracic Society of the Chinese Medical Association[21];(3) Patients whose body mass index (BMI) ≥ 28 kg/m2, complying with the diagnostic criteria for obesity by Chinese Guidelines for the Prevention and Control of Overweight and Obesity in Chinese Adults (Trial) 2003 edition[22];(4) Patients who were willing to receive surgical treatment;and (5) Patients who had a clear awareness and had no obstacles in language communication.The exclusion criteria were:(1) Patients who were treated with a ventilator after surgery;(2) Patients with severe heart, brain, kidney, lung, or limb disorders;and (3) Patients who were participating in other studies.The withdrawal criteria were:(1) Patients who could not continue to participate in the research due to illness, long-term absence, or disease during the study period;(2)Patients who asked to quit actively;and (3) Patients with incomplete clinical data.
妊娠期是否規律補鐵對母嬰血紅蛋白水平和圍產期并發癥的影響 ………………………………………… 譚曉青等(12):1685
Intervention methods
According to a random number table, 100 patients who met the inclusion and exclusion criteria were randomly divided into an intervention group and a control group, with 50 cases in each group.The control group received routine postoperative care, and the intervention group received an MI intervention on the basis of routine care.The MI intervention plan was developed based on the relevant literature and OSAHS disease characteristics, and the plan was revised through the expert meeting method.The intervention time was from the time when the patient was discharged to 6 mo after discharge;the frequency of intervention was 1 time/mo for a total of 6 times.Interventions were completed by systematically trained interviewers and duty nurses.The interviewers were selected from the supervising nurses who had a bachelor’s degree or above and had been working in clinical nursing for more than 5 years.Interventions included face-to-face and telephone interviews.
Control group
The patients in the control group were given general postoperative health education,including knowledge about weight control.Dietary guidance included instruction on maintaining a reasonable weight, controlling nutritional intake, adjusting dietary structure, limiting alcohol consumption, and other dietary adjustments (such as limiting salt intake and increasing dietary fiber intake).Exercise instruction included information on exercise time, exercise goals, exercise items, and precautions.The above health education was conducted before the patients were discharged, and the patients were followed by telephone at 1, 3, and 6 mo after discharge to understand their diet, exercise, and postoperative recovery and to provide guidance.
Intervention group
In addition to regular postoperative health education, patients in the intervention group also received MI interventions developed in advance.Each intervention was performed one-on-one by the interviewer and the patient.Before the intervention, the"Stage Change Assessment Questionnaire" was used to assess which stage of weight management behavior change the patient was in, and corresponding intervention measures were given.The specific intervention plan was as follows.The interviewer informed the patients in the intervention group about the purpose, meaning, and method of the study, obtained the informed consent from the patients and their families, established a good cooperative relationship, and used the Stage Change Assessment Questionnaire to understand the patients’ stage of behavior change, and provided the corresponding intervention responses.The interviewer then proceeded as follows:(1) Pre-intentional stage:Understand the reasons why patients do not have the intention to manage their weight and help them establish motivation for behavior change;help patients realize the benefits of weight management for postoperative recovery;explain the harm of postoperative weight gain to postoperative recovery;and inform patients of ways to gain knowledge about weight management, while strengthening family education;(2) Intentional stage:Understand the specific causes of positive and negative changes in patient behaviors and help patients analyze and overcome ambivalence;guide patients to adjust poor diet and exercise behaviors and establish a good lifestyle;and help patients realize that scientific weight management is their responsibility to optimize the effect of surgery and their own health;(3)Preparation stage:Actively encourage patients to make a commitment to weight management;researchers and patients worked out specific diet and exercise plans, set weight control goals for patients, increased their awareness of self-management, and encouraged family support and participation in supervision;(4) Action stage:Instruct patients to make full use of the surrounding resources and actively seek ways to get help from others;teach patients to avoid stimuli of unhealthy behaviors and increase the implications of healthy behavioral changes;encourage patients to improve their self-monitoring and management capabilities and master solutions to weight management problems;and enhance patients’ confidence in their weight management behaviors;(5) Maintenance stage:Continuously affirm the positive results achieved by the patients’ behavior change and provide appropriate rewards;strengthen the followup and supervision of patients;and strengthen the family and society support to enable patients to adhere to healthy behaviors and avoid behavior regression;and (6)Summary:Discuss and resolve the problems existing in the implementation of MIs for OSAHS patients, identify the gap between their current stage and the expected goals,and assist patients to maintain and execute behavior change plans.After each intervention, the time of the next interview was agreed to according to the evaluation results and the patient’s grasp of the intervention content.If there were no special circumstances, the timing of the intervention would be the first week of each month.The intervention content mainly included disease-related basic knowledge, diet,exercise intervention, emotional intervention, and review guidance.
The pre-intentional and intentional stages had to be face-to-face interviews, each lasting 30 to 45 min.These two interventions were conducted in the 1stand 2ndmonths after discharge.The preparation, action, and maintenance stages could be telephone interviews, each lasting 15 to 20 min, which were carried out in the 3rd, 4th, and 5thmonths after discharge.The summary stage was conducted in the 6thmonth after discharge, lasting 30 to 45 min.It was a face-to-face interview.
Evaluation indicators
The following indicators needed to be evaluated before and after 6 mo of intervention:(1) Obesity-related indicators including weight, BMI, waist circumference, neck circumference, and hip circumference;(2) Postoperative complications including irritating cough, reflux, and foreign body sensation;and (3) Sleep status including Self-Rating Scale of Sleep (SRSS) and Epworth Sleepiness Scale (ESS).SRSS was compiled by Professor Jian-Ming Li[23], and can be used to compare the sleep status assessment of patients before and after treatment.SRSS has a total of 10 items, and each item is rated on a 5-point scale.The higher the score, the more severe the sleep problem.The total score of this scale ranges from 10 to 50 points[23].ESS was developed by the Sleep Research Centre of Epworth Hospital in Melbourne, Australia in 1990.It is an internationally recognized drowsiness assessment scale[24].It consists of 8 questions with a score ranging from 0 to 24 points.An ESS score of ≥ 9 is used as a criterion for screening patients with suspected OSAHS[25].
Statistical analysis
SPSS 24.0 statistical software was used for data processing.The continuous variables are expressed as the mean ± SD, the count data are expressed as percentages, and the comparison between the two groups was analyzed by attest.After the homogeneity test of variance, data with homogeneous variance were tested byttest, and those with heterogeneity of variance were statistically analyzed by the correctedttest.P<0.05 indicated that the difference was statistically significant.
RESULTS
Patient baseline data
A total of 100 patients were included, and 88 patients completed the study.There were 46 patients in the intervention group, including 37 (80.43%) males and 9 (19.57%)females, and 42 patients in the control group, including 38 (90.48%) males and 4(9.52%) females.There was no difference in gender between the two groups (χ2=1.758,P=0.185).There were no significant differences in other baseline data between the two groups of patients (P>0.05) (Table 1).
Comparison of obesity-related indicators between the two groups of patients before and after intervention
After 6 mo of intervention, the weight, BMI, waist circumference, and neck circumference of the patients in the intervention group were significantly improved compared with those in the control group (P<0.05, Table 2).
Postoperative complications of the two groups of patients before and after intervention
In the control group, 10, 9, and 8 patients experienced cough, reflux, and foreign body sensation, respectively, after operation, and in the intervention group, 3, 3, and 4 patients experienced irritating cough, reflux, and foreign body sensation, respectively,within 6 mo after operation.After the MI intervention, the incidence of irritating cough and reflux in patients in the intervention group was significantly lower than that in the control group (P<0.05, Table 3).
Comparison of the sleep status of the two groups of patients before and after intervention
After the intervention, the ESS and SRSS scores of the patients in the intervention group were lower than those in the control group.The sleep of the patients in the intervention group was improved compared with the control group.The difference was statistically significant (P<0.05, Table 4).
DISCUSSION
Effect of MI on postoperative weight improvement in patients with OSAHS
Studies have shown that after receiving conventional postoperative intervention,OSAHS patients’ cognitive and behavioral status with regard to weight control is not ideal[26].In this study, compared with conventional postoperative health education, an MI intervention can better control the weight and BMI of OSAHS patients and reduce waist and neck circumference.Consistent with the results of many studies[27-29],regardless of whether used as an independent treatment or an adjunct method[30], MI can change patients’ lifestyle with regard to weight management and control of the weight and waist and neck circumference of patients with chronic diseases or other related diseases.Exercise and diet are the keys to reducing body mass.MI follows the principles of a healthy and reasonable diet, promotes the formulation of healthy diet recipes for patients, controls patients’ intake of fat and high-calorie food, maintains patients’ balanced diet, and better regulates their weight and waist and neck circumference[31].In addition, through the MI with the patient, emphasis is placed on the harm of obesity to the prognosis of the disease, mobilizing the patient’s enthusiasm for exercise, increasing the amount of exercise, and enabling the patient to record and maintain his/her own condition so that the patient changes from the initial passive exercise to active exercise.During the intervention process, MI can alleviate the patient’s resistance, improve the patient’s cooperation enthusiasm, and achieve the effect of controlling and maintaining weight.
Impact of MI in reducing complications
Common short-term complications after surgery in patients with OSAHS include throat paresthesia, swallowing pain, and long-term diet reflux[32].This study found that three major complications, irritating cough, reflux, and foreign body sensation,occurred within 6 mo after surgery in the two groups of patients.After effective MI intervention, the incidence of complications in the intervention group was lower than that in the control group (P<0.05).At present, most clinical studies have onlyobserved physiological parameters such as body weight, waist and neck circumference, and sleep in patients with OSAHS, and often ignore the occurrence of complications.Complications, as important indicators of long-term curative effect of surgery, seriously affect patients’ quality of life and prognosis.Studies show that MI plays a more active role in controlling the incidence of irritating cough and other complications in patients, which may have a strong correlation with the improvement in the patients’ awareness of disease control and management as well as selfmanagement ability.Effective postoperative upper airway management can greatly reduce the incidence of postoperative complications[33].Under the intervention of the MI, the researchers listed negative and positive cases to enhance patients’ belief and enthusiasm for postoperative recovery, improve patients’ self-management ability,and further reduce the incidence of complications.
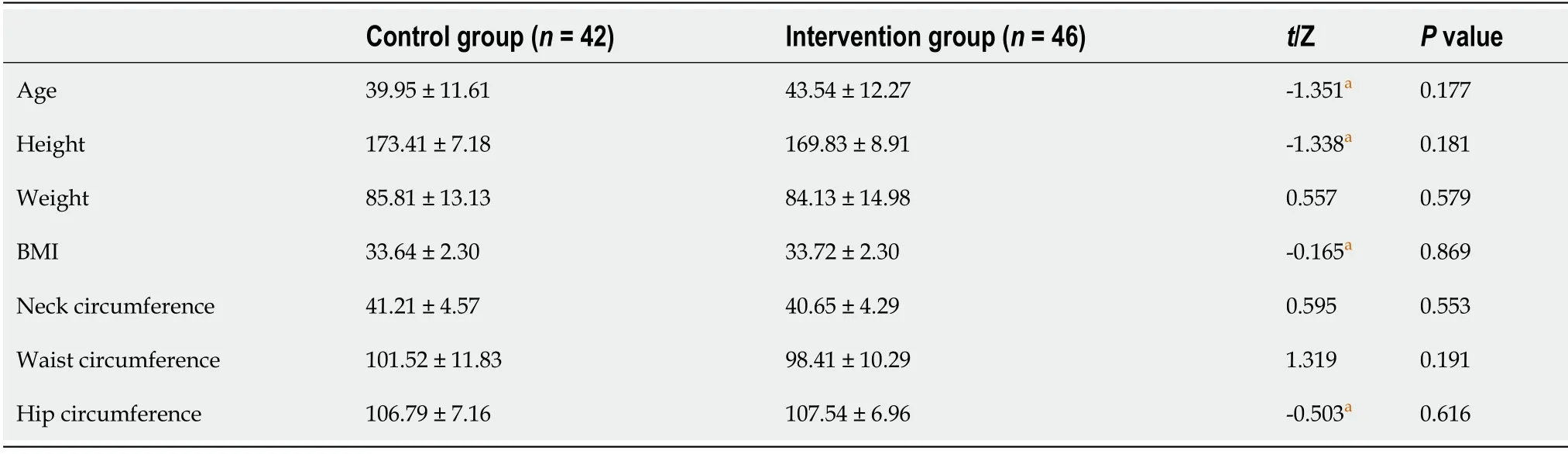
Table 1 Comparison of baseline data between the two groups of patients (mean ± SD)

Table 2 Comparison of obesity-related indicators between the two groups of patients before and after intervention (mean ± SD)
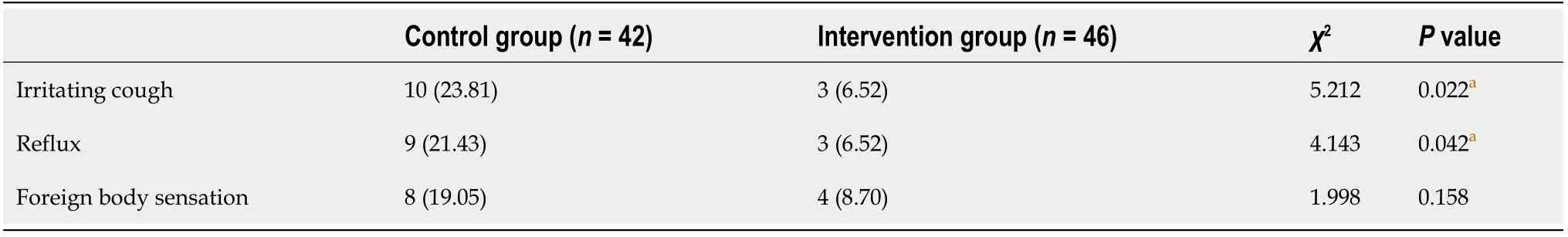
Table 3 Complications in the two groups of patients, n (%)
Impact of MI in improving sleep
This study showed that the drowsiness alleviated and the sleep quality improved in both groups of patients at 6 mo after surgery, but the MI intervention was moreeffective than the conventional postoperative intervention (P<0.05).This proves that on the basis of surgical treatment, effective healthy lifestyle interventions for patients with OSAHS can alleviate the symptoms of drowsiness;patients feel energetic, and their mental state is significantly improved, which is similar to the research results of Baiet al[34]and Tianet al[35].Through the MI with the patient, the researcher informs the patient that improvement in sleep quality can play a certain auxiliary role in weight loss and guide the patient to form a good lifestyle, such as ensuring sufficient sleep,forming a regular schedule, and changing sleeping position.In this process,researchers implement effective behavioral interventions.In addition, researchers use MI to effectively monitor patients to maintain long-term healthy behaviors and avoid behavioral regressions.Compared with routine follow-up, patients can more easily form and maintain good living habits with long-term effective interventional followup.
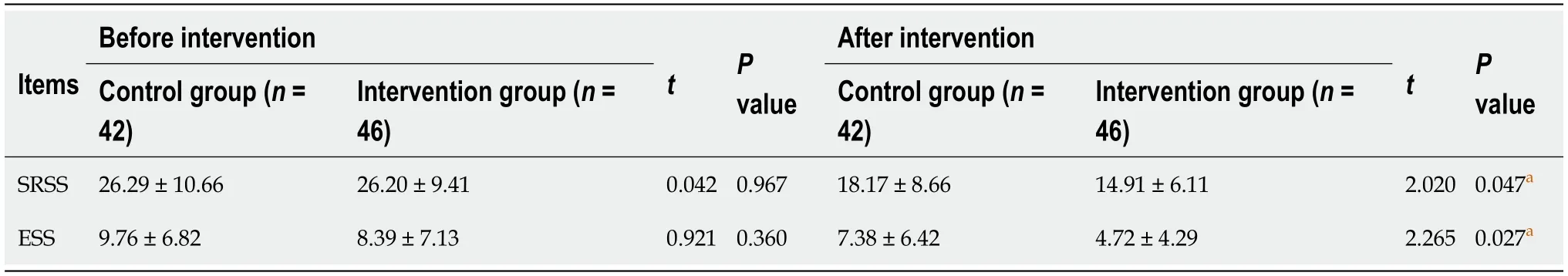
Table 4 Comparison of sleep status of the two groups of patients before and after the intervention (points, mean ± SD)
In summary, routine intervention after surgery can only inform or guide the patient how to enact the required changes;however, it does not consider whether the patient is willing to change and the problems that may occur during the changes.Conventional intervention often ignores the important role of patients’ motivation and beliefs for behavior change.Although routine intervention can change the status of patients’ knowledge and behaviors early after surgery, the long-term behavior change is not good[36].Based on the positive results of this study, compared with postoperative conventional interventions, the MI intervention in this study emphasizes reaching a cooperative and equal relationship with patients, making patients aware of the importance of weight control and the dangers of being overweight, motivating behavior change, and helping patients resolve the difficulties and ambivalence encountered in the process of behavior change so that they can establish health beliefs and enhance self-efficacy, thereby promoting changes in patients’ long-term behaviors and the formation of good living habits.As a result, the patient’s weight is better controlled, complications are reduced, and long-term efficacy is improved after surgery.Therefore, MI can be well applied to postoperative follow-up and intervention in patients with OSAHS.
ARTICLE HIGHLIGHTS
Research background
If postoperative weight control is not good, some patients with obstructive sleep apnea-hypopnea syndrome (OSAHS) will experience rebound symptoms after surgery.Currently, the common measures for controlling the weight mainly include diet control, increase exercise and so on.Conventional postoperative intervention focuses on the health education, but the compliance of patient weight control after surgery is poor.
Research motivation
Motivational interviewing (MI) could mobilize the initiative of obese patients with OSAHS after surgery, making them fully understand the harm of obesity.Also, by combining with personalized weight control scheme to effectively control weight, the surgical treatment effect of obese OSAHS patients could be well promoted, thus finally reducing and controlling the occurrence of complications.
Research objectives
This research aimed to explore the effect of motivational interviewing on postoperative weight control in obesity patients with OSAHS.
Research methods
A case-control study was performed.From March 2018 to March 2019, 100 postoperative patients with OSAHS were randomly divided into an intervention group and a control group, with 50 cases in each group.The control group was given routine health education after the operation;in addition to the regular health education, the intervention group was given MI according to a predetermined plan.Obesity-related indicators, postoperative complications, and the sleep status of both groups were evaluated before and 6 mo after the intervention.
Research results
Patients in the intervention group had significantly improved body weight, BMI, and waist and neck circumference compared with patients in the control group.Regarding complications at 6 mo after operation, the incidence of cough and reflux in patients in the intervention group was significantly lower than that in the control group.In addition, the Epworth Sleepiness Scale and Self-Rating Scale of Sleep scores of patients in the intervention group were lower than those in the control group, and the sleep status of patients in the intervention group was improved.
Research conclusions
MI intervention has a significant advantage compared to the postoperative routine health education.It can greatly change the lifestyle of OSAHS patients, further control the postoperative weight of patients, reduce the occurrence of complications in patients, improve patients’ quality of sleep, and improve long-term postoperative efficacy.
Research perspectives
Our research results show that MI for 6 mo could effectively control the postoperative weight of obesity patients with OSAHS, and reduce the complications.If the long-term intervention effect is to be observed, the follow-up time should be extended.
 World Journal of Clinical Cases2020年15期
World Journal of Clinical Cases2020年15期
- World Journal of Clinical Cases的其它文章
- Facial and bilateral lower extremity edema due to drug-drug interactions in a patient with hepatitis C virus infection and benign prostate hypertrophy:A case report
- Total laparoscopic segmental gastrectomy for gastrointestinal stromal tumors:A case report
- COVID-19 with asthma:A case report
- Computed tomography, magnetic resonance imaging, and Fdeoxyglucose positron emission computed tomography/computed tomography findings of alveolar soft part sarcoma with calcification in the thigh:A case report
- Acute suppurative oesophagitis with fever and cough:A case report
- Coexistence of ovarian serous papillary cystadenofibroma and type A insulin resistance syndrome in a 14-year-old girl:A case report
