乳癌病人術前外周血SII和ELR與預后的關系
金麗濤 李福年
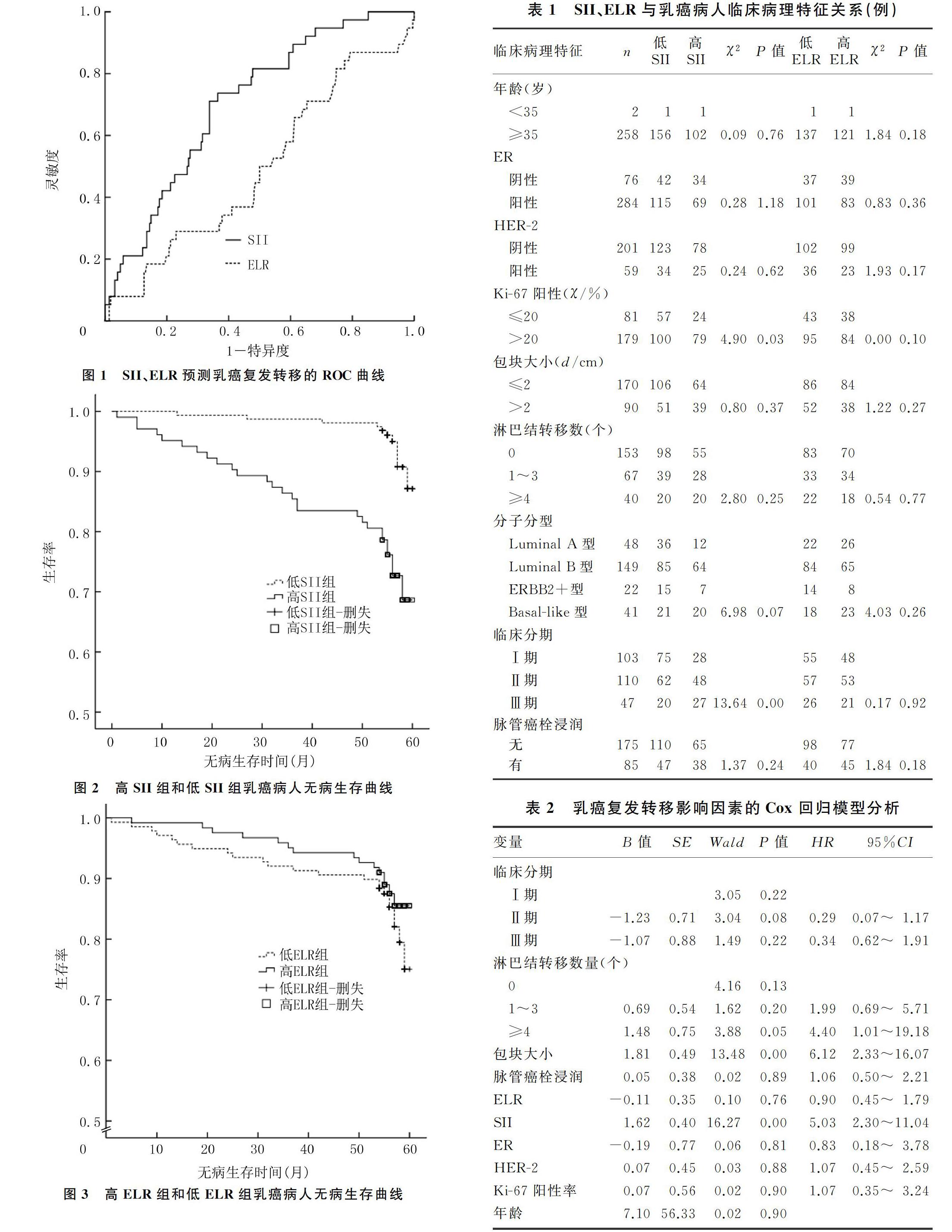
[摘要] 目的 探討乳癌病人術前外周血系統免疫炎癥指數(SII)、嗜酸性粒細胞-淋巴細胞比率(ELR)與預后的關系。方法 回顧性分析2013—2014年我院治療的260例女性乳癌病人的臨床病理資料,采用受試者工作特征(ROC)曲線確定SII、ELR最佳截斷值,將病人分為高SII和低SII組、高ELR和低ELR組,比較各組臨床病理特征,采用Kaplan-Meier法繪制病人生存曲線,Log-rank檢驗分析生存差異,Cox回歸模型對乳癌病人預后影響因素進行分析。結果 SII水平高低與臨床分期(TNM)、Ki-67陽性率密切相關(χ2=13.64、4.90,P<0.05),ELR水平高低與各臨床病理特征無相關性(P>0.05)。乳癌病人5年無病生存率為85.40%,高SII組和低SII組5年無病生存率分別為73.80%和93.00%,差異有統計學意義(χ2=20.84,P<0.05);高ELR組和低ELR組的5年無病生存率分別為87.70%和83.30%,差異無統計學意義(χ2=0.96,P>0.05)。Cox回歸分析顯示,SII(HR=5.03,95%CI=2.30~11.04,P<0.05)、包塊大小(HR=6.12,95%CI=2.33~16.07,P<0.05)、淋巴結轉移數量(HR=4.40,95%CI=1.01~19.18,P<0.05)對乳癌病人復發轉移影響有統計學意義。結論 術前SII可作為預測乳癌預后的獨立因素,高SII值提示預后不良;而ELR不能作為預測乳癌預后的因素。
[關鍵詞] 乳房腫瘤;系統免疫炎癥指數;嗜酸性粒細胞-淋巴細胞比率;預后
[中圖分類號] R737.9 ?[文獻標志碼] A ?[文章編號] 2096-5532(2020)05-0571-05
doi:10.11712/jms.2096-5532.2020.56.129 [開放科學(資源服務)標識碼(OSID)]
[ABSTRACT] Objective To investigate the association of preoperative systemic immune-inflammation index (SII) and eosinophil-lymphocyte ratio (ELR) in peripheral blood with the prognosis of breast cancer patients. ?Methods A retrospective analysis was performed for the clinicopathological data of 260 female patients with breast cancer who underwent treatment in our hospital from 2013 to 2014. The receiver operating characteristic (ROC) curve was used to determine the optimal cut-off values of SII and ELR, and then the patients were divided into high and low SII groups and high and low ELR groups. The clinicopathological features were compared between groups. The Kaplan-Meier method was used to plot survival curves, the Log-rank test was used for survival difference analysis, and the Cox regression model was used to investigate the influencing factors for the prognosis of patients with breast cancer. ?Results The level of SII was closely associated with clinical stage (TNM) and positive rate of Ki-67 (χ2=13.64,4.90;P<0.05), while there was no correlation between the level of ELR and clinicopathological features (P>0.05). The 5 year disease-free survival rate was 85.40% for all 260 breast cancer patients, and there was a significant difference in 5 year disease-free survival rate between the high SII group and the low SII group (73.80% vs 93.00%,χ2=20.84,P<0.05), while there was no significant difference in 5 year disease-free survival rate between the high ELR group and the low ELR group (87.70% vs 83.30%,χ2=0.96,P>0.05). The Cox regression analysis showed that SII (HR=5.03,95%CI=2.30-11.04,P<0.05), tumor size (HR=6.12,95%CI=2.33-16.07,P<0.05), and number of lymph node metastases (HR=4.40,95%CI=1.01-19.18,P<0.05) had significant influence on recurrence and metastasis in patients with breast cancer. ?Conclusion Preoperative SII can be used as an independent predictive factor for the prognosis of breast cancer, and high SII value indicates poor prognosis, while ELR cannot be used as a predictive factor for the prognosis of breast cancer.
SII、ELR是基于中性粒細胞、淋巴細胞、血小板計數的綜合指標,SII、ELR影響惡性腫瘤病人的預后與外周血中性粒細胞、血小板、淋巴細胞等指標的變化有關。近年研究發現,中性粒細胞與腫瘤之間存在密切關系,中性粒細胞具有腫瘤促進作用。其腫瘤促進作用主要表現在以下方面:①腫瘤細胞異位分泌粒系集落刺激因子導致中性粒細胞數量增加,增多的中性粒細胞分泌大量血管內皮生長因子,為腫瘤細胞生長和增殖提供有利條件[10-11];②中性粒細胞釋放中性粒細胞彈性蛋白酶,其進入腫瘤細胞內涵體直接誘導腫瘤細胞增殖[12];③中性粒細胞在TGF-β刺激下釋放一氧化氮合成酶或精氨酸酶,抑制CD8+T淋巴細胞抗腫瘤反應,促進腫瘤增殖、轉移[13-15]。
有研究顯示,血小板不僅參與機體生理性凝血過程,還參與了腫瘤的生長與擴散,血小板對腫瘤生長、擴散的影響主要表現在以下方面[16-17]:腫瘤細胞可以通過直接接觸或釋放ADP、凝血酶、TXA2或腫瘤相關蛋白酶等刺激血小板活化,活化的血小板能釋放溶血磷脂酸,溶血磷脂酸會增強腫瘤細胞的侵襲性和血管通透性;同時,血小板通過血小板衍生的TGF-β下調NK細胞活化的免疫受體自然殺傷細胞活化受體2D(NKG2D)表達,抑制NK細胞活性,促進腫瘤生長、增殖[18-21]。晚期惡性腫瘤病人常伴血小板增多。
淋巴細胞是機體細胞免疫的主要成分,在腫瘤免疫監視中發揮巨大作用,腫瘤浸潤性淋巴細胞減少,相應免疫應答激活減少,機體抗腫瘤作用下降,增加腫瘤轉移和復發風險[22]。惡性腫瘤促進了炎癥反應,同時持續的機體炎癥狀態為惡性腫瘤進展提供了適宜的微環境[23-24]。基于上述機制,較高的SII促進腫瘤血管生成、侵襲和轉移,從而導致乳癌病人預后較差。
本研究結果顯示,ELR與乳癌病人預后無相關性,可能與嗜酸性粒細胞對腫瘤進展發揮雙重作用有關。有研究表明,嗜酸性粒細胞能夠誘導各種腫瘤細胞死亡,其機制是嗜酸性粒細胞具有與細胞毒性T淋巴細胞相同的受體和遞質,因而能發揮抗腫瘤的作用。又有研究表明,嗜酸性粒細胞可能通過合成多種促血管生成因子(如血管內皮生長因子、成纖維細胞生長因子-2和IL-8)促進腫瘤生長[25-29]。
本文研究分析了SII、ELR與乳癌病人臨床病理特征的關系,結果顯示,SII與乳癌病人的Ki-67陽性率和臨床分期相關,提示SII參與了腫瘤的發生發展;而ELR與各臨床病理特征無相關性。本研究進一步分析顯示,術前ELR與乳癌病人無病生存率無相關性,但SII與乳癌病人的無病生存率有顯著相關關系。這與ZHANG等[30]的研究結果相似。HUANG等[9]對458例宮頸癌病人回顧性分析發現,SII是宮頸癌的獨立不良預后因素,高水平SII的宮頸癌病人無病生存率較低且腫瘤復發或轉移的概率較高。以上結果說明SII是預測乳癌無病生存率的獨立因素,可以作為評估乳癌病人預后依據之一,高SII值提示預后不良。
本研究將腫瘤臨床分期、淋巴結轉移數量、SII、ELR、HER-2、ER、Ki-67、年齡等納入Cox回歸模型進行多因素分析,其結果顯示,高SII、包塊大小>2 cm、淋巴結轉移數量≥4為影響乳癌病人預后的獨立危險因素,而在包塊大小、淋巴結轉移數量一定的情形下,高SII病人復發風險是低SII者的5.03倍;在SII、淋巴結轉移數量一定情形下,包塊大小>2 cm病人復發風險是包塊大小≤2 cm者的6.12倍;若SII、包塊大小一定,淋巴結轉移數量≥4者的復發風險是淋巴結轉移數量<4病人的4.40倍。
本研究采用ROC曲線對SII、ELR預測復發風險的診斷價值進行分析,AUC越大,其診斷價值越高。結果顯示,SII的AUC為0.71,靈敏度和特異度分別為0.71和0.66,SII的AUC>0.7,表明SII對乳癌病人預后具有較好的預測價值;而ELR的AUC為0.49,其靈敏度和特異度分別為0.63和0.48,ELR的AUC<0.7,表明ELR對乳癌病人預后的預測價值較差。
綜上所述,術前外周血SII是乳癌術后病人預后評估指標之一,術前高SII病人更容易發生復發和轉移,SII為乳癌病人預后的影響因素。而ELR不能作為預測乳癌預后的指標。本研究存在一定局限性:首先,本文研究對象均來自同一機構,存在選擇偏倚;其次,本研究是回顧性分析,尚需前瞻性臨床試驗進一步驗證。
[參考文獻]
[1] SIEGEL R L, MILLER K D, JEMAL A. Cancer statistics, 2018[J]. CA: A Cancer Journal for Clinicians, 2018,68(1):7-30.
[2] BRAY F, FERLAY J, SOERJOMATARAM I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA: A Cancer Journal for Clinicians, 2018,68(6):394-424.
[3] GUO W, CAI S H, ZHANG F, et al. Systemic immune-inflammation index (SII) is useful to predict survival outcomes in patients with surgically resected non-small cell lung cancer[J]. Thorac Cancer, 2019,10(4):761-768.
[4] SHI H T, JIANG Y Q, CAO H G, et al. Nomogram based on systemic immune-inflammation index to predict overall survi-val in gastric cancer patients[J]. Disease Markers, 2018, 2018:1-11.
[5] ZHOU Z Q, PANG S, YU X C, et al. Predictive values of postoperative and dynamic changes of inflammation indexes in survival of patients with resected colorectal cancer[J]. Current Medical Science, 2018,38(5):798-808.
[6] COFFELT S B, DE VISSER K E. Inflammation lights the way to metastasis[J]. Nature, 2014,507(7490):48-49.
[7] GRIVENNIKOV S I, GRETEN F R, KARIN M. Immunity, inflammation, and cancer[J]. Cell, 2010,140(6):883-899.
[8] JOMRICH G, GRUBER E S, WINKLER D, et al. Systemic immune-inflammation index (SII) predicts poor survival in pancreatic cancer patients undergoing resection[J]. Journal of Gastrointestinal Surgery, 2020,24(3):610-618.
[9] HUANG H P, LIU Q, ZHU L X, et al. Prognostic value of preoperative systemic immune-inflammation index in patients with cervical cancer[J]. Scientific Reports, 2019,9:3284.
[10] ETHIER J L, DESAUTELS D, TEMPLETON A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis[J]. Breast Can-cer Research, 2017,19:2.
[11] ELYASINIA F, KERAMATI M R, AHMADI F, et al.Neutrophil-lymphocyte ratio in different stages of breast cancer[J]. Acta Medica Iranica, 2017,55(4):228-232.
[12] HOUGHTON A M, RZYMKIEWICZ D M, JI H B, et al. Neutrophil elastase-mediated degradation of IRS-1 accelerates lung tumor growth[J]. Nat Med, 2010,16(2):219-223.
[13] FRIDLENDER Z G, SUN J, KIM S, et al. Polarization of tumor-associated neutrophil phenotype by TGF-β:“N1” versus “N2” TAN[J]. Cancer Cell, 2009,16(3):183-194.
[14] BODOGAI M, MORITOH K, LEE-CHANG C, et al. Immunosuppressive and prometastatic functions of myeloid-derived suppressive cells rely upon education from tumor-associated B cells[J]. Cancer Research, 2015,75(17):3456-3465.
[15] OCANA A, NIETO-JIMNEZ C, PANDIELLA A, et al. Neutrophils in cancer:prognostic role and therapeutic strategies[J]. Molecular Cancer, 2017,16:137.
[16] PLANTUREUX L, CRESCENCE L, DIGNAT-GEORGE F, et al. Effects of platelets on cancer progression[J]. Thrombosis Research, 2018,164:S40-S47.
[17] OLSSON A K, CEDERVALL J. The pro-inflammatory role of platelets in cancer[J]. Platelets, 2018,29(6):569-573.
[18] BASTIDA E, ORDINAS A, GIARDINA S L, et al. Differentiation of platelet-aggregating effects of human tumor cell lines based on inhibition studies with apyrase, hirudin, and phospholipase[J]. Cancer Res,1982,42(11):4348-4352.
[19] PINTO S, GORI L, GALLO O, et al. Increased thromboxane A2 production at primary tumor site in metastasizing squamous cell carcinoma of the larynx[J]. Prostaglandins, Leukotrienes and Essential Fatty Acids, 1993,49(1):527-530.
[20] GRIGNANI G, PACCHIARINI L, RICETTI M M, et al. Mechanisms of platelet activation by cultured human cancer cells and cells freshly isolated from tumor tissues[J]. Invasion Metastasis,1989,9(5):298-309.
[21] ZUCCHELLA M, DEZZA L, PACCHIARINI L, et al. Human tumor cells cultured “in vitro” activate platelet function by producing ADP or thrombin[J]. Haematologica,1900,74(6):541-545.
[22] DUMITRU C A, LANG S, BRANDAU S. Modulation of neutrophil granulocytes in the tumor microenvironment: Mechanisms and consequences for tumor progression[J]. Se-minars in Cancer Biology, 2013,23(3):141-148.
[23] FRANCESCONE R, HOU V, GRIVENNIKOV S I. Micro-biome, inflammation, and cancer[J]. The Cancer Journal, 2014,20(3):181-189.
[24] DIAKOS C I, CHARLES K A, MCMILLAN D C, et al. Cancer-related inflammation and treatment effectiveness[J]. Lancet Oncol, 2014,15(11):e493-e503.
[25] SAKKAL S, MILLER S, APOSTOLOPOULOS V, et al. Eosinophils in cancer:favourable or unfavourable[J]? Current Medicinal Chemistry, 2016,23(7):650-666.
[26] MOREIRA A, LEISGANG W, SCHULER G, et al. Eosinophilic count as a biomarker for prognosis of melanoma patients and its importance in the response to immunotherapy[J]. Immunotherapy, 2017,9(2):115-121.
[27] DAVIS B P, ROTHENBERG M E. Eosinophils and cancer[J]. Cancer Immunology Research, 2014,2(1):1-8.
[28] RIGONI A, COLOMBO M P, PUCILLO C. Mast cells, basophils and eosinophils: from allergy to cancer[J]. Seminars in Immunology, 2018,35:29-34.
[29] HARBAUM L, POLLHEIMER M J, KORNPRAT P, et al. Peritumoral eosinophils predict recurrence in colorectal cancer[J]. Modern Pathology, 2015,28(3):403-413.
[30] ZHANG K, HUA Y Q, WANG D, et al. Systemic immune-inflammation index predicts prognosis of patients with advanced pancreatic cancer[J]. Journal of Translational Medicine, 2019,17:30.
(本文編輯 黃建鄉)

