Regulatory effect of mild moxibustion on P2X3 receptors in spinal cord, anterior cingulate cortex and thalamic ventral posterolateral nucleus of rats with IBS visceral hyperalgesia
Zhang Zhi-ying (張智英), Zhang Fang (張方), Weng Zhi-jun (翁志軍), Wu Huan-gan (吳煥淦), Zhou Yun (周云),Han Dong (韓冬), Li Guo-na (李國娜), Liu Hui-rong (劉慧榮), Cui Yun-hua (崔云華)
1 Key Laboratory of Acupuncture and Immunological Effects, Shanghai University of Traditional Chinese Medicine, Shanghai 200030, China
2 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
Abstract
Keywords: Moxibustion Therapy; Moxa Stick Moxibustion; Irritable Bowel Syndrome; Visceral Pain; Central Nervous System Sensitization; Receptors, Purinergic P2X3; Spinal Cord; Brain
Irritable bowel syndrome (IBS) is a chronic recurrent functional bowel disease characterized by abdominal distension or abdominal pain, accompanied by altered bowel habits without organic disease[1]. Current studies believe that the pathogenesis of IBS is closely related to factors such as visceral hypersensitivity (VH), abnormal brain-gut axis function, abnormal gastrointestinal motility, and imbalance of intestinal flora[1]. Among them,VH is considered to be the key factor in IBS pathogenesis,and the abnormal brain-gut axis interaction is the main pathological basis, which results in gastrointestinal motility disorders, intestinal flora disorders, neuroendocrine disorders, and other basic pathological changes; meanwhile, VH is closely related to the severity of IBS disease[2-4]. VH refers to the overreaction of internal organs to physiological and noxious stimuli,including allodynia and hyperalgesia. Studies believe that VH formation is mainly related to the abnormality of the primary afferent nerves of visceral sensory, the increased excitability of neurons in the cornu posterius medullae spinalis, and the adaptive changes of the central nervous system sensory function[5-6]. Abnormal visceral receptors continue to transmit the pain and other nociceptive stimuli to the central nervous system, leading to increased sensitivity of the spinal cord and higher brain centers. This is the central nervous sensitization process and plays a key role in VH formation[7].
P2X purinergic receptors are ion-gated channel receptors with adenosine triphosphate (ATP) as a ligand.They are widely distributed in peripheral and central nerve cells related to the transmission of noxious stimulus signals. P2X receptors are divided into 7 subtypes (P2X1-P2X7). Among them, P2X3 and P2X2/3 receptors are responsible for transmitting the nociceptive stimulus signals to the pain center, and play important roles in the formation of VH in peripheral and central sensitization[8-11]. Studies have found that when stimulated by expansion, intestinal epithelial cells will release a large amount of ATP. ATP acts on the P2X3 and P2X2/3 receptors of the subendothelial afferent nerve endings, to induce the pain signals of visceral nociceptive stimulation into the central nervous system[9,12-13]. In the central sensitization mechanism, the presynaptic P2X receptors of primary sensory neurons in the cornu dorsale medullae spinalis can regulate the release of neurotransmitters, leading to the persistence of visceral hyperalgesia and further inducing central sensitization[14-15]. Therefore, exploring the mechanism of central sensitization is of great significance for studying the pathogenesis of IBS visceral pain and alleviating IBS visceral hyperalgesia.
Many studies have shown that acupuncture has a significant analgesic effect in the treatment of IBS visceral hyperalgesia[16-17]. Previous studies have also confirmed that electroacupuncture stimulates the endogenous analgesia system, regulates nociceptive stimuli in both the peripheral and the central nervous system, as well as relieves visceral hyperalgesia in IBS rats;P2X3 receptors play an important role in the formation of IBS visceral hyperalgesia and the transmission of pain information. Purinergic signal transduction is considered to be the molecular biological mechanism of acupuncture to exert analgesic effect[18]. Among the purinergic receptors, the P2X receptor family is closely related to the generation and conduction of chronic visceral hyperalgesia, and plays an important regulatory role in the maintenance of chronic pain[19]. Some researchers believe that P2X purinergic receptors can be used as a neurobiological target for VH treatment[20].
Our previous study revealed that P2X3 purinergic receptors were abnormally highly expressed in the intestinal myenteric nerve plexus, dorsal root ganglion and other colon peripheral neurons of IBS visceral hyperalgesia model rats, and moxibustion reduced the P2X3 receptor expression of peripheral intestinal sensory nerves, to play a role in alleviating IBS visceral hyperalgesia[21-22].
Therefore, this study intended to observe the regulatory effects of moxibustion on the P2X3 receptor expressions in the spinal cord, anterior cingulate cortex(ACC), and thalamic ventral posterolateral nucleus (VPL)in IBS visceral pain rat models, thus, to reveal the mechanism of moxibustion in improving the visceral hyperalgesia of IBS from the perspective of central sensitization, and to provide a reliable experimental basis and theoretical basis for the clinical application of moxibustion in managing IBS.
1 Materials and Methods
1.1 Experimental animal
SPF grade male Sprague-Dawley newborn rats (5-day old) were provided by the Animal Experiment Center of Shanghai University of Traditional Chinese Medicine[Animal License Number: SCXK (Shanghai) 2013-0016].Rats were reared in the animal room with a 12 h/12 h light-dark cycle, the temperature of (20±2) ℃, and the indoor humidity of 50%-70%. Every 10 newborn rats and one breeding female rat were kept in one cage until the newborn rats were 28-day old. The newborn rats were breast-fed by the female rat, and the female rat was reared regularly with free diet and water. After 3 d,normal newborn rats were used for experiments. The handling and manipulation of experimental animals during the experiments were in compliance with the guidelines of the International Association for the Study of Pain.
1.2 Main instruments and reagents
Fully automatic tissue dehydrator, paraffin embedding machine and paraffin slicer (Leica, Germany); optical microscope (Olympus, Japan); tissue homogenizer(Shanghai Fluke Fluid Machinery Manufacturing Co., Ltd.,China); pipette (Eppendorf, Germany); gel filling rack,electrophoresis machine, film transfer machine and gel imaging system (Bio-Rad, USA).
P2X3 receptor antagonist (Cat. No. M2979, Sigma,USA); hematoxylin-eosin staining kit (Cat. No. D006-1-2,Nanjing Jiancheng Biological Co., Ltd., China); anti-P2X3(Cat. No. ab10269, Abcam, UK); anti-GAPDH (Cat. No.2118S, CST, USA); goat anti-rabbit immunoglobulin (Ig) G(Cat. No. BA1003, BOSTER, USA); horseradish peroxidase labeled goat anti-rabbit IgG (H+L) (Cat. No. A0208,Shanghai Biyuntian Biotechnology Co., Ltd., China).
1.3 Model preparation and evaluation
According to the completely random number table method, thirty 8-day old newborn rats were randomly divided into a normal group (n=6) and a modeling group(n=24). Rats in the normal group were bred routinely,while in the modeling group the IBS chronic visceral hyperalgesia rat model was produced using the colorectal distention (CRD) stimulation method developed by Al-Chaer ED,et al[23]. CRD stimulation was performed twice a day at an interval of 1 h for 14 consecutive days. After the CRD stimulation, rats were routinely raised to 36-day old, and then the abdominal withdrawal reflex (AWR) score was used for model evaluation. The successful rat models were then grouped and intervened.
1.4 Groups and interventions
Except for the normal group, the modelled rats were re-divided into a model group, a mild moxibustion group,a P2X3 receptor antagonist group, and a normal saline group using the completely random number table method with 6 rats in each group. All the rats started to receive corresponding interventions at 37-day old.
1.4.1 Normal group
The rats in the normal group were only fixed without modeling or treatment, once a day for 7 consecutive days.
1.4.2 Model group
The rats in the model group were only fixed without treatment, once a day for 7 consecutive days.
1.4.3 Mild moxibustion group
After successful modeling, special moxa sticks were used for mild moxibustion about 2-3 cm above Zusanli(ST 36). Zusanli (ST 36) was positioned based on theExperimental Acupuncture Science[24]: the posterior lateral of rat knee joint, approximately 3 mm below the fibula head. Moxibustion was performed for 15 min each time, once a day for 7 consecutive days.
1.4.4 P2X3 receptor antagonist group
Rats in this group received 10 μL of P2X3 receptor antagonist (A-317491, 1 mol/L) by intrathecal injection(the needle was slowly inserted between the L5-L6spinous processes to the cauda equina nerve of rat in a prone position after anesthesia, and antagonist was then injected slowly when the rat had a tail-flick reflex)[25].Once a day for 7 consecutive days.
1.4.5 Normal saline group
Rats in the normal saline group received 10 μL of 0.9%normal saline by intrathecal injection at the same injection site as in the P2X3 receptor antagonist group,once a day for 7 consecutive days.
1.5 Sample collection
After treatment, all the rats were fasted but supplied with water for 24 h and anesthetized by intraperitoneal injection of 1% sodium pentobarbital [40 mg/(kg·bw)].The whole brain was immediately isolated after the rat was anesthetized, and immersed in pre-cold normal saline to cool the brain tissue, the ACC and VPL regions of rat brain were separated according to the specific location based on brain atlas; then the spinal cord was quickly exposed to isolate the L6-S2segment[26]; finally,rat lower abdomen was opened to fully expose the abdominal cavity and separate the colon, and 2 cm of colon tissue was collected. A part of the collected spinal cord, ACC, VPL and colon tissues were fixed in 4%paraformaldehyde fixative solution for pathological and immunohistochemistry tests; and the rest tissues were stored in -80 ℃ refrigerator for Western blot (WB)assay.
1.6 Observation indicators and detection methods
1.6.1 Evaluation of visceral hyperalgesia
AWR scores were used to evaluate the IBS visceral hyperalgesia model and the degree of the visceral hyperalgesia of rats in each group before (36-day old)and after (43-day old) the intervention.
The specific process is as follows[23]. Before the AWR scoring, rats in each group were fasted for 8-12 h and gently massaged at the lower abdomen to promote the excretion of feces in the intestine before CRD stimulation;once there was no more fecal blockage in rat intestine, a homemade balloon was inserted into the descending colon from rat anus, and then the rats were adapted in the AWR score observation box for 30 min. Afterward,the self-made balloon was connected to the desktop sphygmomanometer and syringe through the three-way valve; air was injected into the balloon through the syringe to produce CRD stimulation at different pressure levels (20 mmHg, 40 mmHg, 60 mmHg and 80 mmHg,respectively) and the AWR score was recorded (the scoring criteria are shown in Table 1). Each rat was stimulated with CRD at the same pressure level for 20 s each time, 3 times, at an interval of 1 min between two stimulations and an interval of 4 min between different pressure levels. The average of the 3 stimulation scores was used as the final score.
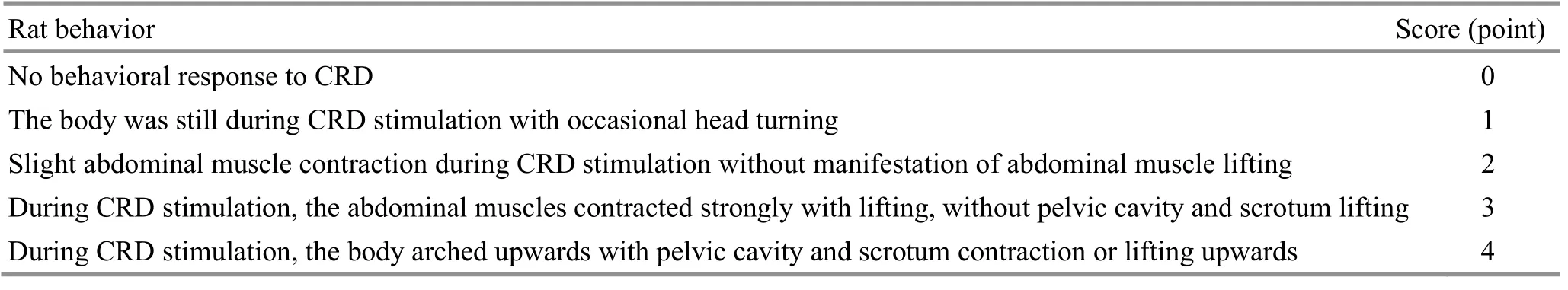
Table 1. AWR scoring standard[23]
1.6.2 Histopathological observation of rat colon
Fresh rat colon tissues were fixed with 4%paraformaldehyde solution for 24-48 h, then gently rinsed with running water for 20 min in the embedding frame. After the routine tissue dehydration and paraffin embedding, the tissue sections of 4 μm in thickness were prepared from the paraffin blocks and dried on 42 ℃slide dryer table overnight.
The tissue sections were placed on a slide dryer table at 60 ℃ for 2 h before hematoxylin-eosin (HE) staining,followed by routinely dewaxing to water; stained with hematoxylin for 2.5 min; rinsed slowly with running water for 10 min, differentiated for 3 s with 1%hydrochloric acid alcohol solution, rinsed slowly with running water for 5 min, stained with eosin for 3 min and dehydrated with gradient alcohol (70%, 80%, 90%, and 100%). Transparency was performed with xylene. A mounting reagent (xylene/neutral gum = 1.5:1) was added dropwise for mounting.
The histopathological changes in rat colon of each group were observed under an optical microscope and photographed.
1.6.3 Immunohistochemistry (IHC) detection of P2X3 protein expression in rat spinal cord, ACC and VPL tissues
IHC was stained by SP method. Images of the tissue sections were obtained under an optical microscope after staining, and Image-Pro PLUS software was used for image analysis and processing.
1.6.4 WB detection of P2X3 protein expressions in rat spinal cord, ACC and VPL tissues
Total proteins were extracted from the rat spinal cord,ACC and VPL tissues of each group using lysis buffer with protease inhibitors. BCA method was used to determine the total protein concentration. The proteins were separated with 12% polyacrylamide gel electrophoresis and blocked for 45 min (room temperature) with 5% BSA after transferred onto the membrane; incubated with the primary antibodies of anti-P2X3 (1:1 000), or anti-GAPDH (1:1 000) overnight at 4 ℃. The membrane was washed with PBST for 10 min × 4 times; then incubated with secondary antibody IgG (H+L) (1:1 000) for 2 h at room temperature. The gel imaging system was used for visualization and band image acquisition. Image J software was used to collect the band gray values of P2X3 and internal reference GAPDH.
1.7 Statistical analysis
All experimental data were analyzed and processed by SPSS 24.0 statistical software. First, normal distribution and homogeneity of variance were tested for all data.One-way analysis of variance (ANOVA) was used to compare the differences among groups when the data followed a normal distribution and homoscedasticity,and the least significant difference (LSD) method was further used for pairwise comparison. Normal distribution data with heterogeneity of variance were compared with one-way ANOVA for differences between groups, followed by pairwise comparison using Games-Howell method. The non-parametric Kruskal-Wallis H test was used to analyze data without normal distribution and the Kruskal-Wallis one-way ANOVA (k samples) was further used for pairwise comparisons. The test standard wasα=0.05, andP<0.05 indicated a statistically significant difference.
2 Results
2.1 Evaluation of IBS visceral hyperalgesia model
2.1.1 Observation of rat colonic histopathology
HE staining of rats in each group showed intact colon tissue and colon mucosal epithelial structures, neatly arranged glands, no mucosal ulcers, no plasma cells,lymphocytes and other chronic inflammatory cell infiltration, no obvious congestion and edema in the interstitium, in line with the clinical manifestation of IBS that has no histopathological changes such as local inflammation and injury (Figure 1).
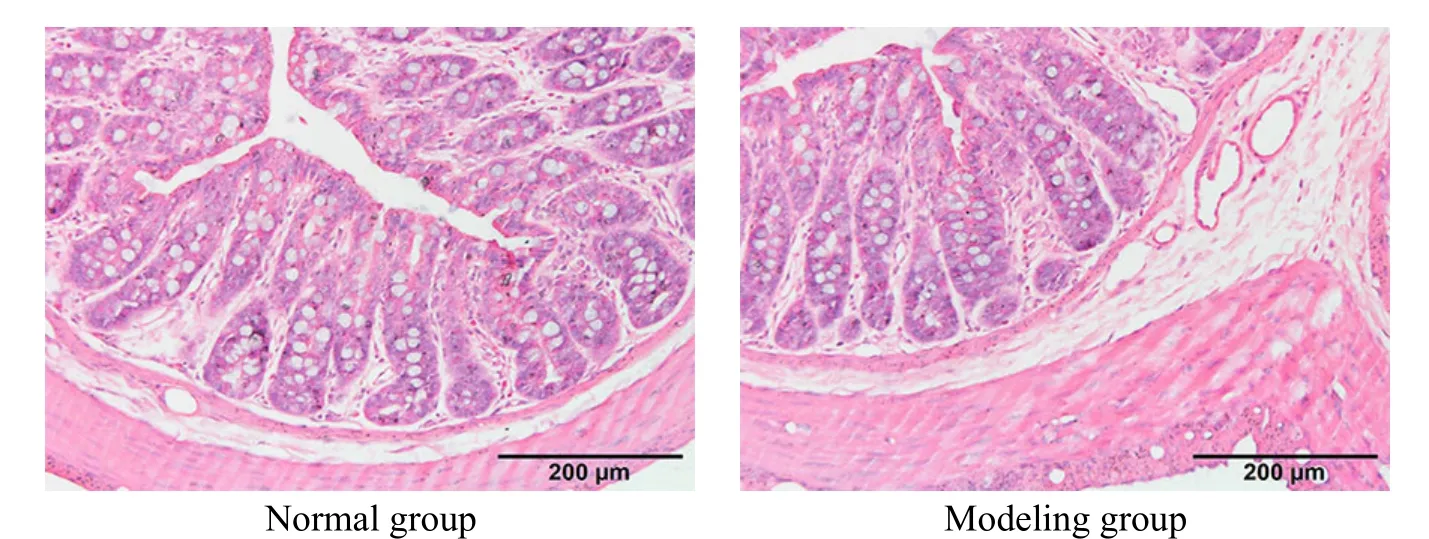
Figure 1. Observation of rat colonic histopathology in each group (HE, ×100)
2.1.2 Evaluation of rat visceral sensitivity in each group before intervention
The AWR scores at different pressure levels of rats in the modeling group before intervention were significantly higher than those of the normal group (allP<0.05), indicating that the IBS visceral hyperalgesia model rats were successfully prepared (Figure 2).
2.2 Effect of mild moxibustion on AWR scores of IBS visceral hyperalgesia model rats
Compared with the normal group, the AWR scores of the model group at different pressure levels were significantly increased (allP<0.01); compared with the model group, the AWR scores of the mild moxibustion group and the P2X3 receptor antagonist group at each pressure level were significantly reduced (allP<0.01);there were no significant differences in the AWR scores at each pressure level between the normal saline group and the model group (allP>0.05). The above behavioral results suggested that blocking P2X3 receptors or mild moxibustion intervention alleviated the degree of visceral hyperalgesia in IBS rats (Figure 3).

Figure 2. Comparison of rat AWR scores between groups before intervention

Figure 3. Comparison of rat AWR scores among groups after intervention
2.3 Effect of mild moxibustion on P2X3 protein expressions in spinal cord of rats with IBS visceral hyperalgesia
IHC results showed that the positive P2X3 receptor expression in the model group was increased significantly versus the normal group, which was dark brown and mainly in the cytoplasm of the small neuron cells in the dorsal horn of the spinal cord (P<0.01). The positive P2X3 receptor expressions in the mild moxibustion group and the P2X3 receptor antagonist group significantly reduced versus the model group(bothP<0.01), The positive P2X3 receptor expression in the normal saline group was not significantly different from that in the model group (P>0.05), (Figure 4).
WB results showed that compared with the normal group, the P2X3 receptor protein expression in rat spinal cord of the model group was increased significantly(P<0.01); compared with the model group, the P2X3 receptor protein expressions in rat spinal cord of the mild moxibustion group and the P2X3 receptor antagonist group were significantly decreased (bothP<0.01); compared with the model group, the normal saline group had no significant difference in P2X3 receptor protein expression (P>0.05), which suggested that P2X3 receptor expression in the spinal cord of IBS visceral hyperalgesia rats was significantly increased.Mild moxibustion and blocking the P2X3 receptor inhibited P2X3 receptor expression in the spinal cord of IBS visceral hyperalgesia rats (Figure 5).

Figure 4. P2X3 protein expression in rat spinal cord tissues in each group (IHC)
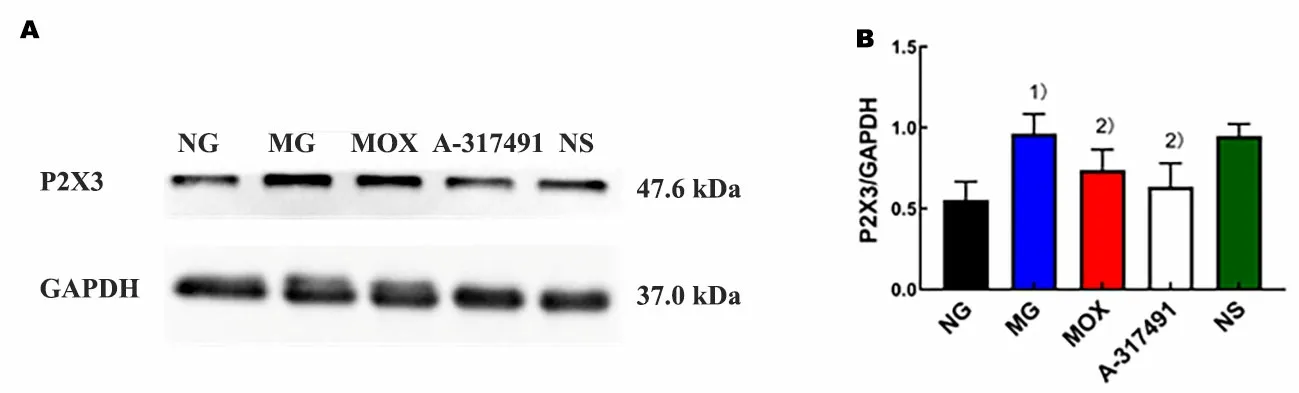
Figure 5. P2X3 protein expression in rat spinal cord tissues in each group (WB)
2.4 Effect of mild moxibustion on P2X3 protein expression in ACC tissues of rats with IBS visceral hyperalgesia
IHC results revealed that compared with the normal group, significantly increased positive P2X3 receptor expression, thicker and longer processes, darker and brownish-yellow cytoplasm of neurons were identified in the ACC of the model group, indicating a strong positive(P<0.01); compared with the model group, the positive P2X3 receptor expression was significantly weakened,the neuron cytoplasm staining was light brown, and the distribution area was small in the ACC of the mild moxibustion group and the P2X3 receptor antagonist group, indicating a weak positive (bothP<0.01); there was no significant difference between the normal saline group and the model group (P>0.05), (Figure 6).
WB results showed that compared with the normal group, P2X3 receptor protein expression in ACC of the model group increased significantly (P<0.01); compared with the model group, P2X3 receptor protein expressions in ACC of the mild moxibustion group and the P2X3 receptor antagonist group were significantly decreased (bothP<0.01); compared with the model group, rats in the normal saline group showed no significant difference in P2X3 receptor protein expression in the ACC (P>0.05), suggesting that P2X3 receptor expression in ACC of IBS visceral hyperalgesia rats was significantly increased. Mild moxibustion and blocking the P2X3 receptor both inhibited P2X3 receptor expression in the ACC of IBS visceral hyperalgesia rats(Figure 7).

Figure 7. P2X3 protein expression in rat ACC tissues in each group (WB)
2.5 Effect of mild moxibustion on P2X3 protein expression in VPL tissues of IBS visceral hyperalgesia model rats
IHC results showed that compared with the normal group, a significantly increased positive P2X3 receptor expression, darker brown stained neuron cytoplasm, and a significantly increased positive neuron number were identified in VPL of the model group, indicating a strong positive (P<0.01); compared with the model group, a weaker positive P2X3 receptor expression, and light brown stained neuron cytoplasm were identified in VPL of the mild moxibustion group and the P2X3 receptor antagonist group, indicating a weaker positive expression (bothP<0.01); the positive P2X3 receptor expression in VPL of the normal saline group was not significantly different versus the model group (P>0.05),(Figure 8).
WB results showed that compared with the normal group, the P2X3 receptor protein expression in the VPL of the model group was significantly increased (P<0.01);compared with the model group, the expressions of P2X3 receptor protein in the VPL of the mild moxibustion group and the P2X3 receptor antagonist group were significantly decreased (bothP<0.01); compared with the model group, the expression of P2X3 receptor protein in the VPL of rats in the normal saline group had no significant difference (P>0.05), suggesting that the expression of P2X3 receptor in VPL of IBS visceral hyperalgesia rats was significantly increased. Mild moxibustion and blocking P2X3 receptor inhibited P2X3 receptor expression in the VPL of IBS visceral hyperalgesia rats (Figure 9).

Figure 8. P2X3 protein expression in rat VPL tissues in each group (IHC)

Figure 9. P2X3 protein expression in rat VPL tissues in each group (WB)
3 Discussion
IBS is a common functional bowel disease, and VH is the core pathogenesis of IBS[4]. Abnormal brain-gut interaction is the main physiological basis for VH formation. Abnormal nociceptive stimuli are continuously transmitted from visceral receptors to the central nervous system, leading to the plastic changes in excitatory and inhibitory synapses, and the increased sensitivity in the spinal cord and higher brain centers[27].Moxibustion shows obvious analgesic advantages in inhibiting IBS visceral hyperalgesia[28-30]. However, the analgesic mechanism of moxibustion in relieving IBS visceral hyperalgesia has not been fully elucidated. Our previous research only explained the effect of moxibustion on peripheral sensitization[22], and the related mechanism of moxibustion for central sensitization remains unknown, so more in-depth research is needed for further exploration.
This study intended to explore the mechanism of moxibustion in analgesia from the perspective of central sensitization. The IBS visceral hyperalgesia model established by CRD stimulation was consistent with the colonic pathological characteristics of IBS patients.
The AWR score was significantly reduced after mild moxibustion at Zusanli (ST 36), which totally confirmed the effects of mild moxibustion in effectively relieving the visceral hyperalgesia in IBS rats[22,31]. Blocking the P2X3 receptor also significantly reduced AWR score, indicating that the P2X3 receptor can be used as a target for IBS visceral hyperalgesia treatment, which is consistent with our previous findings[21]. P2X3 receptors can mediate the central sensitization of chronic visceral pain, and are significantly positively associated with the central sensitization of visceral hyperalgesia[21,32]. Central sensitization is a complex process involved in multiple central conduction sites and functions. Central nociceptive stimulus formed by VH is mainly conducted through the primary afferent neurons located in the dorsal root ganglia to receive visceral sensory information and project it into the spinal cord, and then to the thalamus through the spinothalamic tract by the neurons in the superficial layer of the spinal dorsal horn.VPL receives, modulates and integrates the visceral pain information from the spinothalamic tract, and then projects it to the ACC and other visceral sensationrelated cortex through tertiary neurons. This central conduction pathway is closely related to the formation and development of VH[7,33-35].
Combining previous research on P2X3 receptors and central sensitization, we have found that P2X3 receptors activate pain-sensing neurons in the spinal cord and ACC during VH central sensitization, causing central sensitization. This has been also confirmed in our current study. After application of P2X3 receptor blockers, the P2X3 receptor expressions in the spinal cord, ACC, and VPL of the IBS visceral hyperalgesia model rats were found to be positively associated with behavioral scores,indicating that P2X3 receptors can cause the sensitization of the spinal cord, ACC, and VPL, and exacerbate VH caused by central sensitization;meanwhile, mild moxibustion alleviated IBS visceral hyperalgesia through P2X3 receptors, which was consistent with previous findings that electroacupuncture alleviated VH by down-regulating different levels of P2X3 receptors in the brain-gut axis[21].Therefore, we speculate that inhibition of P2X3 receptorrelated central sensitization should be an important mechanism for mild moxibustion to relieve IBS visceral hyperalgesia. This study revealed that P2X3 receptors in the spinal cord, ACC, and VPL played sensitizing roles in the central sensitization of IBS visceral pain at the molecular biology level; moxibustion inhibited central sensitization by targeting the P2X3 receptor; and the molecular mechanism regarding purinergic receptors in moxibustion inhibiting central sensitization was firstly discovered.
This study did not further verify the mechanism of P2X3 receptors in moxibustion inducing analgesia through interfering functions of the targeted genes or receptors. So, we will carry out more in-depth research to provide more scientific and systematic evidence for moxibustion to treat IBS visceral hyperalgesia.
Conflict of Interest
Author Wu Huan-gan is a member of the Editorial Board of Journal of Acupuncture and Tuina Science. The paper was handled by other editors and has undergone rigorous peer review process. Author Wu Huan-gan was not involved in the journal’s review or decisions related to this manuscript.
Acknowledgments
This work was supported by Shanghai Municipal Commission of Health and Family Planning (上海市衛(wèi)生和計劃生育委員會科研課題, No. 20174Y0015); National Natural Science Foundation of China (國家自然科學(xué)基金項目, No. 81904301); National Basic Research Program of China (973 Program, 國家重點基礎(chǔ)研究發(fā)展計劃項目,No. 2015CB554501); Three-year Action Plan for the Development of Shanghai Traditional Chinese Medicine [上海中醫(yī)藥事業(yè)發(fā)展三年行動計劃項目, No. ZY(2018-2020)-CCCX-2004-01]; National Chinese Medicine Leading Talent Support Program-Qi Huang Scholar (國家中醫(yī)藥領(lǐng)軍人才支持計劃-岐黃學(xué)者).
Statement of Human and Animal Rights
The treatment of animals conformed to the ethical criteria in this experiment.
Received: 14 November 2020/Accepted: 3 February 2021
——中醫(yī)藥科研創(chuàng)新成果豐碩(一)
 Journal of Acupuncture and Tuina Science2021年4期
Journal of Acupuncture and Tuina Science2021年4期
- Journal of Acupuncture and Tuina Science的其它文章
- Modern literature study of auricular point therapy for primary insomnia
- Effects of acupuncture plus MOTOmed intelligent motor training in treating children with spastic cerebral palsy
- Efficacy and effect on serum VEGF-C of mild moxibustion plus functional exercise for upper-limb lymphedema after breast cancer surgery
- Adjunctive effects of acupressure therapy on pain and quality of life in patients with knee osteoarthritis: an interventional study
- Muscle regions of meridians warm needling method plus pricking Jing-Well points for blood-letting in the treatment of shoulder-hand syndrome after stroke
- Clinical study on long-snake moxibustion plus Western medicine in treating chronic heart failure due to heart-kidney yang deficiency
