Tumor characteristics of hepatocellular carcinoma after direct-acting antiviral treatment for hepatitis C:Comparative analysis with antiviral therapy-naive patients
Magdy Fouad,Mohamed El Kassas,Elham Ahmed,Reem El Sheemy
Magdy Fouad,Department of Tropical Medicine and Gastroenterology,Minia University,Minia 61519,Egypt
Mohamed El Kassas,Department of Endemic Medicine,Faculty of Medicine,Helwan University,Cairo 11795,Egypt
Elham Ahmed,Department of Internal Medicine,Minia University,Minia 61519,Egypt
Reem El Sheemy,Department of Tropical Medicine,Minia University,Minia 61111,Egypt
Abstract BACKGROUND Insufficient and contradictory data are available about the relation between directacting antivirals(DAAs)and hepatocellular carcinoma(HCC)development in patients with hepatitis C virus(HCV).AIM To analyze differences in basic clinical,radiological,and laboratory characteristics in addition to tumor behavior upon HCC diagnosis between patients with and without a previous history of DAAs exposure.METHODS This multicenter case-control study included 497 patients with chronic HCVrelated HCC,allocated into one of two groups according to their history of antiviral treatment for their HCV.RESULTS Group I included 151 HCC patients with a history of DAAs,while 346 patients who had never been treated with DAAs were assigned to group II.A significant difference was observed between both groups regarding basic assessment scores(Child,MELD,and BCLC),which tended to have more advanced liver disease and HCC stage upon diagnosis in group I.However,serum albumin was significantly affected,and serum α-fetoprotein was significantly higher in group II(P< 0.001).In addition,group I showed significant HCC multicentricity than group II,while the incidence of portal vein thrombosis was significantly higher in group I(P< 0.001).CONCLUSION The basic clinical scores and laboratory characteristics of HCC patients are advanced in patients who are na?ve to DAAs treatment;however,HCC behavior is more aggressive in DAA-treated patients.
Key Words:Hepatocellular carcinoma;Direct-acting antiviral treatment;Hepatitis C;Tumor behavior;Occurrence
INTRODUCTION
Hepatocellular carcinoma(HCC)is the sixth most common cancer and the third most common cause of cancer-related mortality worldwide[1].In Egypt,HCC is a significant public health problem responsible for 33.63% and 13.54% of all cancers in males and females,respectively[2].On the other hand,hepatitis C virus infection(HCV)is considered a leading cause of chronic liver disease in Europe,the United States,and many other countries,including Egypt[3,4].The risk of HCC development in HCV-related liver cirrhosis is 2% to 8% per year[5].Multiple studies and metaanalyses demonstrated during the era of interferon(IFN)-based therapy that HCV eradication decreased the risk of hepatocarcinogenesis regardless of fibrosis stage[6,7].Furthermore,these studies showed that the achievement of sustained virologic response(SVR)after IFN based treatment is directly related to reduced incidence of HCC and increased survival rates[8].
In 2014,the introduction of the more effective direct-acting antivirals(DAAs)for HCV treatment was generally expected to benefit all patients,including those who were not permitted to be treated with IFN-based therapy[7].However,unexpectedly,the clinical use of DAAs has evoked a significant dilemma about the relationship between DAAs and the development of HCC.Some studies have suggested a direct relation between DAAs and the development of HCC,while others have insisted that DAAs are protective against HCC development[7].
In 2016,the first report in this context showed an unexpectedly high recurrence rate of previously treated HCC after DAAs exposure[6].This initial report was followed by another retrospective study conducted in Italy which included 344 patients with HCVrelated cirrhosis who received different DAA regimens;91% achieved SVR.The patients were followed for 24 wk.The study revealed a 29% recurrence rate for those with a history of HCC and a 3.16% incidence rate(de novo HCCs)in those without a history of prior HCC irrespective of the used DAA regimen[9].
In addition to HCC recurrence,the different biological behavior of HCC in DAAs exposed patients,and the pattern of recurrence after DAA treatment has also been reported in studies coming from various countries.For example,in 2017,Reig and his colleagues reported more aggressive HCC recurrence after DAA treatment,as defined by an advanced Barcelona Clinic Liver Cancer(BCLC)stage[6].Moreover,Renzulliet al[10]found a more aggressive HCC recurrence pattern with vascular invasion evidence after DAA therapy.
This study aimed to analyze differences in basic clinical,radiological,and laboratory characteristics and tumor behavior upon HCC diagnosis between patients with and without a previous history of DAAs exposure.
MATERIALS AND METHODS
Study design
The current study is a multicenter retrospective case-control study designed to compare the basic demographic,laboratory,and radiological criteria of HCC in patients with a history of DAAs treatment for their chronic HCV infection compared to HCC patients with no previous history of HCV antiviral treatment.Patients were recruited from December 2016 to April 2019 from Minia university hospital and Minia fever hospital,Minia,Egypt.Study patients were assigned to one of 2 groups according to previous DAAs exposure.The first group included 151 HCC patients who were previously treated with DAAs(Group I).According to a standardized treatment protocol,all patients were treated in one of the specialized viral hepatitis treatment centers affiliated to the Egyptian National Committee for Control of Viral Hepatitis.Group II included 346 HCC patients with the first presentation as HCC and no history of antiviral treatment for their HCV infection.Patients with combined HBV or HIV infections and patients with extrahepatic malignancies were excluded from the study.
Methods
All patients were recruited and diagnosed according to EASL guidelines and updated AASLD practice guidelines for managing HCC and BCLC guidelines[11-13].In addition,baseline demographic,clinical,laboratory,and radiological criteria were studied.The Child-Turcotte Pugh score(CTP),Model for End-stage Liver Disease(MELD)score,BCLC score,and FIB 4 as a non-invasive marker for fibrosis were calculated and presented.
Lines of treatment for HCV have been verified as well as the viral response.In addition,all baseline characteristics,laboratory,radiological and medical scores were compared between the two groups.
The study was performed according to the ethical guidelines of the 1975 Declaration of Helsinki after approval from the Research Ethics Committee for human subject research at the Faculty of Medicine,Minia University(Serial:165:2/2019)on Feb 25,2019.In addition,written informed consent was obtained from all participants before enrolment in the study.
Statistical analysis
Statistical analyses were performed using IBM SPSS advanced statistics,version 26(SPSS Inc.,Chicago,Illinois,USA.Numerical data were presented as mean ± SD and median(range),whereas categorical data were presented as number(percent).The Mann-Whitney U-test and theχ2-test are used when appropriate.Statistical significance is considered ifPvalue is less than or equal to 0.05.
RESULTS
This study included 497 patients with chronic HCV-related HCC,allocated into one of two groups according to their history of antiviral treatment for their HCV.Group I included 151 patients with chronic HCV and HCC who were previously treated with DAAs.Group II included 346 patients representing all patients recruited in the same period with HCV-related HCC and age and sex-matched with group I.Most of the studied patients in both groups were males:(76.2%)and(72.0%)(Pvalue 0.33),with a mean age of 60.2 years and 59.8 years in groups I and II,respectively(Pvalue 0.70)(Table 1).Regarding the received DAAs regimen in group I patients,44.4% of patientsreceived sofosbuvir/daclatasvir(SOF/DAC),40.1% received SOF/DAC/RBV,13.2% received SOF/RBV,and only 2% received SOF/RBV/PEG IFN.Figure 1 shows patients' distribution among various treatment regimens and treatment duration,in addition to treatment viral response.
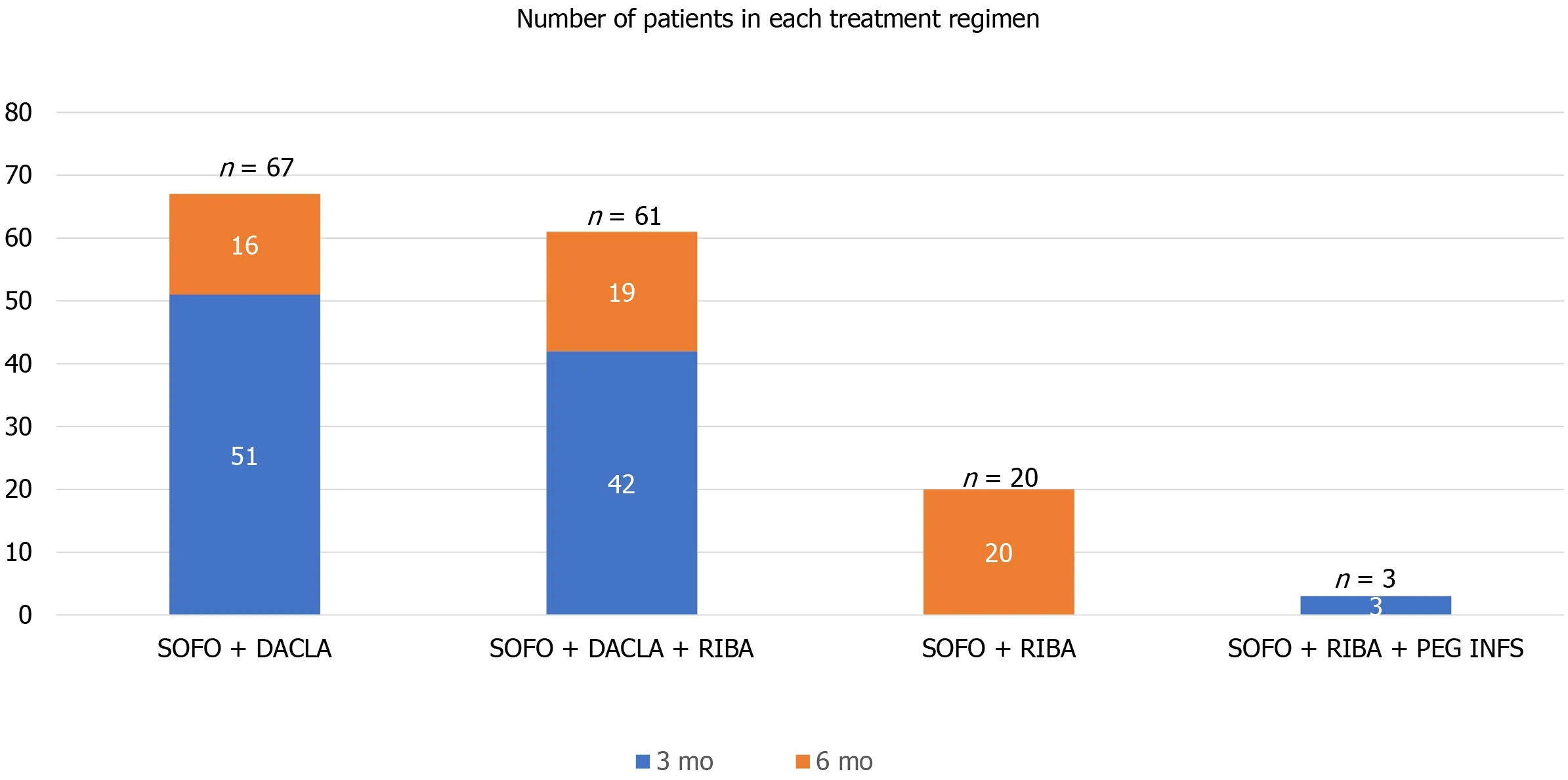
Figure 1 Patients in group I distribution among different treatment regimen.SOFO:Sofosbuvir;DACLA:Daclatasvir;RIBA:Ribavirin;PEG INFS:Pegylated interferon.
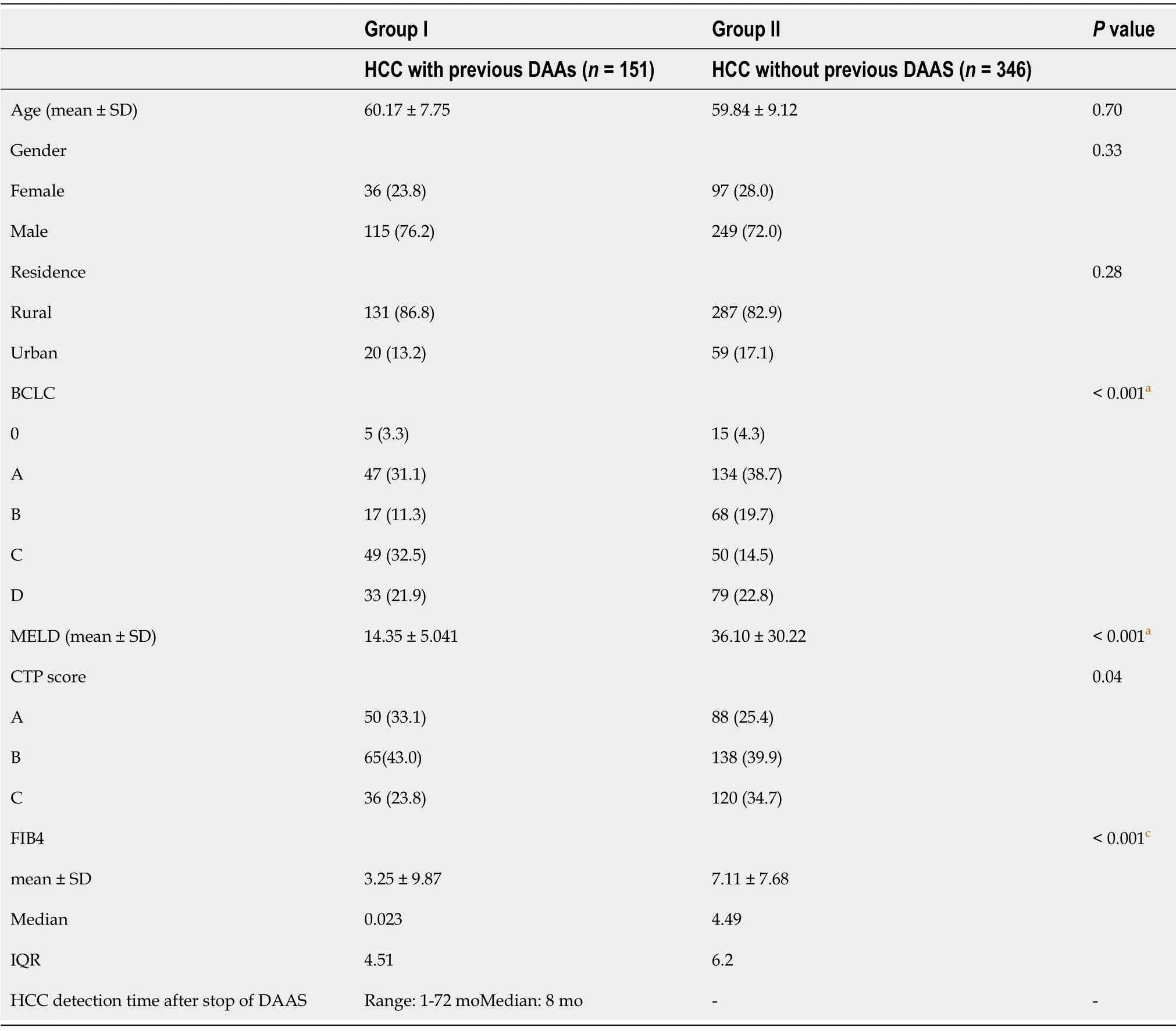
Table 1 Basic demographic data and underlying liver status in both groups
Notably,significant differences were observed between the two groups regarding the case assessment scores that reflect the severity of the underlying liver condition upon HCC discovery.A total of 34.7% of patients in group II were CTP class C,and only 23.8% of group I patients were class C.Mean MELD score in group I was 14,while the mean MELD in group II was 36(Pvalue < 0.001).Moreover,a significant difference was observed in the BCLC score(Pvalue < 0.001).A significant difference was encountered in FIB4 as a method for non-invasive fibrosis assessment with a mean FIB4 of 3.25 in group I,compared to 7.11 in group II(Pvalue < 0.001).Basic demographic data and underlying liver status in both groups are detailed in Table 1.The time between stopping DAAs and the development of HCC ranged from 1 to 72 mo with a median of 8 mo.
When comparing both groups' clinical data,no significant differences were observed except in the current smoking status,which was significantly increased in group I compared to the other group(Pvalue 0.005).On the other hand,a significant history of blood transfusion was observed in patients with no previous history of DAAs(Pvalue 0.01);cellular decompensation in the form of hepatic encephalopathy is significantly observed in patients with no previous history of DAAs(Pvalue 0.01).Detailed clinical data of the two studied groups are well presented in Table 2.
Comparing laboratory data in both groups,hemoglobin level and total leukocytic count were significantly different(Pvalues are 0.02 and 0.004,respectively).Median ALT in group I was 77 IU in comparison to 54 IU in group II(Pvalue 0.001).Mean albumin in groups I and II was(3.3 and 2.9 respectively)(Pvalue 0.004),and mean urea in groups I and II was(40 and 54 respectively)(Pvalue 0.04).Median AFP in group I was 184 in comparison to 60 in group II(Pvalue < 0.001).An illustrated comparison of all laboratory data is presented in Table 3.
Regarding the radiological characters of HCC in both groups,HCC in group I patients was more multifocal(53%)in comparison to(25%)in group II(Pvalue < 0.001).Moreover,HCCs in group I patients tended to present with a bigger tumor size at the initial presentation than group II patients.More precisely,less than 1% of group I patients were presented with tumors less than 2 cm,while more than 15% of group II patients presented with tumors less than 2 cm(Pvalue < 0.001),indicating more aggressive tumor behavior associated with the previous history of DAAs.The right lobe was the dominant victim in both groups.Early vascular invasion was significantly higher in group I compared to group II as evidenced radiologically by portal vein thrombosis(PVT),which present in 45% of group I patients and only 21% of group II patients(Pvalue < 0.001),all radiological data for HCCs in the studied patients are detailed in Table 4.
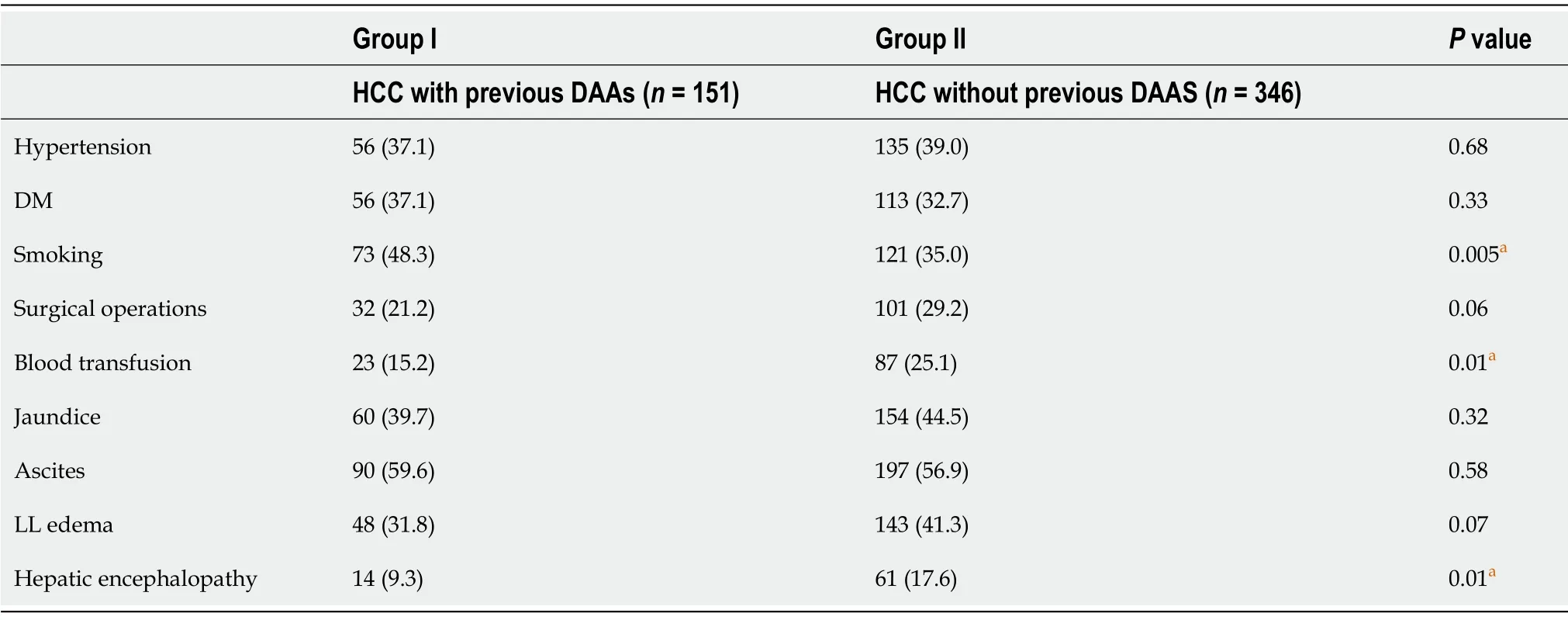
Table 2 Clinical presentation in both groups
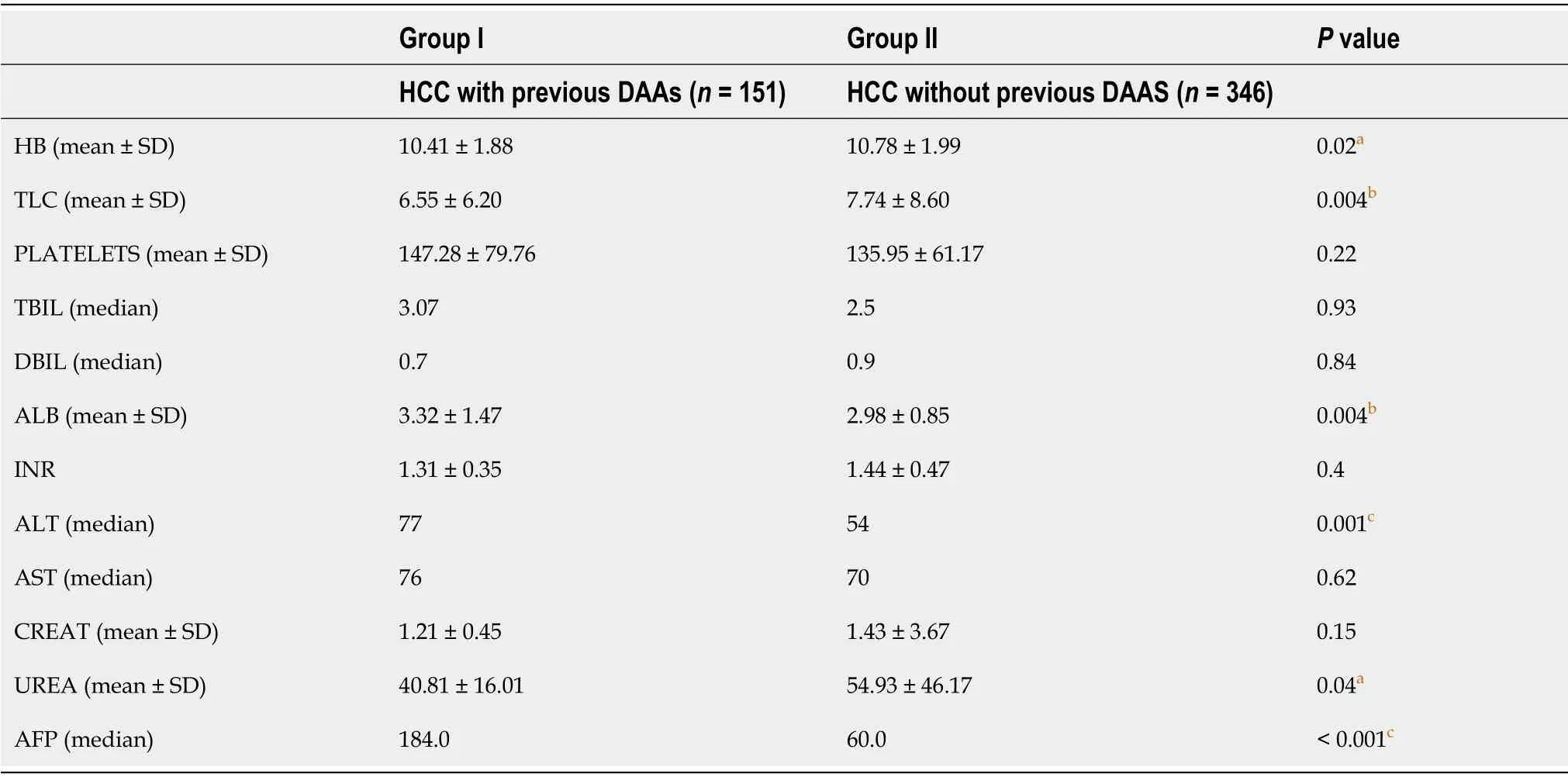
Table 3 Comparison of laboratory data in both groups
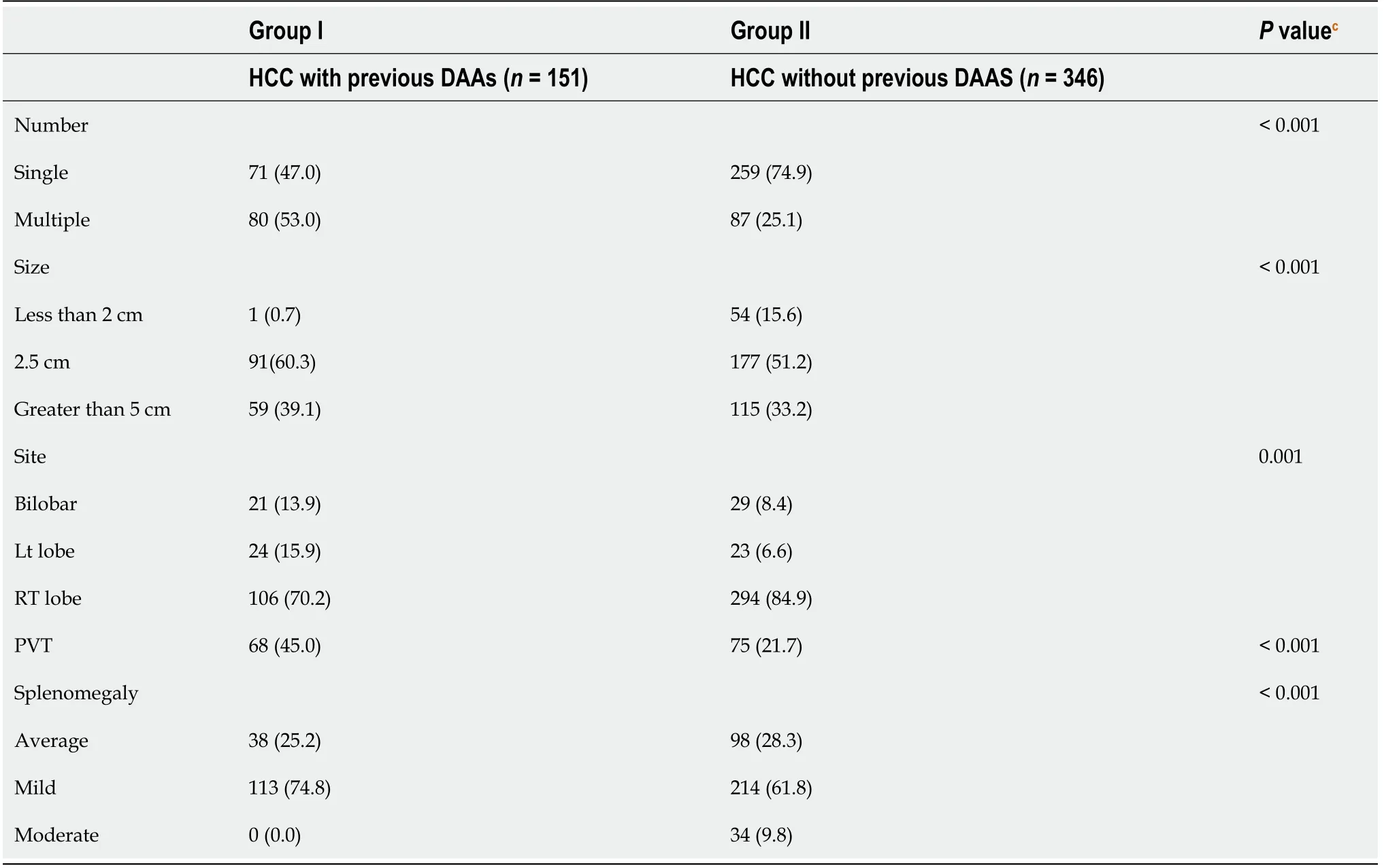
Table 4 Radiological characters of hepatocellular carcinoma in both groups
DISCUSSION
Chronic HCV infection is a significant risk factor for developing liver cirrhosis in approximately 20%-30% of patients with subsequent increased risk for HCC development in those patients with an estimated annual incidence of 3.5%[14].This risk is shown to be lower in patients with chronic HCV infection without cirrhosis and in patients who succeeded in achieving eradication,as proved by their SVR[15].Despite the notable decrease in the overall incidence of HCV infection,its prevalence in HCC patients is still high[16].Surprisingly,HCC development's risk is continuous in HCV-induced liver cirrhosis even after viral eradication and SVR achievement[16].During the interferon-based treatment era,successful viral eradication decreases the risk for HCC and improvement in the fibrosis stage[9].
The emergence of DAAs with their extended patient spectrum,improved efficacy,and safety profile increased our expectations regarding a decrease in HCC occurrence and recurrence.However,unpleasant data from new studies showed that DAAs might encourage tumor occurrence in patients with cirrhosis or recurrence in patients with previously treated HCC[9,17].The same was reported in some studies regarding HCCrecurrence after initial management upon treatment with DAAs[18].
This study stands at the current dilemma between DAAs’ benefits and drawbacks;studying the basic characteristics of HCC patients previously treated with DAAs and comparing them with HCC patients never treated with DAAs provides the central part of this controversy.
In our study,significant differences were found in the CTP,MELD,and BCLC scores in HCC patients without DAAs and those who received DAAs;these findings are contrary to what proved by Abdelazizet al[19],who found matching between patients with HCC and previous DAAs and HCC without DAAs regarding CTP score.In accordance with our results,a large study from Pakistan reported a raised neutrophil to lymphocyte ratio and younger patient age with more aggressive tumorbehavior in HCV-treated HCC patients[20].
The pattern of HCC invasion either locally inside the liver manifested by multiplicity and larger size or vascularly manifested by PVT is significantly increased with the previous history of DAAs,suggesting a possible DAAs role in such aggressive behavior.In accordance with the current study,Reiget al[6]stated the increased aggressiveness of HCC,but in recurrent cases,he omitted de novo HCC in his study.Also,Renzulliet al[10]noticed a faster rate of development of HCC after DAA therapy with an aggressive course of microvascular invasion.Similarly,Faillaciet al[21]proved that DAAs are associated with increased aggressiveness and tumor recurrence growth.Another study done by Romanoet al[21]demonstrated an aggressive behavior of tumors after DAA in the form of a higher number of nodules and extrahepatic metastases,suggesting that such patients' tumor growth is faster than usual.Many theories have been proposed to explain this unexpected event;some researchers have related the development of HCC to baseline risk factors such as advanced fibrosis grade,HBV co-infection,or age[7].Another theory proposes that DAAs cause immune surveillance mechanisms to become dysregulated due to the rapid viral clearance,and this behavior has been confirmed by several investigations[16,19].With the downregulation of type II and III IFNs,their receptors,and IFNstimulated genes,this dysregulation may result in the re-establishment of innate immunity.Due to the anti-angiogenic and anti-proliferative capabilities of IFN,which DAAs lack,a reduction in IFN activation may promote the proliferation of malignant cells.Furthermore,after HCV eradication,one of the immune system alterations observed is a decrease in the number of cytotoxic activity of natural killer cells in the liver,favoring a faster progression of HCC foci[7,22].
A significant difference was observed in AFP levels between the two groups,explained mainly by the invasive pattern and prominent vascular invasion in group I,and this is in agreement with Abdelazizet al[20].
The strengths of our study include its design and the large number of included subjects.Limitations include the exclusive existence of genotype four patients because of its prevalence in Egypt and lack of tight evaluation of other risk factors for HCC,like non-alcoholic fatty liver disease and aflatoxin effect,and the lack of further longitudinal follow up of the studied cohort.
CONCLUSION
In conclusion,despite the introduction of newer DAAs,HCV-related HCC will continue to be a significant public health concern in the coming period.Post-treatment HCV-related HCC has been discovered to be an emerging issue due to unmet needs for early HCC identification and intervention.In this study,more aggressive tumor behavior was encountered in DAAs exposed patients.Such finding needs to be investigated further in prospective studies with larger cohorts and more longitudinal followup for comparing survival and necessitates proactive screening for HCC in HCVtreated patientsviapublic or private pharmacovigilance programs.Furthermore,anti-HCV therapy in HCC patients should be postponed until a consistent risk-benefit ratio is established through further research.
ARTICLE HIGHLIGHTS
Research background
The evidence on the link between direct-acting antivirals(DAAs)and the development of hepatocellular carcinoma(HCC)in hepatitis C virus(HCV)patients is insufficient and conflicting.
Research motivation
Due to unmet needs for early HCC detection and care,post-treatment HCV-related HCC is an increasing concern.
Research objectives
To compare fundamental clinical,radiographic,and laboratory features and tumor behavior in individuals with and without a history of DAAs exposure after HCC diagnosis.
Research methods
A multicenter case-control study including 497 patients with chronic HCV-related HCC,allocated into one of two groups according to their history of antiviral treatment for their HCV.
Research results
Group I consisted of 151 HCC patients who had previously been treated with DAAs,while group II included 346 patients who had never been treated with DAAs.Regarding basic assessment scores(Child,MELD,and BCLC),there was a substantial difference between the two groups,with group I showing a tendency for more advanced liver disease and HCC stage at diagnosis.However,serum albumin levels were considerably lower in group II,and serum-fetoprotein levels were significantly greater(P= 0.001).In addition,HCC multicentricity was substantially higher in group I than in group II,and the rate of portal vein thrombosis was significantly higher in group I(P= 0.001).
Research conclusions
HCC patients who are na?ve to DAAs have more advanced clinical scores and laboratory features than those who have never been treated with DAAs;yet,HCC behavior is more aggressive in DAA-treated patients.
Research perspectives
The findings of this study warrant additional investigation in prospective trials with larger cohorts and longer follow-up for comparing survival and proactive screening for HCC in HCV-treated patients through public or private pharmacovigilance programs.
ACKNOWLEDGEMENTS
The authors acknowledge the physicians of Minia University who helped in this research.
 World Journal of Hepatology2021年11期
World Journal of Hepatology2021年11期
- World Journal of Hepatology的其它文章
- Incidence of umbilical vein catheter-associated thrombosis of the portal system:A systematic review and meta-analysis
- Six-minute walking test performance is associated with survival in cirrhotic patients
- Nonalcoholic fatty liver disease is associated with worse intestinal complications in patients hospitalized for Clostridioides difficile infection
- Circulating microRNA 9-3p and serum endocan as potential biomarkers for hepatitis C virus-related hepatocellular carcinoma
- Cystic fibrosis associated liver disease in children
- Mitochondrial hepatopathy:Respiratory chain disorders- ‘breathing in and out of the liver’
