Pyopneumothorax caused by Parvimonas micra and Prevotella oralis: a case report
Yixuan Li, Jun Yang, Junyu Wang, Bing Wei, Le Hu
Emergency Medicine Clinical Research Center, Beijing Chao-Yang Hospital, Capital Medical University, Beijing 100043,China
Parvimonasis a group of Gram-positive bacteria that are common anaerobic cocci in the oral cavity and the gastrointestinal tract and one of the pathogens of periodontitis,[1]andPrevotellais a group of Gramnegative anaerobic bacteria that are found mainly in the oral cavity and intestinal tract and are mainly involved in periodontal infections.[2]In immunocompromised patients, the abovementioned pathogens can cause infections in sites other than the oral cavity, such as bloodstream infections,[3]infective endocarditis,[4]liver abscesses,[5]meningitis,[6]and iliopsoas abscesses.[7]Because of the atypical presentation and the difficulty of culture, it is often difficult to identify these pathogenic bacteria in a timely manner in clinical practice.[8]Here,we report a case of severe pneumothorax caused by a coinfection withParvimonas micraandPrevotella oralis.
CASE
On June 19, 2022, a 59-year-old male patient presented to the Emergency Center of Beijing Chao-Yang Hospital, Capital Medical University, complaining of right chest pain and dyspnea, with a temperature of 36.9 ℃, heart rate of 145 beats per minute, breathing of 38 breaths per minute, and blood pressure of 130/73 mmHg (1 mmHg=0.133 kPa).The patient was a longterm alcoholic (equivalent to alcohol 250 g/d for more than 40 years) but was not drunk when he had chest pain.Nine days before admission, he had intermittent right chest sharp pain, accompanied by coughing and producing yellow mucous sputum; four days ago, the right chest pain worsened, accompanied by dyspnea,and the volume of the coughed-up sputum increased significantly; and one day ago, the patient’s chest pain continued to be unrelieved, dyspnea progressively worsened, and he was referred to our emergency department.Chest computed tomography (CT) revealed right pleural enveloping effusion with infection and double lung inflammation (Figure 1A).The results of laboratory tests were as follows: white blood cell (WBC)count 11.8×109/L, C-reactive protein (CRP) 209.8 mg/L, procalcitonin (PCT) 4.71 ng/mL, and partial pressure of blood oxygen (PO2) 71 mmHg (oxygen concentration:60%).Meropenem combined with vancomycin was given for anti-infection and closed drainage of the right side of the chest cavity was performed; the drainage pus was yellow-green purulent pleural fluid with a foul odor.A repeat chest CT demonstrated that the right lung had reopened, and the left lung infection was more progressive than before (Figure 1B).The pus culture and the sputum culture were negative repeatedly.The results of next-generation sequencing (NGS) of purulent pleural fluid on the 5thday after admission suggestedPeptostreptococcus(6.25%),Clostridiales FamilyXIII.Incertae Sedis(4.80%),Slackia(4.34%),Prevotella(21.49%),Parvimonas(36.33%), of whichParvimonas micra(36.33%) andPrevotella oralis(17.23%) dominated, with 12 probable normal flora(14.86%), with noMycobacteria, noMycoplasma/Chlamydia/Rickettsia, no Fungi, no DNA viruses, and no Parasites, so metronidazole was added for antiinfection.The dentistry consultation confirmed the presence of chronic periodontitis, poor oral hygiene,tartar (++), and a large amount of plaque and soft tartar.On the 7thday after admission, he developed fever with a temperature of 37.8 °C; the blood cultures was negative,and the sputum culture suggestedCandida albicans,and fluconazole antifungal treatment was added.On the 8thday post admission, the body temperature returned to normal, sputum culture suggested pan-resistantAcinetobacter baumanniiandCandida albicans, and tigecycline and sulfonamide anti-infection treatment was added.On the 11thday post admission, sputum culture suggested pan-resistantAcinetobacter baumannii, panresistantKlebsiella pneumoniae, andCandida albicans;chest X-ray showed that the left lung infection did not improve, and the WBC count further increased to 29.1×109/L.Therefore, the anti-infective regimen was modified to inclue cefoperazone sulbactam, linezolid,amikacin, and fluconazole, after which the patient’s infection index gradually decreased, and the follow-up chest CT showed improvement (Figure 1C).The patient received effective respiratory support and nutritional support during hospitalization and discharged after the improvement of his general condition.
DISCUSSION
Here, we report a case of pyopneumothorax caused by anaerobic bacteria associated with periodontitis.As the lung is an oxygen-rich organ,anaerobic bacteria-related infections rarely occur,and the pulmonary environment is unsuitable for the growth and reproduction of anaerobic bacteria such asParvimonas micraandPrevotella oralis.Thus far, there have been very few reports of pneumonia caused byParvimonas micra,[9]and this patient had a co-infection ofParvimonas micraandPrevotella oraliscausing pyopneumothorax combined with severe pneumonia,which is rare.
Parvimonas micrais a normal flora of the digestive system, genitourinary system, and skin, but is not a dominant bacterium in an aerobic environment, and it is prone to causing periodontitis in poor oral conditions.[1]There have been several cases of abdominal infection,[10]intervertebral discitis,[11]lumbar muscle infection,[7]intracranial infection,[10]and bloodstream infection[3]associated withParvimonas micra, but there are few reported cases of severe pneumonia caused by it.There has been only one case of a 35-year-old female with cerebral hemorrhage, in which the sputum culture was negative several times, and an NGS examination of the bronchoalveolar lavage fluid revealed that the pathogen causing pneumonia wasParvimonas micra.[9]The lack of specific symptoms of infection ofParvimonas micraand the relative difficulty of the microbial culture lead to a delay in the identification of the pathogenic bacteria and the adjustment of the anti-infective treatment.The application of NGS technology can be used clinically as a supplementary means of pathogenic bacteria culture,[12]particularly in the case of anaerobic bacterial infections with a low culture positivity rate.In addition, some of the lung abscesses formed byParvimonas micraare difficult to distinguish from lung cancer in radiology, and the use of NGS technology can clarify the disease diagnosis rapidly.[13]Parvimonas micrais sensitive to carbapenem,metronidazole, penicillin, vancomycin, and linezolid.[14]The previous case reports were mostly of elderly patients or patients undergoing surgery and cancer treatment,suggesting that immune insufficiency and postoperative stress may be the risk factors for aParvimonas micrainfection.However, our patient had no history of immune insufficiency or cancer, long-term alcohol abuse and poor oral hygiene as risk factors for this infection are considered.
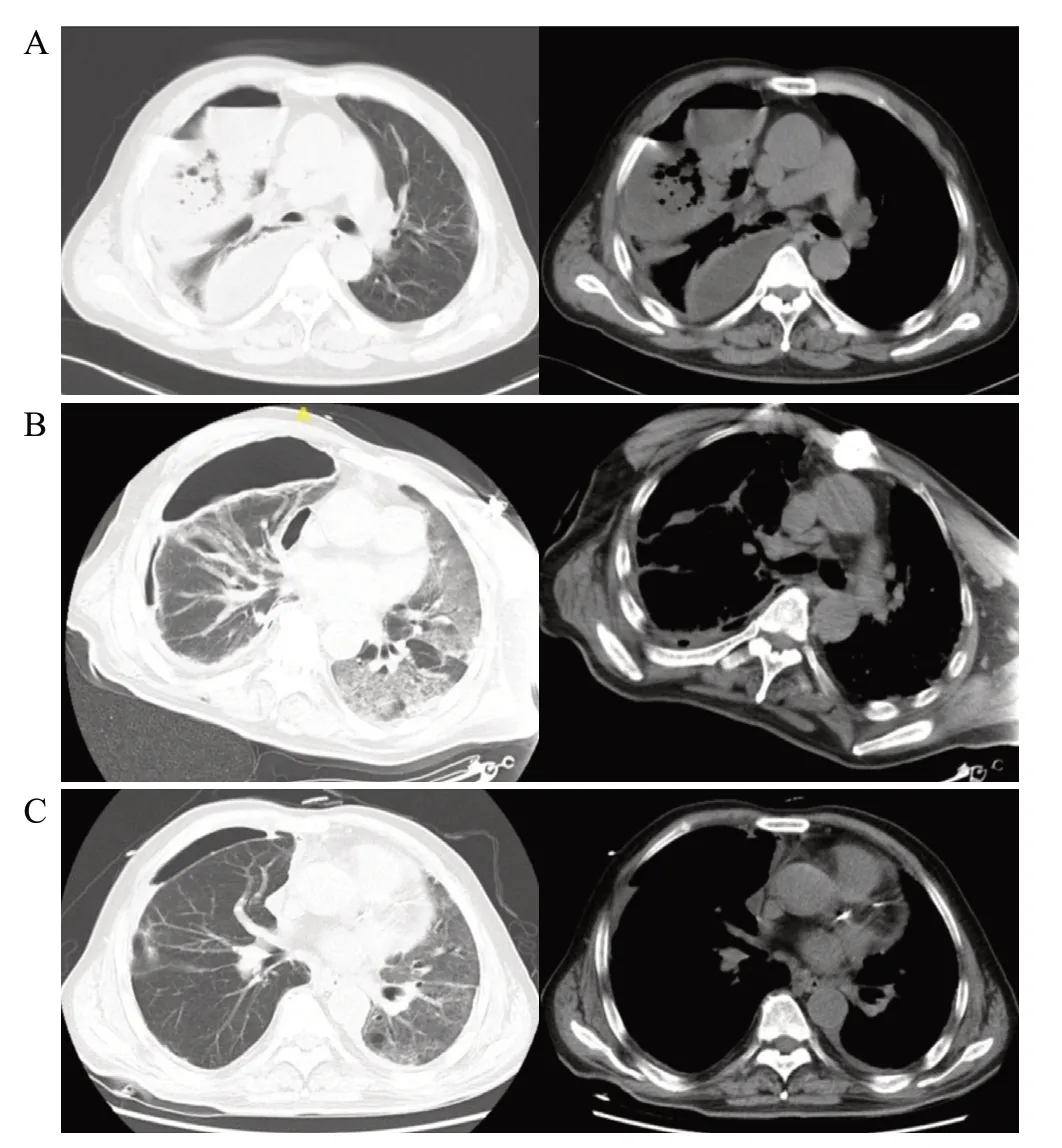
Figure 1.Comparison of chest computed tomography before and after treatment: A: before treatment, right pleural enveloping effusion with infection and double lungs inflammation; B: after chest drainage, right effusion decreased, right lung reopened, left lung progressed compared to before; C: after treatment, right effusion and pneumonia improved significantly, left lung infection improved compared to before.
Prevotella oralisis mainly found in the oral cavity and the intestinal tract, particularly in the gingival crevices.[2]In addition to oral and periodontal infections,bloodstream infections,[5,15]neck abscesses,[16]liver abscesses,[5]meningitis,[6]and breast abscesses[17]have been reported in patients with diabetes, post-surgical procedures, and immunosuppression.Prevotella oralisis an anaerobic bacterium with a low positive microbiological culture rate, and NGS can significantly increase the positive rate of this bacterium.[18]The bacterium may be resistant to penicillin and clindamycin,with a documented resistance rate of 77% to penicillin and 31%–43.5% to clindamycin, and has high sensitivity to carbapenem antibiotics.[5]
Patients with anaerobic infections are highly susceptible to secondary infections with other bacteria,with most studies reporting that less than 50% of anaerobic infections alone and more than half of anaerobic infections are mixed[19]The British Thoracic Society, in its 2010 Guidelines for the Management of Pleural Disease,[20]stated that 65% of the communityacquired pleural infections had Gram-positive aerobic microorganisms as the causative agent, and 12%–34%of patients had anaerobic infections.However, with the development of anaerobic detection methods and isolation techniques, researchers have found that anaerobes are present in up to 76% of cases, and in approximately 14% of patients, anaerobes may be the only pathogen found.
In our case, the NGS was positive for anaerobic bacteria on the 5thday after admission, and then we added anti-anaerobic bacteria treatment according to the results and the patient’s condition showed remission.However,fever developed on the 7thday, which, combined with the patient’s long-term alcohol abuse and treatment with carbapenems advanced antibiotics in the pre-course of the disease, suggested the occurrence of nosocomial infection, and the pathogen, in this case, was pandrug resistantAcinetobacter.Acinetobacteris capable of accumulating multiple antibiotic resistance genes,resulting in multi-drug resistant or pan-drug resistant strains,[21]and the mechanisms of resistance often expressed by hospital-based strains ofAcinetobacterinclude the acquisition of β-lactamases,[22]altered cell wall channels, and efflux pumps,[23]which may be the mechanism for the development ofAcinetobacterinfections in such patients.
There are some limitations of our case report.First,we did not findParvimonas micraandPrevotella oralisin the blood, sputum, or pus cultures.Second, because of the high cost, we did not perform NGS testing on the oral cavity to further clarify the homology of the pyopneumothorax pathogens, nor did we send the sputum or the bronchoalveolar lavage fluid for NGS after treatment to clarify whetherParvimonas micraandPrevotella oraliswere eradicated after treatment.
CONCLUSION
The clinical manuifestations of anaerobic pneumonia are difficult to distinguish from gernal bacterial pneumonia, prone to abscess formation, sputum or pus foul odor, but the bacterial culture is mostly negative, so identifying the pathogenic organism is the key to treating infections, and NGS allows for a rapid and accurate diagnosis when the bacterial culture results do not match the clinical presentation, and play a guiding role in the rapid response to emergency.
Funding:None.
Ethical approval:This case has received informed consent and permission from the patient.
Conflicts of interest:None.
Author contribution:All authors contributed to the design,research, writing and review of this paper.
 World journal of emergency medicine2023年6期
World journal of emergency medicine2023年6期
- World journal of emergency medicine的其它文章
- The effects of hyperbaric oxygen therapy on paroxysmal sympathetic hyperactivity after cardiopulmonary resuscitation: a case series
- The effect of prophylactic antibiotics in acute upper gastrointestinal bleeding patients in the emergency department
- Uterine artery pseudoaneurysm after subtotal hysterectomy: a case report
- Tension urinothorax as a reversible cause of cardiac arrest: a case report
- Hemorrhagic pancreatitis from fenofibrate and metformin toxicity: a case report
- A case of pulmonary mucormycosis presented with cardiac arrest
