老年HBV相關(guān)慢加急性肝衰竭預(yù)后的危險(xiǎn)因素及風(fēng)險(xiǎn)預(yù)測(cè)列線圖模型構(gòu)建
摘要:目的探討老年HBV相關(guān)慢加急性肝衰竭(HBV-ACLF)患者的臨床特點(diǎn),以及影響患者近期預(yù)后的危險(xiǎn)因素。方法選取2015年1月—2023年1月在西部戰(zhàn)區(qū)總醫(yī)院收治的417例HBV-ACLF患者進(jìn)行回顧性研究。收集患者一般情況、血常規(guī)、生化指標(biāo)、肝硬化及失代償事件情況(腹水及分級(jí),肝性腦病及分級(jí))等臨床資料。隨訪患者90天生存情況。根據(jù)年齡將患者分為老年組(≥60歲,n=106)和非老年組(lt;60歲,n=311),老年組中根據(jù)90天生存情況分為生存組(n=41)和死亡或移植組(n=65)。定量資料兩組間比較采用成組t檢驗(yàn)或Mann-Whitney U檢驗(yàn),定性資料兩組間比較采用χ2檢驗(yàn)。采用二元Logistic回歸分析確定老年HBV-ACLF患者90天死亡風(fēng)險(xiǎn)的獨(dú)立影響因素,構(gòu)建老年HBV-ACLF患者死亡風(fēng)險(xiǎn)預(yù)測(cè)列線圖模型。使用受試者工作特征曲線(ROC曲線)分別評(píng)價(jià)訓(xùn)練集與驗(yàn)證集中模型對(duì)于HBV-ACLF患者轉(zhuǎn)歸預(yù)測(cè)價(jià)值。繪制訓(xùn)練集與驗(yàn)證集中所構(gòu)建模型的校準(zhǔn)曲線與決策曲線,判斷模型擬合程度與預(yù)測(cè)收益。結(jié)果老年患者的90天病死率顯著高于非老年患者(Plt;0.05),其中老年組女性發(fā)生率、肝硬化基礎(chǔ)發(fā)生率、肝性腦病發(fā)生率及分級(jí)、腹水發(fā)生率、肝纖維化指標(biāo)水平(APRI、FIB-4)顯著高于非老年組(P值均lt;0.05);而總膽固醇、高密度脂蛋白、白蛋白、甲胎蛋白、淋巴細(xì)胞等方面顯著低于非老年組(P值均lt;0.05)。在老年HBV-ACLF患者中,生存組與死亡或移植組在總膽固醇、TBil、國(guó)際化標(biāo)準(zhǔn)比值(INR)、甲胎蛋白、血小板、肌酐、血清鈉、單核細(xì)胞數(shù)量、肝性腦病發(fā)生率及分級(jí)等方面存在顯著性差異(P值均lt;0.05)。此外,多因素Logistic回歸分析提示INR(OR=11.351,95%CI:1.942~66.362)、單核細(xì)胞(OR=23.636,95%CI:1.388~402.529)、TBil(OR=1.007,95%CI:1.001~1.013)、血小板(OR=0.968,95%CI:0.945~0.993)為HBV-ACLF老年患者90天預(yù)后的獨(dú)立影響因素(P值均lt;0.05),由此構(gòu)建的列線圖模型具有較高預(yù)測(cè)價(jià)值(ROC曲線下面積為0.915,敏感度為88.0%,特異度為86.7%),且在驗(yàn)證集中同樣具有較高效能與擬合度,決策曲線提示獲益較好,該模型與常用預(yù)測(cè)模型(MELD評(píng)分、COSSH-ACLFⅡ評(píng)分等)相比,仍具有較高預(yù)測(cè)效能。結(jié)論老年HBV-ACLF患者可能因肝臟合成、儲(chǔ)備功能、再生能力下降、免疫功能紊亂等原因而表現(xiàn)為短期高病死率。INR、單核細(xì)胞、TBil、血小板在預(yù)測(cè)老年HBV-ACLF患者死亡風(fēng)險(xiǎn)方面具有較高價(jià)值,由此構(gòu)建的列線圖模型具有較高預(yù)測(cè)效能。
關(guān)鍵詞:慢加急性肝功能衰竭;老年人;列線圖;預(yù)后
基金項(xiàng)目:四川省衛(wèi)健委科研課題(20PJ180)
Risk factors for the prognosis of elderly patients with hepatitis B virus-related acute-on-chronic liver failure and construction of a nomogram model for risk prediction
ZHANG Shihua1,2,3,BAI Chengzhi2,4,LI Chunyan2,XU Limao3,XU Huaqian2,TANG Shanhong1,2.(1.Department of Gastroenterology,The Affiliated Hospital of Southwest Medical University,Luzhou,Sichuan 646000,China;2.Department of Gastroenterology,The General Hospital of Western Theater Command,Chengdu 610083,China;3.Department of Gastroenterology,Pidu District People’s Hospital,Chengdu 611730,China;4.College of Medicine,Southwest Jiaotong University,Chengdu 610031,China)
Corresponding author:TANG Shanhong,tangshanhong@swjtu.edu.cn(ORCID:0000-0001-6652-2942)
Abstract:Objective To investigate the clinical features of elderly patients with hepatitis B virus-related acute-on-chronic liver failure(HBV-ACLF)and the risk factors affecting the short-term prognosis of patients.Methods A retrospective analysis was performed for 417 patients with HBV-ACLF who were admitted to The General Hospital of Western Theater Command from January 2015 to January 2023,and related clinical data were collected,including general status,routine blood test results,biochemical parameters,and conditions of liver cirrhosis and decompensated events(ascites,hepatic encephalopathy,and their severities).The patients were followed up to observe 90-day survival.According to the age,the patients were divided into elderly group(with 106 patients aged≥60 years)and non-elderly group(with 311 patients agedlt;60 years),and according to the 90-day survival,the elderly group were further divided into survival group with 41 patients and death/transplantation group with 65 patients.The independent-samples t test or the Mann-Whitney U test was used for comparison of quantitative data between two groups,and the chi-square test was used for comparison of qualitative data between two groups.The binary logistic regression analysis was used to determine the independent influencing factors for the risk of death within 90 days in elderly patients with HBV-ACLF,and a nomogram model was constructed for predicting the risk of death.The receiver operating characteristic(ROC)curve was used to investigate the value of the model in predicting the prognosis of HBV-ACLF patients in both the training set and the validation set.Calibration curve and decision curve were plotted for the models constructed in the training set and the validation set,and the model was assessed in terms of the degree of fitness and predicting benefits.Results The elderly patients had a significantly higher 90-day mortality rate than the non-elderly patients(Plt;0.05),and compared with the non-elderly group,the elderly group had significantly higher incidence rate in female individuals,basic incidence rate of liver cirrhosis,incidence rate and grade of hepatic encephalopathy,incidence rate of ascites,and liver fibrosis markers(aspartate aminotransferase-to-platelet ratio index and fibrosis-4)(all Plt;0.05),as well as significantly lower total cholesterol,high-density lipoprotein,albumin,alpha-fetoprotein,and lymphocytes(all Plt;0.05).As for the elderly patients with HBV-ACLF,there were significant differences between the survival group and the death/transplantation group in total cholesterol,total bilirubin,international normalized ratio(INR),alpha-fetoprotein,platelet,creatinine,serum sodium,monocytes,and the incidence rate and grade of hepatic encephalopathy(all Plt;0.05).In addition,the multivariate logistic regression analysis showed that INR(odds ratio[OR]=11.351,95%confidence interval[CI]:1.942—66.362,Plt;0.05),monocyte count(OR=23.636,95%CI:1.388—402.529,Plt;0.05),total bilirubin(OR=1.007,95%CI:1.001—1.013,Plt;0.05),and platelet count(OR=0.968,95%CI:0.945—0.993,Plt;0.05)were independent influencing factors for the 90-day prognosis of elderly patients with HBV-ACLF,and the nomogram model constructed based on these factors had a relatively high predictive value,with an area under the ROC curve of 0.915,a sensitivity of 88.0%,and a specificity of 86.7%.The nomogram model showed relatively high efficiency and degree of fitness in the verification set,and the decision curve suggested that the model had good benefits,with a higher prediction efficiency compared with the commonly used prediction models such as MELD score and COSSH-ACLFⅡscore.Conclusion Elderly HBV-ACLF patients may have a high short-term mortality rate due to the reductions in liver synthesis,reserve function,and regenerative ability and immune dysfunction.INR,monocyte count,total bilirubin,and platelet count have a relatively high value in predicting the risk of death in elderly HBV-ACLF patients,and the nomogram model constructed based on these factors has a relatively high prediction efficiency.
Key words:Acute-On-Chronic Liver Failure;Aged;Nomograms;Prognosis
Research funding:The Science Foundations of Health Commission of Sichuan Provincial(20PJ180)
慢加急性肝衰竭(ACLF)是在慢性肝病基礎(chǔ)上出現(xiàn)的急性肝功能惡化,以肝臟和/或肝外器官衰竭和短期高病死率為主要特征的復(fù)雜綜合征[1]。HBV感染是我國(guó)ACLF患者的主要病因,占所有ACLF患者的80%以上[2]。隨著人口老齡化加重,HBV相關(guān)ACLF(HBV-ACLF)的老年患者數(shù)量也逐漸增加。老年患者肝臟的體積縮小,肝細(xì)胞數(shù)量減少,肝臟代謝、免疫功能及再生功能下降,并且易合并其他慢性疾病,故導(dǎo)致老年肝臟疾病有其獨(dú)特性。劉磊等[3]發(fā)現(xiàn)老年HBV-ACLF患者病情更易進(jìn)展,病死率更高,故早期識(shí)別危險(xiǎn)因素,對(duì)于降低病死率有重要意義。
目前關(guān)于ACLF的預(yù)后評(píng)分模型較多,包括MELD系列評(píng)分、Child-Pugh評(píng)分、CLIF-C ACLF評(píng)分、AARC評(píng)分、COSSH-ACLF評(píng)分、COSSH-ACLFⅡ評(píng)分等,但以上模型均基于所有ACLF患者而建立,忽略了老年人群的特殊性,故具有一定局限性。列線圖是一種較新穎的模型構(gòu)建方法,可以將復(fù)雜的回歸方程轉(zhuǎn)變?yōu)榭梢暬膱D形,方便對(duì)患者進(jìn)行評(píng)估[4]。正是由于列線圖直觀簡(jiǎn)便的特點(diǎn),近年來它已被廣泛運(yùn)用于多種疾病的風(fēng)險(xiǎn)預(yù)測(cè)中[5-6]。因此本研究旨在分析老年HBV-ACLF患者的臨床特征,并進(jìn)一步探究老年HBV-ACLF患者的近期預(yù)后危險(xiǎn)因素,構(gòu)建風(fēng)險(xiǎn)預(yù)測(cè)列線圖模型,為老年HBV-ACLF患者的臨床診療提供參考。
1資料與方法
1.1研究對(duì)象選取2015年1月—2023年1月在西部戰(zhàn)區(qū)總醫(yī)院住院的ACLF患者。入組患者均符合《肝衰竭診治指南(2018年版)》[7]ACLF診斷標(biāo)準(zhǔn)。排除標(biāo)準(zhǔn):(1)同時(shí)感染其他病毒(戊型、甲型、丁型、丙型肝炎病毒或HIV);(2)肝功能衰竭的其他原因(自身免疫性肝病、藥物性肝炎、酒精性肝損傷等其他疾病);(3)入院時(shí)疑診或確診肝癌或其他惡性腫瘤;(4)合并心、肺、腎等其他器官系統(tǒng)的嚴(yán)重疾病;(5)年齡lt;18或gt;80歲;(6)數(shù)據(jù)不完整或失訪。所有患者根據(jù)病情需要針對(duì)性給予保肝、抗病毒、補(bǔ)充白蛋白及血漿、凝血物質(zhì)、防治并發(fā)癥,必要時(shí)行人工肝治療。
1.2研究方法通過醫(yī)院病歷系統(tǒng)查閱患者資料。收集患者一般情況(年齡、性別等);血常規(guī);生化指標(biāo),包括肝功能、腎功能、凝血功能、血脂、甲胎蛋白(AFP)等;通過癥狀、檢驗(yàn)及影像學(xué)了解是否有肝硬化及失代償事件情況(腹水及分級(jí),肝性腦病及分級(jí))。通過電話或就診記錄隨訪患者90天生存情況。根據(jù)年齡將患者分為老年組(≥60歲)和非老年組(lt;60歲),老年組中根據(jù)90天生存情況分為生存組和死亡或移植組。
1.3統(tǒng)計(jì)學(xué)方法使用SPSS 25.0進(jìn)行統(tǒng)計(jì)學(xué)分析。服從正態(tài)分布的定量資料以±s表示,兩組間比較采用成組t檢驗(yàn);不服從正態(tài)分布的定量資料以M(P25~P75)表示,兩組間比較采用Mann-Whitney U檢驗(yàn)。定性資料兩組間比較采用χ2檢驗(yàn)。Plt;0.05為差異具有統(tǒng)計(jì)學(xué)意義。運(yùn)用R 4.2.2軟件將人群按3∶1隨機(jī)分為訓(xùn)練集與驗(yàn)證集,用SPSS 25.0軟件比較兩組間各指標(biāo)差異。在訓(xùn)練集人群中,采用二元Logistic回歸分析確定老年HBV-ACLF患者90天死亡風(fēng)險(xiǎn)的獨(dú)立影響因素,運(yùn)用R 4.2.2軟件構(gòu)建老年HBV-ACLF患者死亡風(fēng)險(xiǎn)預(yù)測(cè)列線圖模型。使用受試者工作特征曲線(ROC曲線)評(píng)價(jià)訓(xùn)練集與驗(yàn)證集中模型對(duì)于HBV-ACLF患者轉(zhuǎn)歸的預(yù)測(cè)價(jià)值。繪制訓(xùn)練集與驗(yàn)證集中所構(gòu)建模型的校準(zhǔn)曲線與決策曲線,判斷模型擬合程度與預(yù)測(cè)收益。
2結(jié)果
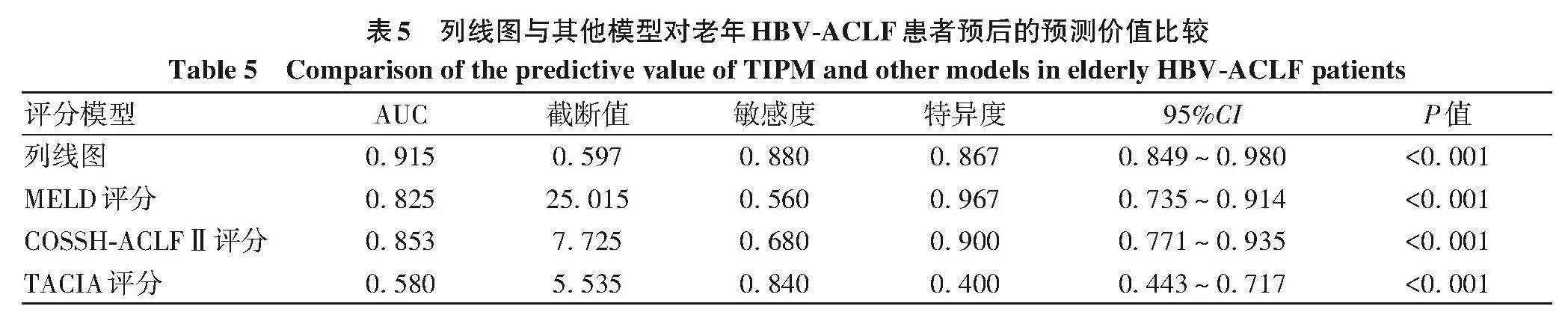
2.1老年組與非老年組HBV-ACLF臨床特征比較研究初始納入患者545例,其中40例因合并腫瘤性疾病而被排除,6例合并其他系統(tǒng)嚴(yán)重疾病被排除,72例因其他病因?qū)е翧CLF被排除,還有10例因數(shù)據(jù)不全或失訪而被排除,最終納入417例HBV-ACLF患者。按年齡60歲分組,其中老年組106例,非老年組311例。研究發(fā)現(xiàn)老年組女性發(fā)生率、肝硬化基礎(chǔ)發(fā)生率、肝性腦病發(fā)生率及等級(jí)、腹水發(fā)生率、肝纖維化指標(biāo)水平(APRI、FIB-4)COSSH-ACLFⅡ評(píng)分顯著高于非老年組(P值均lt;0.05);而血小板、總膽固醇、高密度脂蛋白(HDL-C)、白蛋白、AFP、淋巴細(xì)胞、90天生存率等方面顯著低于非老年組(P值均lt;0.05)(表1)。
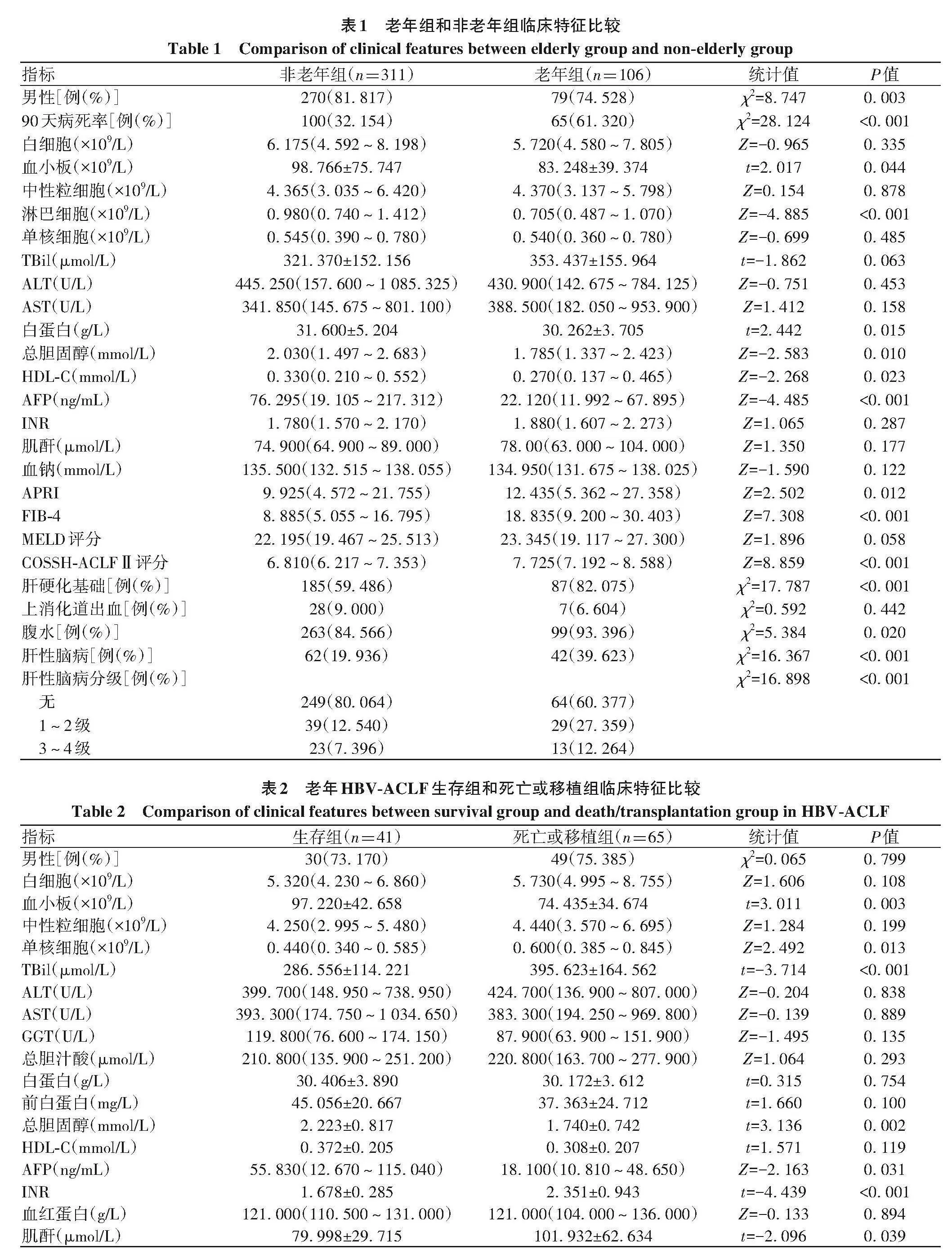
2.2老年HBV-ACLF患者生存組與死亡或移植組臨床特征比較為進(jìn)一步分析老年HBV-ACLF患者臨床特征差異,根據(jù)患者90天生存情況將老年組患者分為生存組(41例)及死亡或移植組(65例)。研究發(fā)現(xiàn)兩組間總膽固醇、TBil、INR、AFP、血小板、肌酐、血清鈉、單核細(xì)胞數(shù)量、肝性腦病發(fā)生率及分級(jí)、MELD評(píng)分、COSSH-ACLFⅡ評(píng)分有顯著性差異(P值均lt;0.05)(表2)。
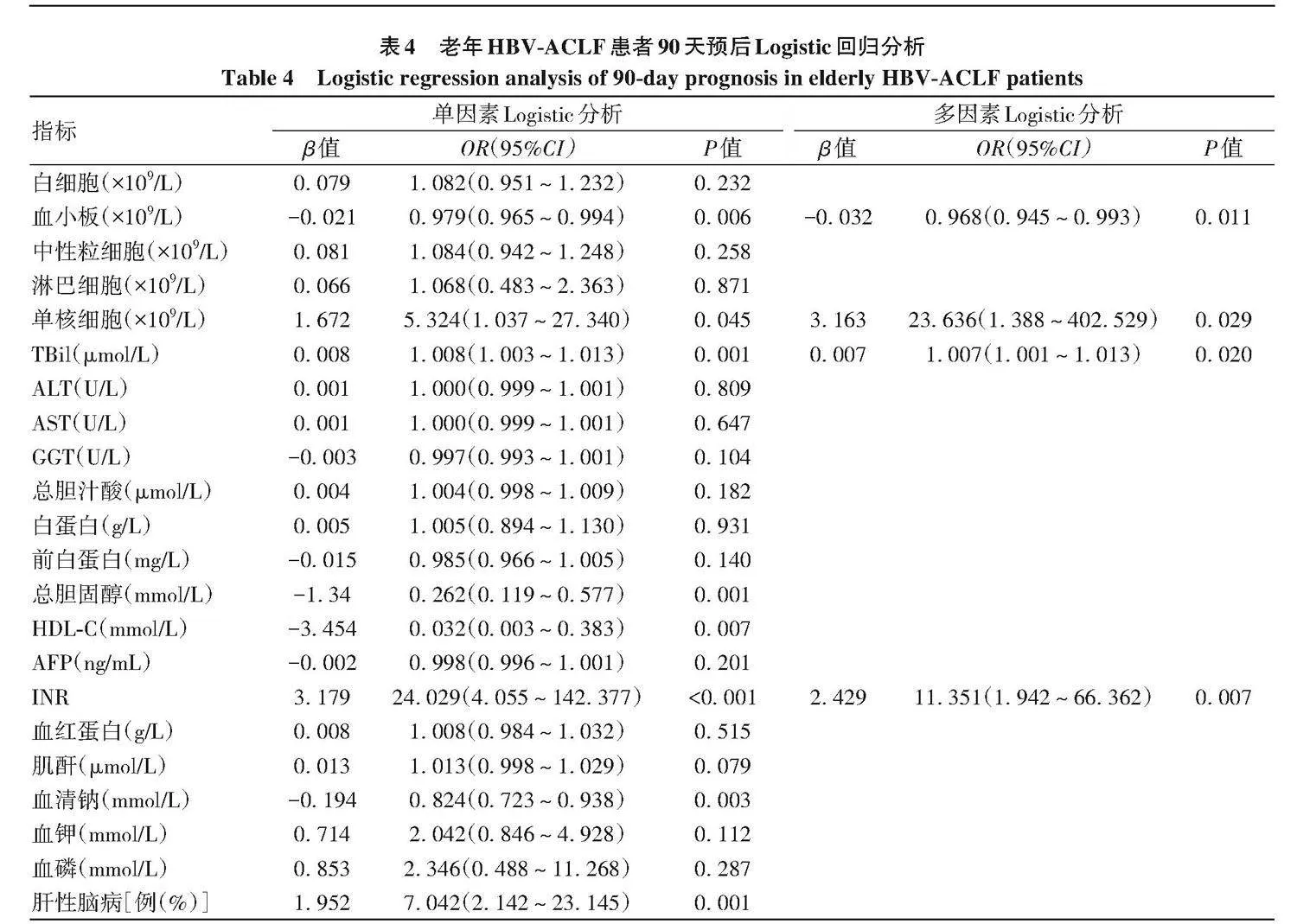
2.3 HBV-ACLF老年患者預(yù)后的相關(guān)性分析通過R語言將HBV-ACLF老年患者隨機(jī)分為驗(yàn)證集與訓(xùn)練集,兩組間各項(xiàng)指標(biāo)差異均無統(tǒng)計(jì)學(xué)意義(P值均gt;0.05)(表3)。使用Logistic回歸模型進(jìn)行單因素分析,將單因素分析有意義的指標(biāo)(總膽固醇、TBil、INR、血小板、HDL-C、血清鈉、單核細(xì)胞、肝性腦病)進(jìn)一步采用多因素Logistic回歸向前似然比法進(jìn)行分析,結(jié)果顯示INR、單核細(xì)胞、TBil、血小板為HBV-ACLF老年患者90天預(yù)后的獨(dú)立影響因素(P值均lt;0.05)(表4)。
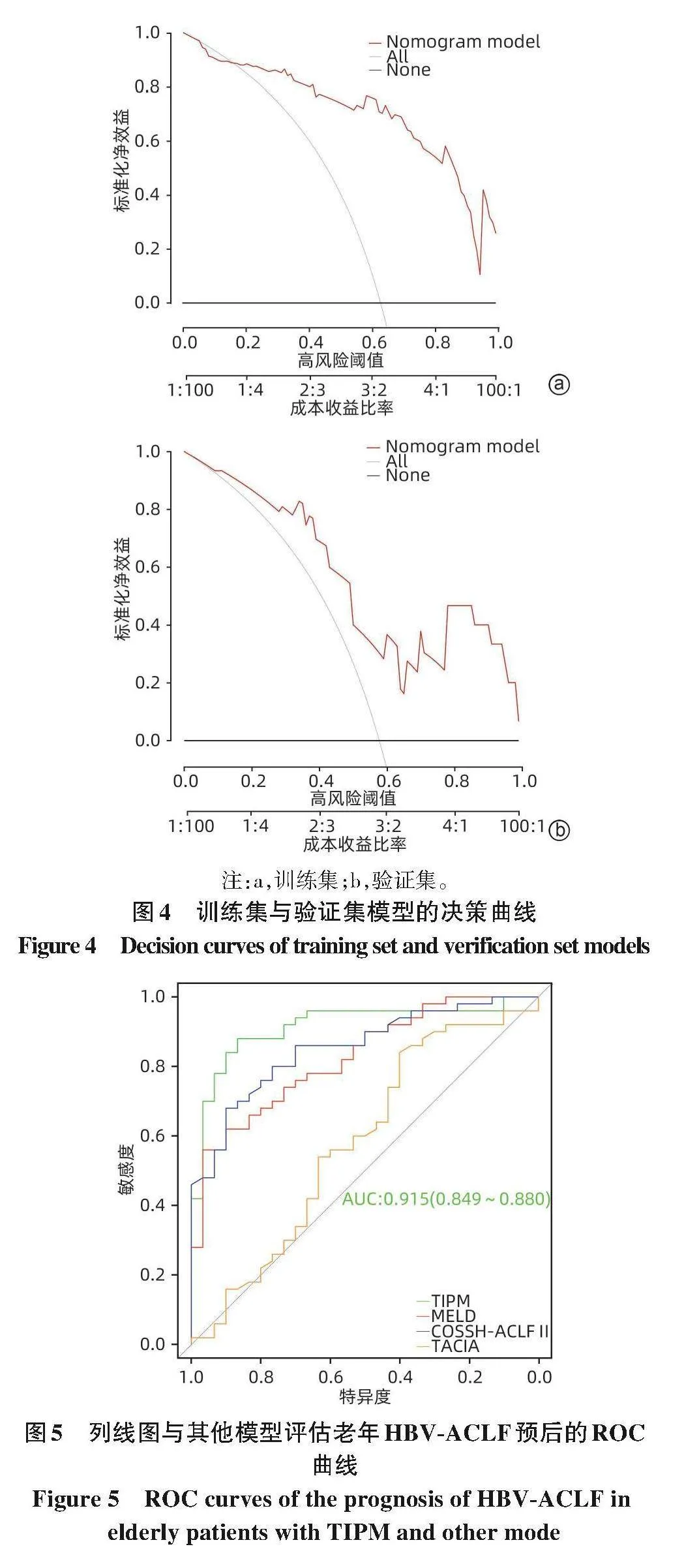
2.4預(yù)測(cè)老年HBV-ACLF預(yù)后的列線圖模型對(duì)驗(yàn)證集運(yùn)用R軟件構(gòu)建并繪制老年HBV-ACLF預(yù)后的列線圖預(yù)測(cè)模型,根據(jù)列線圖獲取各因素評(píng)分,將對(duì)應(yīng)的評(píng)分加和計(jì)算總評(píng)分,以評(píng)估老年HBV-ACLF患者90天內(nèi)死亡的風(fēng)險(xiǎn)(圖1)。
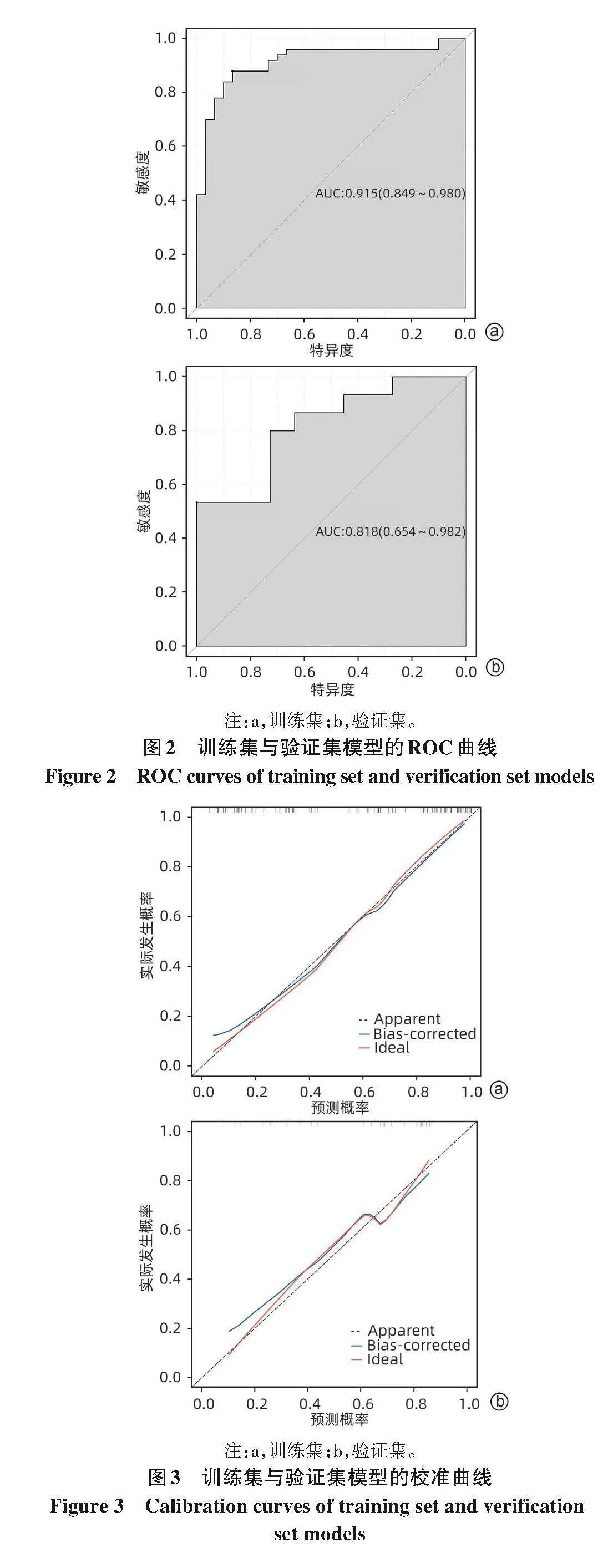
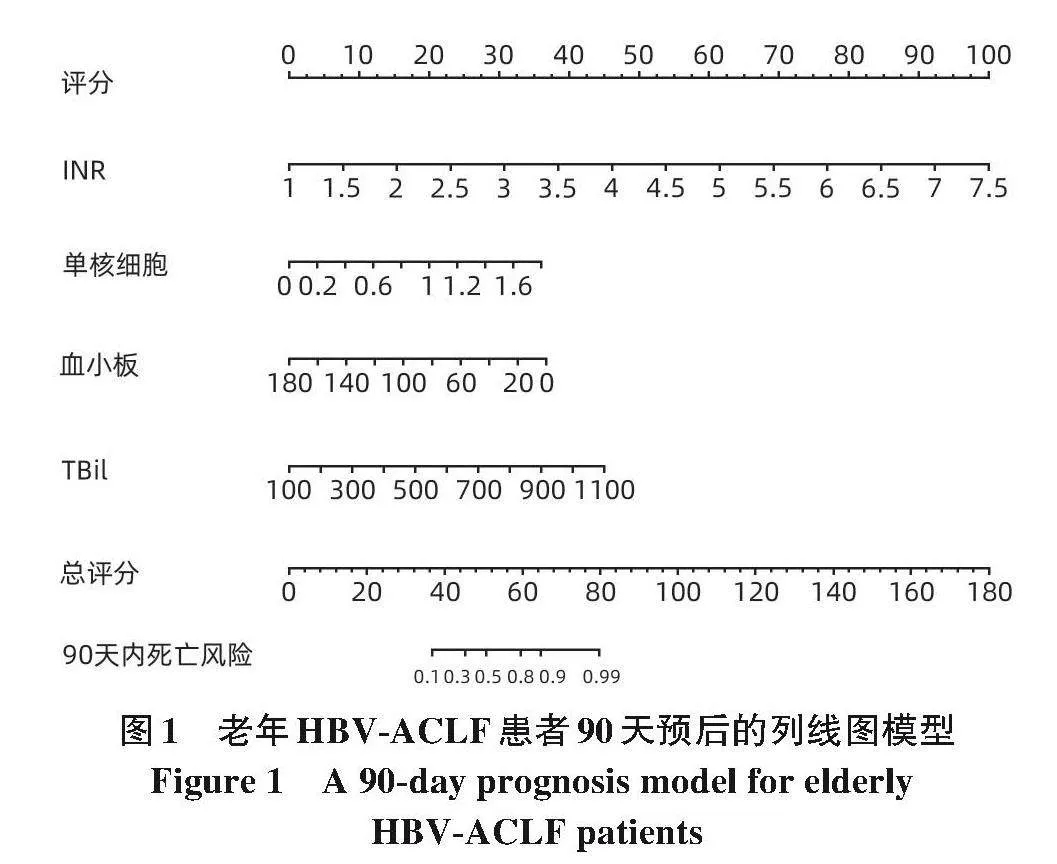
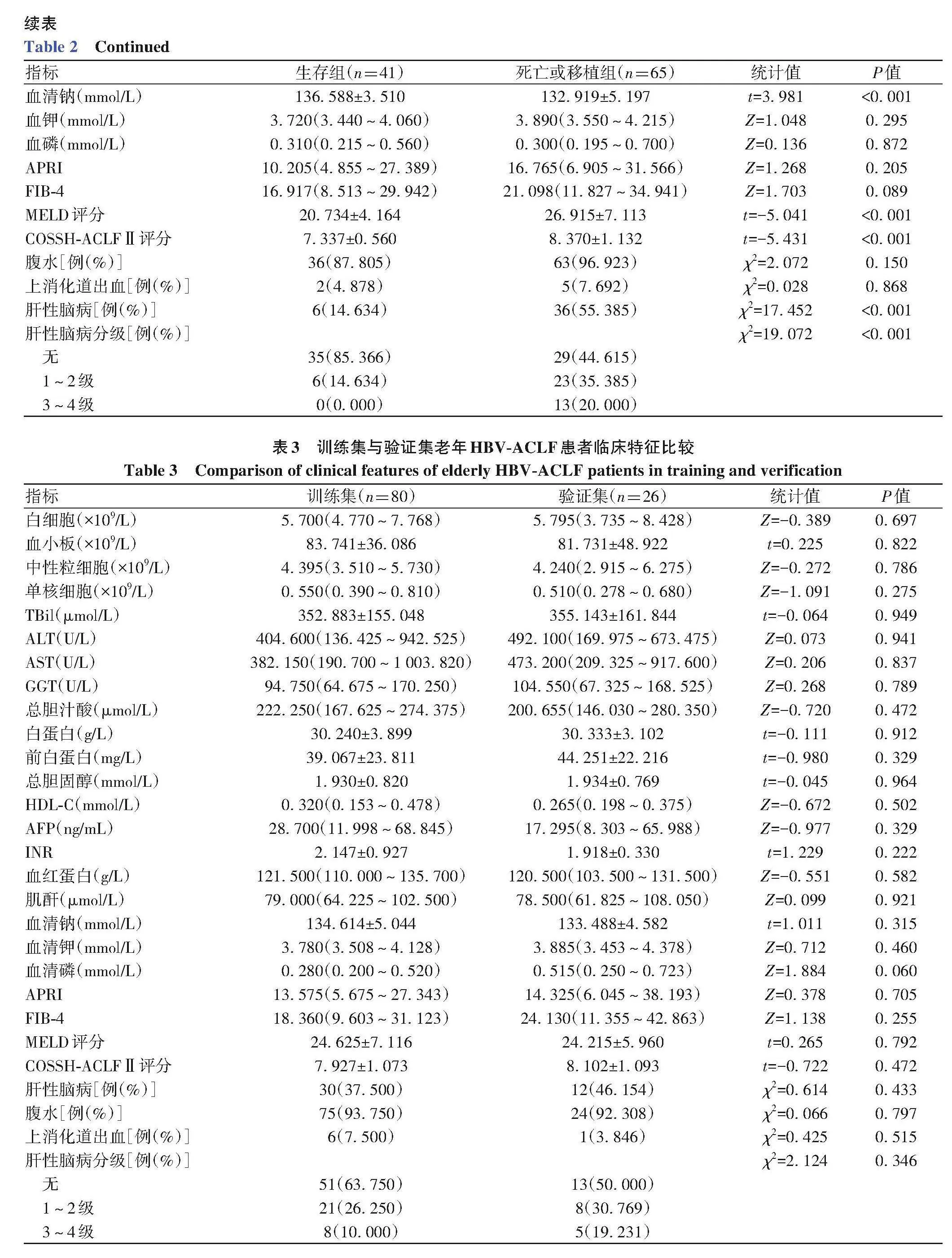
2.5老年HBV-ACLF預(yù)后列線圖模型的驗(yàn)證對(duì)訓(xùn)練集繪制ROC曲線,其ROC曲線下面積(AUC)為0.915,截?cái)嘀禐?.597,特異度為0.867,敏感度為0.880,通過R語言算出模型C-index為0.914,與AUC一致,故而該模型預(yù)測(cè)效能較好(圖2a)。對(duì)驗(yàn)證集繪制ROC曲線,其AUC為0.818,表明該模型預(yù)測(cè)準(zhǔn)確度較高(圖2b)。通過R語言分別對(duì)驗(yàn)證集與訓(xùn)練集繪制校準(zhǔn)曲線,可見兩者擬合均較好(圖3)。通過決策曲線判斷模型凈收益,可見訓(xùn)練集與驗(yàn)證集模型曲線均在兩種極端情況之上,表明通過該模型作出的決策可帶來凈收益(圖4)。
2.6列線圖風(fēng)險(xiǎn)預(yù)測(cè)模型與其他模型對(duì)老年HBV-ACLF預(yù)后預(yù)測(cè)價(jià)值比較列線圖預(yù)測(cè)老年HBV-ACLF患者的90天生存率AUC為0.915(敏感度88.0%,特異度86.7%),而MELD、COSSH-ACLFⅡ、TACIA評(píng)分的AUC分別為0.825、0.853、0.580(表5,圖5),提示列線圖模型對(duì)老年HBV-ACLF患者90天生存預(yù)測(cè)效能優(yōu)于其他模型。
3討論
HBV-ACLF病情兇險(xiǎn),疾病進(jìn)展迅速,常伴發(fā)多器官功能衰竭,具有較高的短期病死率[1]。有研究[8]提示,ACLF短期生存率僅為50%,且高齡患者死亡相對(duì)風(fēng)險(xiǎn)比是年輕患者的2.55倍。本研究結(jié)果也表明,老年HBV-ACLF患者病死率顯著高于非老年患者,其中總膽固醇、白蛋白、淋巴細(xì)胞、AFP水平較非老年組更低,而肝纖維化程度、肝性腦病發(fā)生率較非老年組更高。因此對(duì)于老年HBV-ACLF患者需考慮其自身特征,早期識(shí)別并及時(shí)干預(yù)以改善患者臨床預(yù)后。
肝臟具有較強(qiáng)的再生功能,在肝功能受損后可發(fā)生代償,恢復(fù)其功能。Kakisaka等[9]發(fā)現(xiàn)血清AFP可作為急性肝損傷或肝衰竭時(shí)肝祖細(xì)胞誘導(dǎo)和增殖的標(biāo)記。本課題組[10-11]前期發(fā)現(xiàn)AFP可作為再生標(biāo)志物,對(duì)HBV-ACLF具有較高預(yù)測(cè)價(jià)值。但本研究結(jié)果提示,老年組AFP水平顯著低于非老年組。有研究[12]表明,老年患者肝細(xì)胞衰老,端粒酶功能障礙,再生功能受損。因此,隨著患者年齡增加,肝臟免疫系統(tǒng)紊亂、再生信號(hào)通路改變、衰老細(xì)胞的表觀遺傳及肝臟中細(xì)胞因子的分泌和功能改變將導(dǎo)致肝臟再生能力下降[13]。此外,老年患者肝臟體積縮小,肝細(xì)胞數(shù)量減少,動(dòng)脈壁增厚導(dǎo)致肝臟血流灌注減少,肝竇內(nèi)皮細(xì)胞窗孔減少,星狀細(xì)胞活性增加,樹突狀細(xì)胞抗原提呈降低,T淋巴細(xì)胞活性降低,巨噬細(xì)胞吞噬及清除衰老細(xì)胞能力下降,導(dǎo)致肝臟合成、儲(chǔ)備功能、免疫功能下降,對(duì)于急性打擊易感性更高、預(yù)后更差[14]。本研究結(jié)果提示,老年生存組患者AFP水平顯著高于死亡或移植組,但分析發(fā)現(xiàn)AFP并非是老年HBV-ACLF的獨(dú)立風(fēng)險(xiǎn)預(yù)測(cè)因子,推測(cè)其可能與樣本量偏小有關(guān),有待于進(jìn)一步擴(kuò)大樣本進(jìn)行驗(yàn)證。
本研究還發(fā)現(xiàn)INR、單核細(xì)胞、TBil、血小板是老年HBV-ACLF患者90天預(yù)后的獨(dú)立影響因素,并建立了更為簡(jiǎn)化客觀的列線圖預(yù)測(cè)模型,同時(shí)通過多種方式驗(yàn)證了模型的效能與準(zhǔn)確度。INR與膽紅素在目前關(guān)于ACLF預(yù)后的預(yù)測(cè)模型中已被廣泛運(yùn)用[15-16]。老年HBV-ACLF患者多數(shù)發(fā)生在肝硬化基礎(chǔ)上,有多種機(jī)制作用均可導(dǎo)致血小板降低:肝硬化伴隨脾功能亢進(jìn)、彌散性血管內(nèi)凝血外周血小板破壞增加、血小板生成素生成減少而導(dǎo)致血小板生成減少、門靜脈高壓導(dǎo)致毒素易位和其他腸道源性物質(zhì)可導(dǎo)致免疫紊亂導(dǎo)致體內(nèi)循環(huán)免疫復(fù)合物作用于血小板,使血小板發(fā)生自身免疫性溶解[17]。Xu等[18]及本課題組[19]均發(fā)現(xiàn)血小板下降是HBV-ACLF患者預(yù)后不良的指標(biāo)。此外,一系列研究[20-21]也發(fā)現(xiàn)各種炎癥指標(biāo)(如白細(xì)胞、中性粒細(xì)胞、中性粒細(xì)胞與淋巴細(xì)胞比值、單核細(xì)胞與淋巴細(xì)胞比值、IL-6等)與HBV-ACLF患者預(yù)后有關(guān)。單核細(xì)胞是免疫早期浸潤(rùn)的細(xì)胞,與ACLF的發(fā)生息息相關(guān)[22],而老年患者對(duì)疾病進(jìn)展后的免疫應(yīng)答較弱[22],因此,筆者推測(cè)相較于其他免疫細(xì)胞,單核細(xì)胞是老年HBV-ACLF患者中更重要的危險(xiǎn)因素,但還需要進(jìn)一步的研究加以證實(shí)。
綜上所述,老年HBV-ACLF患者可能因肝臟合成、儲(chǔ)備功能、再生能力下降,免疫功能紊亂等原因而表現(xiàn)為短期高病死率。通過納入臨床上易得的數(shù)據(jù)構(gòu)建預(yù)后預(yù)測(cè)模型可以較早提示死亡風(fēng)險(xiǎn)的增減,進(jìn)而對(duì)疾病的治療方式作出及時(shí)調(diào)整。
倫理學(xué)聲明:本研究方案于2020年7月9日由西部戰(zhàn)區(qū)總醫(yī)院倫理委員會(huì)審批,批號(hào):2020ky005。
利益沖突聲明:本文不存在任何利益沖突。
作者貢獻(xiàn)聲明:張仕華、柏承志、李春燕負(fù)責(zé)研究設(shè)計(jì),數(shù)據(jù)收集與分析,稿件撰寫;張仕華、柏承志、徐理茂、徐華謙負(fù)責(zé)數(shù)據(jù)分析,稿件修改;湯善宏負(fù)責(zé)研究設(shè)計(jì)與指導(dǎo),并最終定稿。
參考文獻(xiàn):
[1]LI X,ZHANG L,PU CM,et al.Liver transplantation in acute-on-chronic liver failure:Timing of transplantation and selection of pa?tient population[J].Front Med(Lausanne),2022,9:1030336.DOI:10.3389/fmed.2022.1030336.
[2]Hepatology Branch of Chinese Medical Association,Infectious Dis?eases Branch of Chinese Medical Association.Guidelines for the prevention and treatment of chronic hepatitis B(version 2022)[J].Chin J Infect Dis,2023,41(1):3-28.DOI:10.3760/cma.j.cn311365-20230220-00050.
中華醫(yī)學(xué)會(huì)肝病學(xué)分會(huì),中華醫(yī)學(xué)會(huì)感染病學(xué)分會(huì).慢性乙型肝炎防治指南(2022年版)[J].中華傳染病雜志,2023,41(1):3-28.DOI:10.3760/cma.j.cn311365-20230220-00050.
[3]LIU L,HAN T,CAI JJ,et al.Clinical characteristics and progression risk factors for hepatitis B-related acute-on-chronic liver failure in el?derly patients[J].Chin J Geriatr,2022,41(1):51-56.DOI:10.3760/cma.j.issn.0254-9026.2022.01.011.
劉磊,韓濤,蔡均均,等.老年乙肝相關(guān)慢加急性肝衰竭患者臨床特點(diǎn)及進(jìn)展危險(xiǎn)因素分析[J].中華老年醫(yī)學(xué)雜志,2022,41(1):51-56.DOI:10.3760/cma.j.issn.0254-9026.2022.01.011.
[4]WANG X,ZHAO M,ZHANG C,et al.Establishment and clinical ap?plication of the nomogram related to risk or prognosis of hepatocellu?lar carcinoma:A review[J].J Hepatocell Carcinoma,2023,10:1389-1398.DOI:10.2147/jhc.s417123.
[5]ZHANG LJ,TANG L,CHEN SY,et al.A nomogram for predicting the 4-year risk of chronic kidney disease among Chinese elderly adults[J].Int Urol Nephrol,2023,55(6):1609-1617.DOI:10.1007/s11255-023-03470-y.
[6]CAI ZM,LIN HM,LI ZX,et al.A prediction nomogram for postopera?tive gastroparesis syndrome in right colon cancer:A retrospective study[J].Langenbecks Arch Surg,2023,408(1):148.DOI:10.1007/s00423-023-02885-6.
[7]Liver Failure and Artificial Liver Group,Chinese Society of Infectious Diseases,Chinese Medical Association;Severe Liver Disease and Artificial Liver Group,Chinese Society of Hepatology,Chinese Medi?cal Association.Guideline for diagnosis and treatment of liver failure(2018)[J].J Clin Hepatol,2019,35(1):38-44.DOI:10.3969/j.issn.1001-5256.2019.01.007.
中華醫(yī)學(xué)會(huì)感染病學(xué)分會(huì)肝衰竭與人工肝學(xué)組,中華醫(yī)學(xué)會(huì)肝病學(xué)分會(huì)重型肝病與人工肝學(xué)組.肝衰竭診治指南(2018年版)[J].臨床肝膽病雜志,2019,35(1):38-44.DOI:10.3969/j.issn.1001-5256.2019.01.007.
[8]ZHAO RH,SHI Y,ZHAO H,et al.Acute-on-chronic liver failure in chronic hepatitis B:An update[J].Expert Rev Gastroenterol Hepa?tol,2018,12(4):341-350.DOI:10.1080/17474124.2018.1426459.
[9]KAKISAKA K,KATAOKA K,ONODERA M,et al.Alpha-fetoprotein:A biomarker for the recruitment of progenitor cells in the liver in pa?tients with acute liver injury or failure[J].Hepatol Res,2015,45(10):E12-E20.DOI:10.1111/hepr.12448.
[10]WANG XP,SHEN CF,YANG JJ,et al.Alpha-fetoprotein as a predic?tive marker for patients with hepatitis B-related acute-on-chronic liver failure[J].Can J Gastroenterol Hepatol,2018,2018:1232785.DOI:10.1155/2018/1232785.
[11]QIN S,TANG SH,WANG XH,et al.Value of serum alpha-fetoprotein for the prognostic evaluation of hepatitis B virus-related acute-on-chronic liver failure treated with artificial liver[J].Chin J Hepatol,2020,28(1):69-72.DOI:10.3760/cma.j.issn.1007-3418.2020.01.016.
秦森,湯善宏,王顯紅,等.血清甲胎蛋白在人工肝治療乙型肝炎相關(guān)慢加急性肝衰竭預(yù)后評(píng)估中的價(jià)值[J].中華肝臟病雜志,2020,28(1):69-72.DOI:10.3760/cma.j.issn.1007-3418.2020.01.016.
[12]HOARE M,DAS T,ALEXANDER G.Ageing,telomeres,senescence,and liver injury[J].J Hepatol,2010,53(5):950-961.DOI:10.1016/j.jhep.2010.06.009.
[13]TANG CL,CHEN H,JIANG L,et al.Liver regeneration:Changes in oxidative stress,immune system,cytokines,and epigenetic modifi?cations associated with aging[J].Oxid Med Cell Longev,2022,2022:9018811.DOI:10.1155/2022/9018811.
[14]ALLAIRE M,GILGENKRANTZ H.The aged liver:Beyond cellular se?nescence[J].Clin Res Hepatol Gastroenterol,2020,44(1):6-11.DOI:10.1016/j.clinre.2019.07.011.
[15]KAMATH PS,WIESNER RH,MALINCHOC M,et al.A model to pre?dict survival in patients with end-stage liver disease[J].Hepatol?ogy,2001,33(2):464-470.DOI:10.1053/jhep.2001.22172.
[16]LI JQ,LIANG X,YOU SL,et al.Development and validation of a new prognostic score for hepatitis B virus-related acute-on-chronic liver failure[J].J Hepatol,2021,75(5):1104-1115.DOI:10.1016/j.jhep.2021.05.026.
[17]MITCHELL O,F(xiàn)ELDMAN DM,DIAKOW M,et al.The pathophysiol?ogy of thrombocytopenia in chronic liver disease[J].Hepat Med,2016,8:39-50.DOI:10.2147/HMER.S74612.
[18]XU XW,HOU ZH,XU YY,et al.The dynamic of platelet count as a novel and valuable predictor for 90-day survival of hepatitis B virus-related acute-on-chronic liver failure patients[J].Clin Res Hepatol Gastroenterol,2021,45(2):101482.DOI:10.1016/j.clinre.2020.06.008.
[19]TU Y,LI X,CHEN MJ,et al.Value of platelet count and related scor?ing models in predicting the prognosis of hepatitis B virus-relatedacute-on-chronic liver failure[J].J Clin Hepatol,2023,39(6):1308-1312.DOI:10.3969/j.issn.1001-5256.2023.06.009.
涂穎,李雪,陳美娟,等.血小板計(jì)數(shù)及相關(guān)評(píng)分模型對(duì)HBV相關(guān)慢加急性肝衰竭預(yù)后的預(yù)測(cè)價(jià)值[J].臨床肝膽病雜志,2023,39(6):1308-1312.DOI:10.3969/j.issn.1001-5256.2023.06.009.
[20]ZACCHERINI G,WEISS E,MOREAU R.Acute-on-chronic liver fail?ure:Definitions,pathophysiology and principles of treatment[J].JHEP Rep,2021,3(1):100176.DOI:10.1016/j.jhepr.2020.100176.
[21]JALAN R,SALIBA F,PAVESI M,et al.Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure[J].J Hepatol,2014,61(5):1038-1047.DOI:10.1016/j.jhep.2014.06.012.
[22]TRIANTAFYLLOU E,WOOLLARD KJ,MCPHAIL MJW,et al.The role of monocytes and macrophages in acute and acute-on-chronic liver failure[J].Front Immunol,2018,9:2948.DOI:10.3389/fimmu.2018.02948.
收稿日期:2024-01-19;錄用日期:2024-02-18
本文編輯:王瑩
引證本文:ZHANG SH BAI CZ, LI CY, et al. Risk factors for the prognosis of elderly patients with hepatitis B virus-related acute-on-chronic liver failure and construction of a nomogram model for risk prediction[J]. J Clin Hepatol, 2024, 40(10): 1976-1984.
張仕華, 柏承志, 李春燕, 等. 老年HBV相關(guān)慢加急性肝衰竭預(yù)后 的危險(xiǎn)因素及風(fēng)險(xiǎn)預(yù)測(cè)列線圖模型構(gòu)建[J]. 臨床肝膽病雜志, 2024, 40(10): 1976-1984.