重癥肺炎支原體肺炎患兒CD14+單核細胞人類白細胞抗原-DR表達的觀察
孫海英,邵曉麗,劉淑梅,郭 平,周國忠,陳 溢
(1.浙江省紹興縣婦幼保健所兒童保健科,浙江紹興 312030;2.浙江省紹興市人民醫院,浙江大學紹興醫院兒科,浙江紹興 312000;3.浙江省紹興市人民醫院,浙江大學紹興醫院檢驗科,浙江紹興 312000)
·論 著·
重癥肺炎支原體肺炎患兒CD14+單核細胞人類白細胞抗原-DR表達的觀察
孫海英1,邵曉麗2*,劉淑梅2,郭 平2,周國忠3,陳 溢2
(1.浙江省紹興縣婦幼保健所兒童保健科,浙江紹興 312030;2.浙江省紹興市人民醫院,浙江大學紹興醫院兒科,浙江紹興 312000;3.浙江省紹興市人民醫院,浙江大學紹興醫院檢驗科,浙江紹興 312000)
目的通過研究重癥肺炎支原體肺炎患兒靜脈血CD14+單核細胞人類白細胞抗原-DR(human leukocyte antigen DR,HLA-DR)表達百分率的變化,評價患兒的免疫狀態及與疾病的嚴重程度和預后的關系。方法選擇重癥肺炎支原體肺炎患兒共65例,以臨床肺部感染評分(clinical pulmonary infection score,CPIS)≥6分為CPIS高分組共21例,CPIS<6分為CPIS低分組共44例;正常對照組30例。重癥MPP患兒入院后第1天及出院當日抽取靜脈血,應用流式細胞儀測定CD14+單核細胞HLA-DR表達百分率,并記錄入院當天的CPIS。結果重癥肺炎支原體肺炎患兒CD14+單核細胞HLA-DR表達CPIS高分組和CPIS低分組均明顯低于正常對照組,差異有統計學意義(P<0.01);且CPIS高分組低于CPIS低分組,差異有統計學意義(P<0.01);2組治療后恢復期CD14+單核細胞HLA-DR表達均明顯升高(P<0.01)。結論重癥肺炎支原體肺炎患兒CD14+單核細胞HLA-DR表達持續低下提示患兒處于免疫抑制狀態。檢測CD14+單核細胞HLA-DR表達可用于判斷肺炎支原體肺炎患兒病情的嚴重程度和評估預后。
肺炎,支原體;抗原,CD14;兒童
肺炎支原體肺炎(mycoplasma pneumoniae pneumonia,MPP)是由肺炎支原體(mycoplasma pneumoniae,MP)感染導致的肺炎,已成為學齡期兒童社區獲得性肺炎的常見原因。目前重癥患兒增多,導致多臟器功能損害,引起國內外學者的重視。近年來的研究證實,免疫功能紊亂在MPP的發生發展中起重要作用[1]。CD14+單核細胞人類白細胞抗原(human leukocyte antigen,HLA)表達百分率是用于免疫功能抑制的指標之一[2]。本研究通過觀察MPP患兒CD14+單核細胞HLA-DR表達百分率及臨床肺部感染評分(clinical pulmonary infection score,CPIS),評價CD14+單核細胞HLA-DR表達百分率與疾病嚴重程度及預后的關系。
1 資料與方法
1.1 研究對象:2008年1月—2011年10月我院收治的MPP患兒共65例,男性42例,女性23例,年齡3~8歲,平均(5.8±1.1)歲。根據《諸福棠實用兒科學》第7版 MPP診斷標準[3],病程早期采用PCR法檢測患兒咽拭子標本中MP-DNA陽性,且發病1周后血清MP-IgM陽性,急性期抗體滴度≥1∶80,或恢復期較急性期抗體滴度升高4倍及以上為陽性;臨床符合MPP,無其他病原感染的臨床及實驗室證據。因目前重癥MPP尚無統一的診斷標準,本文參考一般的表現及重癥支氣管肺炎的診斷,將病情重或出現嚴重肺外并發癥,或單用大環內酯類抗生素治療1周無反應,或病程超過6周仍遷延不愈的,視為重癥[4]。排除標準如下。①患有肺結核等其他傳染病患兒;②近期有糖皮質激素及免疫抑制劑使用史;③有使用糖皮質激素的禁忌證;④合并細菌、病毒、衣原體等其他病原體感染;⑤病程中需要用激素或其他免疫調節劑者。其中CPIS≥6分為CPIS高分組(21例),CPIS<6分為CPIS低分組(44例)。選擇年齡相匹配在我院體檢的健康兒童30例為正常對照組,均無近期感染,無個人及家族過敏及其他變態反應性疾患史,其中男性17例,女性13例,年齡3~7歲,平均(5.1±1.7)歲。CPIS高分組、低分組及正常對照組3組間性別、年齡差異無統計學意義。
1.2 治療原則:常規抗感染,吸痰叩背、臟器功能支持、霧化吸入、營養代謝支持及維持水、電解質、酸堿平衡等對癥支持治療,避免使用皮質激素等影響免疫功能的藥物。
1.3 檢測方法:上述重癥MPP患兒入院后24h內抽取外周靜脈血,應用流式細胞儀測定CD14+單核細胞HLA-DR表達百分率。靜脈血用乙二胺四乙酸抗凝。取實驗管加入 10μL異硫氰酸熒光素(fluorescein isothiocyanate,FITC)標記小鼠抗人CD14抗體、10μL LPE標記小鼠抗人HLA-DR抗體。對照管加入等體積FITC、PE標記同型小鼠IgG(FITC標記小鼠抗人CD14抗體、PE標記小鼠抗人HLA-DR抗體及相應的同型小鼠免疫球蛋白均為美國BeckmanCoulter公司產品)。再向試管加50μL抗凝靜脈血,混勻,室溫下避光孵育15min,應用Coulter Q-PREP溶血儀溶血后,避光儲存待測。檢驗標本前應用Coulter公司標準液校準流式細胞儀(美國Beckman Coulter公司Coulter EPICSXL型)使流量系數(volume cofficient,CV)值在2%以內。檢測時每管收集100 000個細胞,分別記錄CD14+單核細胞中HLA-DR的陽性率。與此同時,計算出并記錄當天的CPIS。
1.4 統計學方法:應用SPSS11.5軟件進行數據處理。計量資料以±s表示,各指標變化的組間比較采用單因素方差分析。P<0.05為差異有統計學意義。
2 結 果
入院當天CPIS高分組與低分組CD14+單核細胞HLA-DR表達百分率均低于正常對照組,且CPIS高分組低于低分組(P<0.05)。治療后,CPIS高分組和低分組CD14+單核細胞HLA-DR表達百分率均升高,與治療前比較,差異有統計學意義(P<0.01)。見表1。
表1 重癥MPP患兒CD14+單核細胞HLA-DR表達變化Table 1 PeriPheral blood CD14+mononuclera cells HLA-DR exPression in severe MPP children(±s,%)
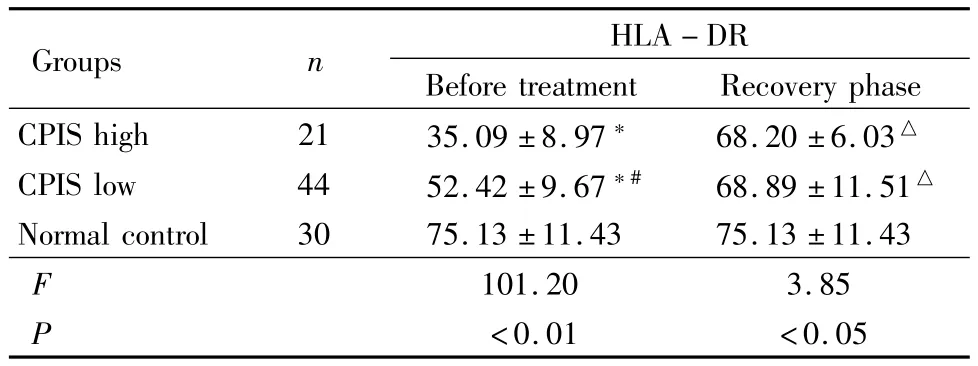
表1 重癥MPP患兒CD14+單核細胞HLA-DR表達變化Table 1 PeriPheral blood CD14+mononuclera cells HLA-DR exPression in severe MPP children(±s,%)
*P<0.01 vs normal control group #P<0.01 vs CPIS high group△P<0.01 vs before treatment by q testHLA-DR:human leukocyte antigen DR;CPIS:clinical pulmonary infection score
HLA-DR Before treatment Recovery phase CPIS high 21 35.09±8.97* 68.20±6.03 Groups n△CPIS low 44 52.42±9.67*# 68.89±11.51△Normal control 30 75.13±11.43 75.13±11.43 F<0.01 <0.05 101.20 3.85 P
3 討 論
MPP是兒童的常見病和多發病,重癥MPP表現為起病急,以劇烈咳嗽、氣喘起病,并很快出現發熱和呼吸困難,肺外并發癥多見,肺部病變嚴重,可合并肺膿腫、大量胸腔積液、壞死性肺炎以及閉塞性支氣管炎或閉塞性毛細支氣管炎等[5]。迄今MPP發病機制還不十分清楚。1996年Bone等[6]針對感染或創傷時導致機體免疫功能的內源性抗炎反應,提出了代償性抗炎癥反應綜合征。重癥MPP可能并不像以往所認為的是“過度炎癥反應”,更多的可能是由于“過度抑制”導致機體“免疫系統發生故障”,不能清除病原體所致[7]。
單核細胞作為機體重要的免疫細胞之一,參與其中每個過程,有著不可或缺的作用。它的功能變化在一定程度上反映機體的免疫功能狀態。CD14+單核細胞HLA-DR是單核吞噬細胞表面的抗原表達,其功能是把經單核吞噬細胞吞噬并處理后的抗原提呈給T輔助細胞,繼而激活包括T細胞、B細胞和吞噬細胞在內的所有免疫細胞,所以,足夠的HLA-DR表達對于特異性免疫和非特異性免疫功能都十分重要。
當前,檢測免疫功能的方法很多,但能夠作為定量的診斷免疫抑制的檢查,目前首推CD14+單核細胞的HLA-DR。Venet等[8]證明,以CD14+單核細胞HLA-DR<30%為閾值能夠可靠地篩選出膿毒癥免疫抑制的患者。他們發現,燒傷后發生膿毒癥患者HLA-DR<30%或持續降低超過5d患者病死率及膿毒血癥發生率遠高于對照組。本研究結果顯示,重癥 MPP患兒的外周血 CD14+單核細胞的HLA-DR表達率明顯低于正常對照組,臨床表現為病情重或出現嚴重肺外并發癥,或單用大環內酯類抗生素治療1周無反應等。提示CD14+單核細胞HLA-DR表達持續低下的患兒處于免疫抑制狀態,易發生持續且嚴重的感染。
CPIS最早由Pugin提出,它將胸部X線片以及實驗室檢驗結果和臨床相結合,用于評估肺部感染嚴重程度,分值越高提示肺部感染越重[9]。本研究結果顯示,重癥 MPP中外周血 CD14+單核細胞HLA-DR表達水平可反映重癥MPP患者肺部感染程度,CD14+單核細胞HLA-DR表達水平越低,肺部感染程度越重。與Gogos等[10]的研究結果一致。
本研究結果顯示,治療后患兒CD14+單核細胞HLA-DR表達百分率均明顯升高,與治療前相比差異有統計學意義(P<0.01)。與文獻報道一致[11]。說明CD14+單核細胞HLA-DR表達可用于判斷MPP患兒病情的嚴重程度,并在重癥MPP的發生發展和疾病轉歸中起重要作用。
[1] CHUNG HL,SHIN JY,JU M,et al.Decrased interleukin-18 response in asthmatic children with severe mycoplasma pneumoniae pneumonia[J].Cytokine,2011,54(2):218-221.
[2] POSCHKE I,MOUGIAKAKOS D,HANSSON J,et al.Immature immunosuppressive CD14+HLA-DR-/low cells in melanoma patients are Stat3hi and overexpress CD80,CD83,and DC-sign[J].Cancer Res,2010,70(11):4335-4345.
[3] 胡亞美,江載芳.諸福棠實用兒科學[M].北京:人民衛生出版社,2002:1204-1205.
[4] 趙順英,馬云,張桂芳,等.兒童重癥肺炎支原體肺炎11例臨床分析[J].中國實用兒科雜志,2003,7(18):414-416.
[5] YOUN YS,LEE KY.Mycoplasma pneumoniae pneumonia in childeren[J].Korean J Pediatr,2012,55(2):42-47.
[6] BONE RC.Immunologic dissonance:a continuing evolution in our understanding of the systemic inflammatory response syndrome(SIRS)and the multiple organ dysfunction syndrome(MODS)[J].Ann Intern Med,1996,125(8):680-687.
[7] MUNETA Y,MINAGAWA Y,SHIMOJI Y,et al.Immune response of gnotobiotic piglets against Mycoplasma hyopneumoniae[J].J Vet Med Sci,2008,70(10):1065-1070.
[8] VENET F,TISSOT S,DEBARD AL,et al.Decreased monocyte human leukocyte antigen-Drexpression after severe burn injury:Correlation with severity and secondary septic shock[J].Crit Care Med,2007,35(8):1910-1917.
[9] BHADADE RR,DE SOUZA RA,HARDE MJ,et al.Clinical characteristices and outcomes of patients with acute lung injury and ARDS[J].J Postgrad Med,2011,57(4):286-290.
[10] GOGOS C,KOTSAKI A,PELEKANOU A,et al.Early alterations of the innate and adaptive statuses in sepsis according to the type of underlying infection[J].Crit Care,2010,14(3):R96.
[11] HUANG SW,CHEN J,OUYANG B,et al.Immunotherapy improves immune homeostasis and increases survial rate of septic patients[J].Chin J Traumatol,2009,12(6):344-349.
(本文編輯:劉斯靜)
OBSERVATION OF THE EXPRESSION OF CD14+MONOCYTE HUMAN LEUKOCYTE ANTIGEN DR IN SEVERE MYCOPLASMA PNEUMONIAE PNEUMONIA
SUN Haiying1,SHAO Xiaoli2*,LIU Shumei2,GUO Ping2,ZHOU Guozhong3,CHEN Yi2
(1.Department of Pediatrics,Shaoxing County Maternity and Child Care Centers,Zhejiang Province,Shaoxing 312030,China;2.Department of Pediatrics,Shaoxing People′s Hospital&Zhejiang University Shaoxing Hospital,Zhejiang Province,Shaoxing 312000,China;3.Department of Medical Molecular Biology,Shaoxing People′s Hospital&Zhejiang University Shaoxing Hospital,Zhejiang Province,Shaoxing 312000,China)
ObjectiveTo monitor the change of the expression of CD14+monocyte human leukocyte antigen DR(HLA-DR)in severe mycoplasma pneumoniae pneumonia children and evaluate their immunological condition,relationship between severity of illness,prognosis and CD14+monocyte HLA-DR.MethodsSixth-five cases of severe mycoplasma pneumoniae pneumonia children were collected and divided into the following groups,total 44 cases with clinical pulmonary infection score(CPIS)≥6 were CPIS high grade;total 21 cases with CPIS<6 were CPIS low grade,and 30 normal cases were selected as control group.The levels of venous blood CD14+monocyte HLA-DR were detected at the first day after admission and discharge.The CPIS grade of the patients was recorded at the first day after admission.ResultsThe levels of CD14+monocyte HLA-DR in severe mycoplasma pneumoniae pneumonia were obviously lower no matter in CPIS high grade and in CPIS low grade than normal cases with statistically significant differences(P<0.01),and the level in CPIS high grade waslower than the CPIS low grade(P<0.01).The levels of CD14+monocyte HLA-DR in the 2 groups were increased significantly after treatment(P<0.01).ConclusionPersistent low level of the expression of CD14+monocyte HLA-DR in severe mycoplasma pneumoniae pneumonia indicate the patients are in the states of immunosuppression.Detection of the expression of CD14+monocyte HLADR can be used to evaluate the severity of disease and predict prognosis in severe mycoplasma pneumoniae pneumonia.
pneumonia,mycoplasma;antigens,CD14;child
R563.1
A
1007-3205(2012)09-1021-04
2012-01-30;
2012-04-28
孫海英(1977-),女,浙江紹興人,浙江省紹興縣婦幼保健所主治醫師,醫學學士,從事小兒呼吸內科疾病診治研究。
*通訊作者。E-mail:nuannuan717@126.com
10.3969/j.issn.1007-3205.2012.09.011