阻塞性睡眠呼吸暫停低通氣綜合征與高血壓的相關性及危險因素分析
朱小川 儲德節 洪燕 胡辛 俞靜 莊遠非 方子睿
(上海市第八人民醫院呼吸科, 上海 200235)
·論著·
阻塞性睡眠呼吸暫停低通氣綜合征與高血壓的相關性及危險因素分析
朱小川儲德節洪燕胡辛俞靜莊遠非方子睿
(上海市第八人民醫院呼吸科, 上海200235)
摘要目的:探討阻塞性睡眠呼吸暫停低通氣綜合征(OSAHS)與高血壓的關系及其危險因素,為預防和治療OSAHS合并高血壓提供依據。方法: 選擇OSAHS患者共108例,記錄一般情況,測定患者22∶00和8∶00的血壓,檢測血脂水平。根據呼吸暫停低通氣指數(AHI)將108例患者分為3組。輕度組:5次/h≤AHI<15次/h,31例;中度組:15次/h≤AHI<40次/h,36例;重度組:AHI≥40次/h,41例。比較各組的血壓水平。根據OSAHS患者是否合并高血壓,將患者分為單純OSAHS組及OSAHS合并高血壓組。通過單因素分析篩選與OSAHS合并高血壓相關的因素,然后進行Logistic多因素回歸分析。結果: (1)108例OSAHS患者中合并高血壓60例(55.6%),其中輕度組15例(48.4%,15/31),中度組19例(52.8%,19/36),重度組26例(63.4%,26/41);3組間高血壓的患病率差異無統計學意義(P>0.05)。3組間22∶00和8∶00的收縮壓(SBP)、舒張壓(DBP)比較,差異均有統計學意義(P<0.05)。重度組22∶00和8∶00 SBP、DBP明顯高于輕度組(P<0.05),重度組22∶00和8∶00 SBP明顯高于中度組(P<0.05)。(2)單因素分析結果顯示,OSAHS合并高血壓組的年齡、體質量指數(BMI)、吸煙率、腹圍、AHI、總膽固醇(TC)、三酰甘油(TG)及低密度脂蛋白膽固醇(LDL-C)均高于單純OSAHS組(P<0.05),而高密度脂蛋白膽固醇(HDL-C)低于單純OSAHS組( P<0.05)。(3)多因素Logistic回歸結果顯示,BMI、AHI、TC為OSAHS合并高血壓的危險因素。結論: OSAHS患者高血壓的水平與其病情嚴重程度具有一致性,而BMI、AHI、TC為OSAHS合并高血壓的危險因素。
關鍵詞阻塞性睡眠呼吸暫停低通氣綜合征;高血壓;危險因素;相關性
Analysis of Correlation between Obstructive Sleep Apnea Hypopnea Syndrome and Hypertension and Risk FactorsZHUXiaochuanCHUDejieHONGYanHUXinYUJingZHUANGYuanfeiFANGZiruiShanghaiEighthPeople’sHospital,Shanghai200235,China
AbstractObjective: To investigate the correlation between obstructive sleep apnea hypopnea syndrome (OSAHS) and hypertension and its risk factors, so as to provide basis for prevention and treatment of OSAHS accompanied by hypertension. Methods: A total of 108 OSAHS patients were enrolled and the general conditions were recorded. The blood pressure at 22∶00 before sleep and that at 8∶00. next morning was determined routinely, and the blood lipid level was detected. According to apnea hypoapnea index (AHI), the patients were divided into three groups, the mild group (5/h≤AHI<15/h) with 31 cases, the moderate group (15/h≤AHI<40/h) with 36 cases, and the severe group (AHI ≥40 /h) with 41 cases. The levels of blood pressure were compared among the groups. According to whether OSAHS was accompanied by hypertension, the patients were divided into simple OSAHS group and OSAHS accompanied by hypertension group. The relevant factors associated with OSAHS accompanied by hypertension were screened out by single factor analysis, and then the multiple Logistic regression analysis was conducted. Results: (1)Among 108 patients with OSAHS,60 cases(55.6%) were accompanied by hypertension, including 15 cases of mild group(48.4%, 15/31), 19 cases of moderate group (52.8%, 19/36), and 26 cases of severe group(63.4%, 26/41). There was no significant difference regarding the prevalence rate of hypertension among the three groups (P>0.05). There were significant differences regarding systolic blood pressure(SBP) and diastolic blood pressure (DBP) at 22∶00 and 8∶00 among the three groups (P<0.05); SBP and DBP at 22∶00 and 8∶00 in severe group were significantly higher than those in mild group (P<0.05). SBP at 22∶00 and 8∶00 in severe group was significantly higher than that in moderate group (P<0.05).(2) Single factor analysis showed that age, body mass index(BMI), smoking rate, abdominal circumference, AHI, total cholesterol(TC), triglyceride(TG) and low density lipoprotein cholesterol (LDL-C) in OSAHS accompanied by hypertension group were significantly higher than those in simple OSAHS group, while HDL-C was significantly lower than that in simple OSAHS group (P<0.05). (3) Multivariate Logistic regression analysis showed that BMI, AHI, TC were the risk factors for OSAHS accompanied by hypertension. Conclusions: The level of blood pressure in patients with OSAHS was accordance with the disease severity, while BMI, AHI, TC were the risk factors for OSAHS accompanied by hypertension.
Key WordsObstructive sleep apnea hypopnea syndrome;Hypertension;Risk factor;Correlation
阻塞性睡眠呼吸暫停低通氣綜合征(obstruc-tive sleep apnea hypopnea syndrome, OSAHS)是一組睡眠期疾病,主要原因為睡眠中反復發生上氣道阻塞而引起呼吸暫停和低通氣,進而導致低氧血癥、高碳酸血癥和睡眠結構紊亂。OSAHS患者表現為白天嗜睡、合并心腦血管疾病甚至多臟器損害。OSAHS與高血壓之間存在密切關系[1]。汪迎春等[2]報道, 30%~50%OSAHS患者合并高血壓,而70%的頑固性高血壓患者存在OSAHS。本研究比較了不同程度OSAHS患者的血壓及相關生化指標之間的差異,并分析了OSAHS合并高血壓的危險因素。
1資料與方法
1.1一般資料選擇2013年1月—2015年3月在我院呼吸科經多導睡眠圖(polysomnogram,PSG)監測后診斷為OSAHS的108例患者,其中男性83例,女性25例;年齡37~76歲,平均年齡(53.4±9.8)歲。根據臨床及實驗室檢查結果排除卒中、糖尿病、肝腎功能障礙等嚴重疾病,剔除有哮喘和慢性阻塞性肺疾病的患者,入選患者在入院前均未經過OSAHS規范治療。
根據中華醫學會的OSAHS診斷標準和病情分度標準[3]對108例患者分組。輕度組:5次/h≤呼吸暫停低通氣指數(AHI)<15次/h,31例;中度組:15次/h≤AHI<40次/h,36例;重度組:AHI≥40次/h,41例。
1.2研究方法患者入院后進行體格檢查。記錄患者的年齡、性別、身高、體質量、頸圍、腹圍以及吸煙史、飲酒史和高血壓家族史等。患者入院次日晨空腹抽取靜脈血,檢測血糖(FBG) 、三酰甘油(TG) 、總膽固醇(TC) 、高密度脂蛋白膽固醇(HDL-C) 、低密度脂蛋白膽固醇( LDL-C)等指標。入院當晚應用德國萬曼公司的Somnolab2多導睡眠監測系統行PSG檢查。患者均于22∶00和次日8∶00用汞柱式血壓計測量血壓,測量前至少休息5 min,測量2次右上臂肱動脈血壓,取平均值。高血壓的診斷參照《中國高血壓防治指南》(2010年)的診斷標準:未用降壓藥物且非同日3次測量血壓,收縮壓≥140 mmHg(1 mmHg=0.133 kPa)和(或)舒張壓≥90 mmHg。

2結果
2.1各組高血壓發生率及血壓水平比較108例OSAHS患者中合并高血壓者60例(55.6%),其中輕度組15例(48.4%,15/31),中度組19例(52.8%,19/36),重度組26例(63.4%,26/41),3組間高血壓患病率差異無統計學意義(P>0.05)。3組間22∶00和8∶00的SBP、DBP比較,差異均有統計學意義(P<0.05);重度組22∶00和8∶00的SBP、DBP明顯高于輕度組(P<0.05),重度組22∶00和8∶00的SBP明顯高于中度組(P<0.05)。見表1。
2.2OSAHS合并高血壓的相關指標分析根據OSAHS患者是否合并高血壓,將患者分為單純OSAHS組(n=48)及OSAHS合并高血壓組(n=60)。OSAHS合并高血壓組的年齡、體質量指數(BMI)、吸煙比例、腹圍、AHI、TC、TG及LDL-C均明顯高于單純OSAHS組(P<0.05),而HDL-C明顯低于單純OSAHS組(P<0.05)。見表2。
2.3OSAHS合并高血壓的危險因素分析以OSAHS患者是否發生高血壓作為因變量,其中未合并高血壓定義為“0”,而合并高血壓定義為“1”;將單因素分析顯示有意義的變量即年齡、BMI、吸煙、腹圍、AHI、TC、TG、LDL-C及HDL-C作為自變量,采用逐步回歸法對各變量進行分析。多因素Logistic回歸模型顯示,BMI、AHI、TC為OSAHS合并高血壓發病的危險因素。見表3。
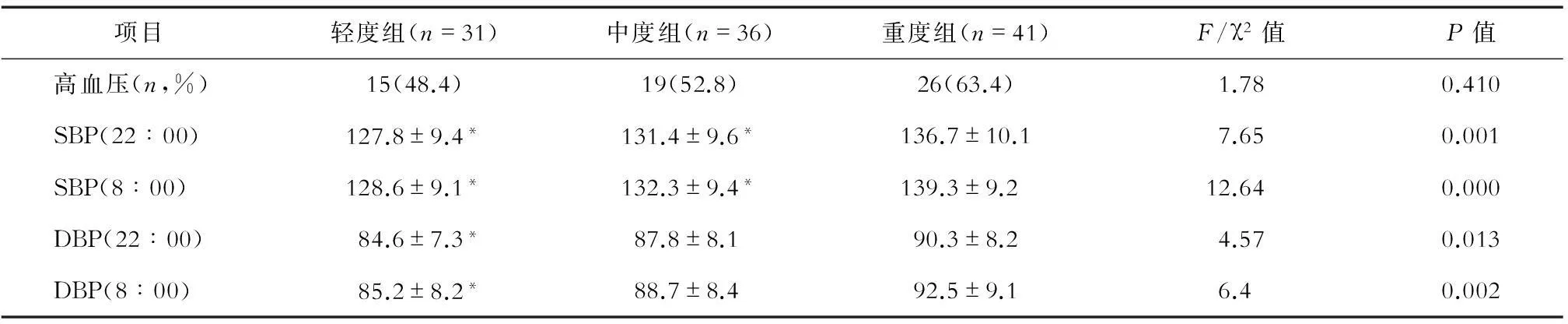
表1 各組患者高血壓的發生率及血壓水平比較
注:與重度組比較,*P<0.05
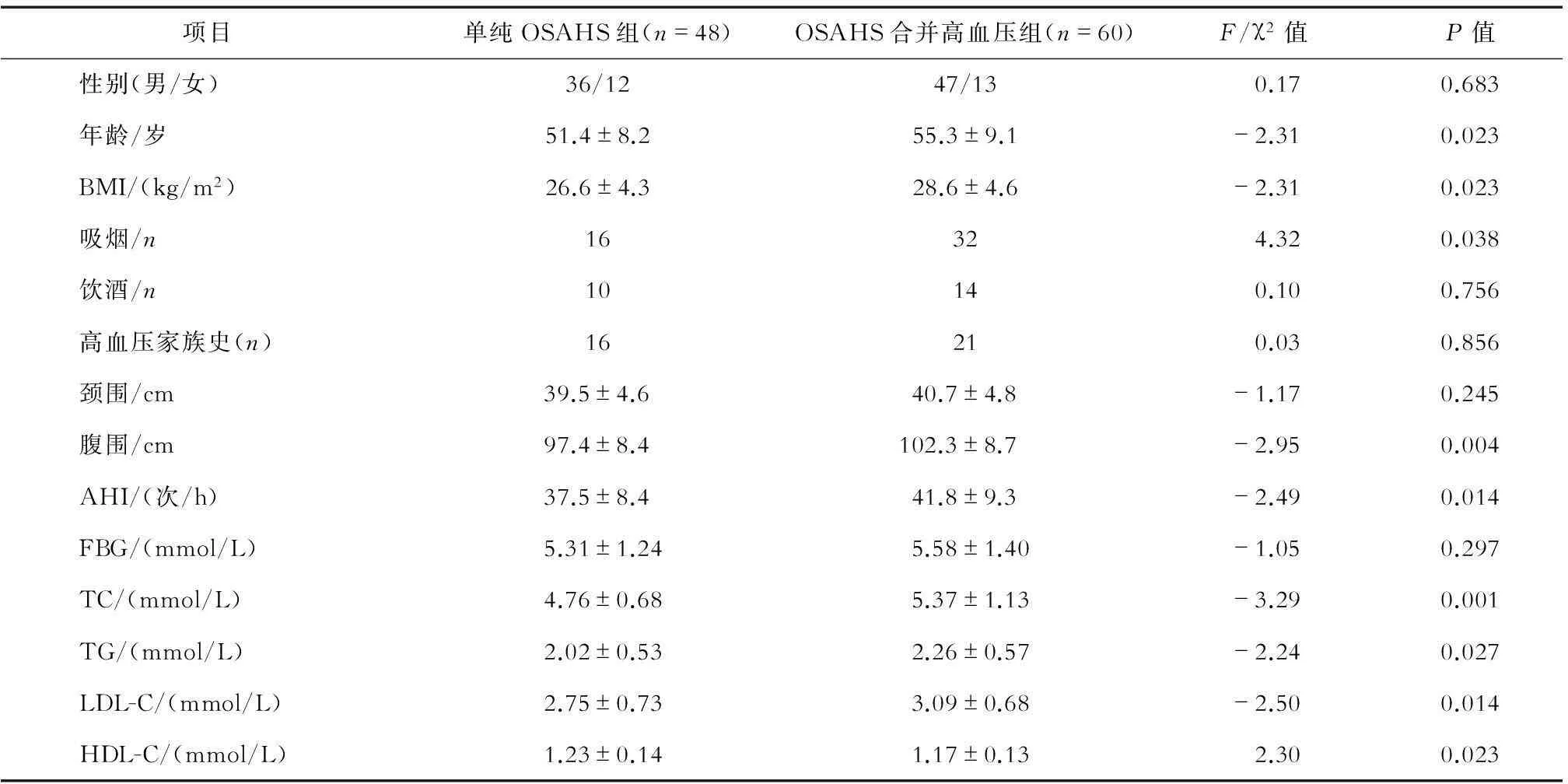
表2 OSAHS合并高血壓的相關指標分析
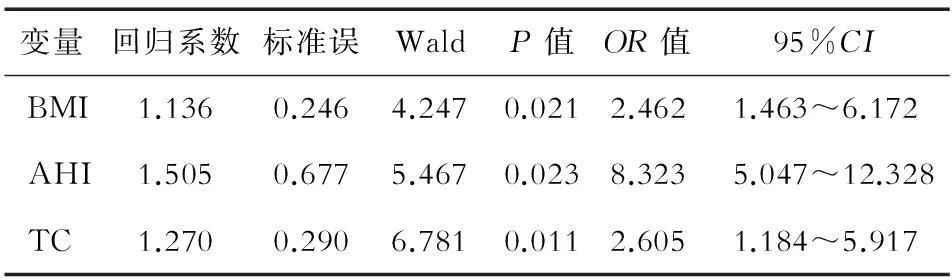
表3 多因素非條件Logistic回歸分析結果
注:OR為優勢比;95%CI為95%可信區間
3討論
OSAHS與高血壓密切相關。有研究[4-5]表明,OSAHS是除性別、年齡、飲酒、精神緊張及心、腎疾病外引起高血壓的獨立危險因素;美國國家聯合委員會第7次報告提出,將OSAHS列于繼發性高血壓發病原因的首位。然而,關于OSAHS 導致高血壓的原因及其機制,目前尚未完全清楚。本研究的108例OSAHS患者中高血壓的患病率為55.6%,輕度組、中度組、重度組高血壓的患病率分別為48.4%、52.8%、63.4%。雖然3組間差異無統計學意義(P>0.05),但高血壓的患病率有隨著OSAHS的嚴重程度而不斷升高的趨勢,今后有待通過大樣本研究進一步論證。OSAHS發生的病理生理機制為:睡眠過程中反復發生的呼吸暫停和低通氣引起低氧血癥和高碳酸血癥,進而刺激中樞和心血管化學感受器,使交感神經興奮[6]。缺氧和交感神經興奮可引起夜間頻繁的暫時性血壓升高,早期表現為晨醒血壓升高,長期則導致血管結構改變,引起高血壓。本研究對108例OSAHS患者測定22∶00和8∶00的血壓。結果顯示,3組不同嚴重程度的OSAHS患者比較,22∶00和8∶00的SBP、DBP的組間差異有統計學意義(P<0.05);重度組22∶00和8∶00的SBP、DBP明顯高于輕度組,重度組22∶00和8∶00的SBP明顯高于中度組,差異有統計學意義(P<0.05)。
OSAHS與性別、年齡、肥胖、家族史、吸煙、飲酒及顱面畸形等有關[7],但關于OSAHS合并高血壓的危險因素國內外報道較少。本研究中的多元回歸分析結果顯示,BMI、AHI、TC為OSAHS合并高血壓發病的危險因素。BMI是衡量人體胖瘦程度的指標。肥胖患者頸部和下頜部的脂肪組織較厚,導致患者口咽部及喉咽部的腔外壓增高,因此吸氣時咽部容易塌陷。Hu等[8]將727例OSAHS患者按照BMI分為3組(BMI<25,n=201;25≤BMI<29.99,n=388;BMI≥30,n=138);共有244(33.6%)例患者合并高血壓,BMI<25、25≤BMI<29.99、BMI≥30組患者高血壓的患病率分別為24.9%(50/201)、33.2%(129/388)和47.1%(65/138);BMI與OSAHS患者高血壓的發生明顯正相關。威斯康辛隊列研究[9]顯示,AHI≥15次/h的OSAHS患者發生高血壓的風險增加3倍。Li等[10]將1 149例OSAHS疑似患者根據AHI分成10組,結果顯示,AHI與舒張壓、收縮壓正相關(r分別為0.239和0.305,P<0.01);隨著OSAHS病情的加重,高血壓發病率明顯升高,并在AHI 30次/h和50次/h處出現兩個明顯截點。本研究顯示,OSAHS合并高血壓患者的血漿TC水平明顯升高。研究[11]證實,高血壓患者可出現血脂代謝異常,而血脂水平升高是高血壓的獨立危險因子。Toyama等[12]報道,AHI與血TG水平明顯正相關,而睡眠持續時間與血TC、LDL水平明顯負相關。大量動物及臨床試驗證據表明,OSAHS可以導致血脂代謝發生改變,主要表現為TC、LDL及TG的升高[13]。本研究中單因素分析顯示,年齡、吸煙、腹圍、TG、LDL-C及HDL-C是OSAHS合并高血壓的危險因素,但多因素分析并未將它們納入Logistic回歸模型,這一結果可能與入選患者的樣本量偏少有關,有待今后進一步進行大樣本研究。
綜上所述,OSAHS患者高血壓的水平與OSAHS病情嚴重程度有一致性,而BMI、AHI、TC為OSAHS患者合并高血壓的危險因素。因此,應在OSAHS患者中加強預防和治療高血壓,控制相關危險因素,以降低OSAHS合并高血壓的發病率。
參考文獻
[ 1 ]Li J, Chen X, Sun J. Is the grading system of the severity of the OSAHS used presently rational or not?: from the view of incidence of hypertension in different severity groups[J]. Eur Arch Otorhinolaryngol, 2014, 271(9): 2561-2564.
[ 2 ]汪迎春,歐陽瑋琎,李南方,等.高血壓合并阻塞性睡眠呼吸暫停低通氣綜合征患者血壓水平及血壓變異性分析[J].中國心血管雜志,2011,16(5):348-351.
[ 3 ]中華醫學會呼吸病學會睡眠呼吸疾病學組.阻塞性睡眠呼吸暫停綜合征診治指南(草案)[J]. 中華結核和呼吸雜志,2002,25(4):195-198.
[ 4 ]Sova M, Sovová E, Hobzová M, et al. Research of relations among sleep disorders, obstructive sleep apnoea, hypertension onset and hypertensive treatment-current or long-term trend[J]. Vnitr Lek, 2015, 61(1): 50-55.
[ 5 ]Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea-Implications for cardiac and vascular disease[J]. JAMA, 2003, 290(14): 1906-1914.
[ 6 ]韓瑞梅,李南方,嚴治濤,等.阻塞性睡眠呼吸暫停相關性高血壓患者血壓節律影響因素分析[J].中華高血壓雜志,2013,41(9):751-755.
[ 7 ]汪小亞,余勤.成人阻塞性睡眠呼吸暫停低通氣綜合征流行病學研究進展[J].國際呼吸雜志,2009,29(5):290-294.
[ 8 ]Hu W, Jin X, Gu J, et al. Risk factor panels associated with hypertension in obstructive sleep apnea patients with different body mass indexes[J]. J Am Soc Hypertens, 2015, 9(5): 382-389.
[ 9 ]殷忠,楊曄.阻塞性睡眠呼吸暫停綜合征與心血管疾病[J].中華老年心腦血管病雜志,2010,12(12):1143-1145.
[10]Li JR, Chen X, Sun JJ. Relationship between obstructive sleep apnea-hypopnea syndrome and hypertension[J]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi, 2012, 47(2): 97-100.
[11]董健,于宏.原發性高血壓與血漿同型半胱氨酸及血脂的關系[J].中國慢性病預防與控制,2013,21(3):368-369.
[12]Toyama Y, Chin K, Chihara Y, et al. Association between sleep apnea, sleep duration, and serum lipid profile in an urban, male, working population in Japan[J]. Chest, 2013, 143(3): 720-728.
[13]王明輝.阻塞性睡眠呼吸暫停低通氣綜合征與冠心病及其危險因素的關系[C].天津:天津醫科大學,2013:20.
中圖分類號R 563
文獻標識碼A
通訊作者儲德節, E-mail: djchu@sina.com

