Outcomes in 334 cases of Millions of Poor Cataract Patients’ Extraction Project in Shanxi Province
Hong Zhang, Fang-Fang Wang, Wen-Jie Liu, Jiang-Li Dai, Kui Dong, Yuan-Yuan Gong, Li Wang,2
?
Outcomes in 334 cases of Millions of Poor Cataract Patients’ Extraction Project in Shanxi Province
Hong Zhang1, Fang-Fang Wang1, Wen-Jie Liu1, Jiang-Li Dai1, Kui Dong1, Yuan-Yuan Gong1, Li Wang1,2
1Shanxi Eye Hospital, Taiyuan 030002, Shanxi Province, China;
2Department of Ophthalmology, Baylor College of Medicine, Houston, Texas, 77030, USA
Correspondence to:Hong Zhang. Shanxi Eye Hospital, Taiyuan 030002, Shanxi Province, China.sxzhanghong@126.com
Received: 2015-12-21Accepted: 2016-07-05
目的:了解中國山西省貧困白內障患者術后視力、視功能和生存質量的變化,分析貧困白內障患者手術成本/效果。
方法:采用回顧性方法,對334例334眼接受貧困白內障復明手術的患者進行基本情況、術前及術后1wk視力、術中并發癥、術后并發癥的病歷采集及現場調查,對其中83例進行視功能和生存質量調查,225例貧困白內障患者和120例非貧困白內障患者進行手術成本/效果的對比分析,使用多重線性回歸模型及Logistic回歸模型進行術后視力影響因素分析。
結果:患者術后1wk視力明顯高于術前視力(P<0.05),其中術后1wk視力≥0.5的為235例(70.4%)、視力<0.05的為16例(4.8 %)。多重線性回歸分析顯示,眼部其他疾病、白內障分類是術后視力的影響因素。logistic回歸分析顯示,術前視力低、眼部有其他疾病是術后低視力的危險因素,其OR值及其95%CI依次為6.5 (2.8-14.8)和1.3 (1.0-1.6)。術后視功能以及生存質量均高于術前。貧困白內障患者手術成本/效果低于非貧困白內障。
結論:貧困白內障患者術后視力、視功能明顯提高,且手術成本低,顯著改善了生活質量。
引用:張紅,王芳芳,劉文潔,戴江麗,董魁,龔元元,王莉. 中國山西334例“百萬貧困白內障患者復明工程”手術效果分析.國際眼科雜志2016;16(8):1397-1401
Abstract
?AIM: To evaluate the visual acuity, visual function, quality of life, and cost/effectiveness of cataract surgery in patients with low socioeconomic status (LSES) who received government subsidies for free cataract surgery.
?METHODS: Retrospectively, 334 eyes of 334 patients were reviewed. Visual function and quality of life questionnaires were available in 83 patients. The cost/effectiveness of cataract surgery was analyzed in 225 patients with LSES and 120 patients who received standard cataract surgery. Multiple linear regression analysis and logistic regression analysis were used to assess the factors affecting the postoperative visual acuity.
?RESULTS: At 1wk postoperatively, uncorrected visual acuity (UCVA) was improved significantly compared to these preoperatively (P<0.05), 235 eyes (70.4%) had UCVA of 20/40 or better, and 16 eyes (4.8%) had UCVA worse than 20/400. Multiple linear regression analysis revealed that other ocular diseases and cataract classification were factors contributing to postoperative UCVA. Logistic regression analysis showed that low preoperative visual acuity and other ocular diseases were risk factors of postoperative low vision, and the odds ratio (95% confidence interval) values were 6.5 (2.8-14.8) and 1.3 (1.0-1.6), respectively. Visual function and quality of life were significantly improved after the surgery. The cost/effectiveness of cataract surgery in patients with LSES was lower than that in standard cataract patients.
?CONCLUSION: Visual acuity and visual function were significantly better after the surgery in cataract patients with LSES, and the operation cost was low. Quality of life in these patients was significantly improved.
KEYWORDS:?Millions of Poor Cataract Patients’ Extraction Project; postoperative visual acuity and visual function; analysis of quality of life
Citation:Zhang H, Wang FF, Liu WJ, Dai JL, Dong K, Gong YY, Wang L. Outcomes in 334 cases of Millions of Poor Cataract Patients’ Extraction Project in Shanxi Province.GuojiYankeZazhi(IntEyeSci) 2016;16(8):1397-1401
INTRODUCTION
Shanxi is a low-income province in China. In 2009, the Chinese government implemented a special program (Millions of Poor Cataract Patients’ Extraction Project) using specific fund, in which cataract patients with low socioeconomic status (LSES) received free cataract surgery. The purpose is to eliminate the blindness caused by cataract. Surgical treatment is the main approach to prevent blindness in cataract patients[1]. Between 2009 and 2012, in Shanxi Province, 45 034 free cataract surgeries were performed in patients with LSES in 115 hospitals using this government fund. Of these cases, 19 802 (44%) cases were performed in county (district) level general hospitals, 20 321 cases (45%) in specialized ophthalmic hospitals, and 4911 cases (11%) in large general hospitals.
In a previous study, we investigated the eye care status in Millions of Poor Cataract Patients’ Extraction Project[2]. In this study, we evaluated the visual acuity, visual function, and quality of life in these patients with LSES following the cataract surgery, preoperative factors contributing to postoperative visual acuity, and the cost/effectiveness of cataract surgery in patients with LSES.
SUBJECTS AND METHODS
SubjectsRetrospectively, we reviewed consecutive patients who participated in the special program Millions of Poor Cataract Patients’ Extraction Project between Apr. 2011 and Sep. 2014.
Before the surgery, ocular biometry was measured using the partial coherence interferometer (IOLMaster, Carl Zeiss Meditec Inc., Oberkochen, Germany), immersion A-scan, or applanation A-scan. Intraocular lens (IOL) power calculation was done using SRK/T formula. Small incision cataract surgery with phacoemulsification and spherical IOL implantation was performed in 334 eyes of 334 patients. Of the 334 eyes, 179 (53.6%) eyes were operated in specialized ophthalmic hospitals and 155 (46.4%) eyes had surgery in general hospitals. All cataract surgeries were performed by certified cataract surgeon.
Survey MethodologyThis research was approved by the ethics committee and the study adhered to the tenets of the Declaration of Helsinki. Patients’ charts were reviewed and demographic characteristics were recorded, including name, gender, age, etc. Before and 1wk after the surgery, patients received detailed binocular eye exam, including visual acuity, anterior segment and fundus examination. Visual acuity was tested using the international standard Snellen decimal visual acuity chart, and then converted to logMAR visual acuity for data analysis. Patients also completed the visual function and quality of life questionnaires.
The visual function and quality of life questionnaires used in this study are those designed for developing countries by the World Health Organization and National Eye Institute,USA (NEI-VFQ)[3-4]. Visual function questionnaire consists of 13 questions to assess the following 4 aspects: limitation in daily activity (questions 2 - 5), peripheral vision (question 6), adaptation (questions 7a, 7b, 8a, 9a, 11a and 11b), and stereo vision (question 10). Quality of life questionnaire was used to measure the overall quality of life, consisting of 11 questions that covered 4 aspects:self-care (bathing, eating, and dressing), general daily activity (walking to the neighbor, shopping, and housework), social activity (attending party and meeting people), and psychologic stress (self-contempt, emotion, and self-confidence).
Participating researchers had rigorous training. To ensure the data reliably and comparably, one examiner filled out and completed the questionnaires in all subjects.
Data AnalysisPatients were divided into subgroups according to age ( ≤49 y, 50-59y,60-69y, and ≥ 70y), gender, duration of poor vision preoperatively (< 1y, 1-3y, 4-6y, 7-10y, and >10y), other diseases (diabetes, hypertension, diabetes and hypertension, and other), cataract classification (senile, traumatic, secondary caused by other eye conditions, and metabolic) , and other ocular diseases (corneal diseases, glaucoma, high myopia, uveitis, ocular trauma, and fundus lesions).
A subset of eyes (83 eyes) was randomly selected for visual function and quality of life analyses. A simple scoring method was used for the visual function and quality of life questionnaire results with ranges from 1 to 4. A score of 1 represents extreme difficulty and 4 as no difficulty at all. In order to make the starting point of each index score and maximum score in the same level, all scores were transformed into a score between 0 and 100, with 0 indicating the maximum degree of difficulty, and 100 representing no difficulty at all. This means the higher a score, the better subjective visual function and quality of life are.
The cost/effectiveness analysis is a form of analysis that compares the relative costs and outcomes (effects) of two or more courses of action. It is expressed in terms of a ratio where the denominator is a gain in health from a measure and the numerator is the total cost associated with the health gain. In this study, uncorrected visual acuity (UCVA) of 20/40 or better following cataract surgery was defined as successful, and the success rate for cataract surgery was calculated as the ratio of number of eyes with UCVA of 20/40 or better to total number of eyes. Then, the success rate for cataract surgery and the total cost of hospitalization were used in the cost/effectiveness analysis.
Statistical AnalysisThe SPSS version 22.0(IBM American, USA) was used in this study. The Student’s-ttest, Chi-square test, multiple linear regression, and logistic regression model were performed for statistical analysis. AP<0.05 was considered as statistically significant.
RESULTS
Totally 334 eyes of 334 patients were included; 117 patients (35%) were male and 217 patients were female. Of these patients, 12 patients aged ≤49y, 54 patients aged 50-59y, 102 patients aged 60-69y, and 166 patients aged ≥70y.
Visual AcuityThe mean UCVA values were 1.48±0.58 (LogMAR, mean ± standard deviation) preoperatively and 0.36±0.41 at 1wk postoperatively; there was significant improvement (t=34.139,P<0.01). The percentages of eyes with UCVA of <20/400, 20/400-20/70, 20/70-20/40, and ≥20/40 before and 1wk after the surgery are listed in Table 1, and postoperative UCVA was significantly better than that preoperatively (χ2=428.50,P<0.01).
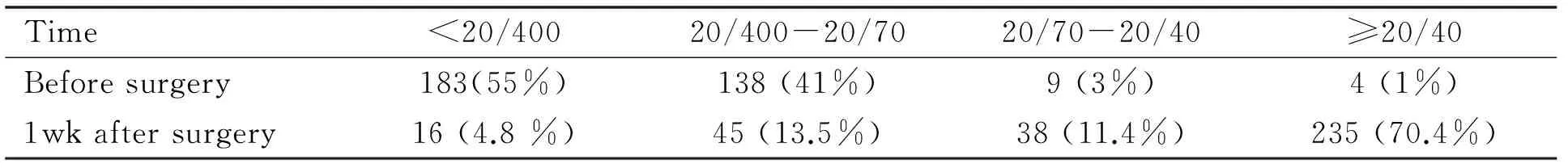
Table 1 Uncorrected visual acuity before and 1wk after the surgery (n=334)
Table 2Factors associated with postoperative visual acuity
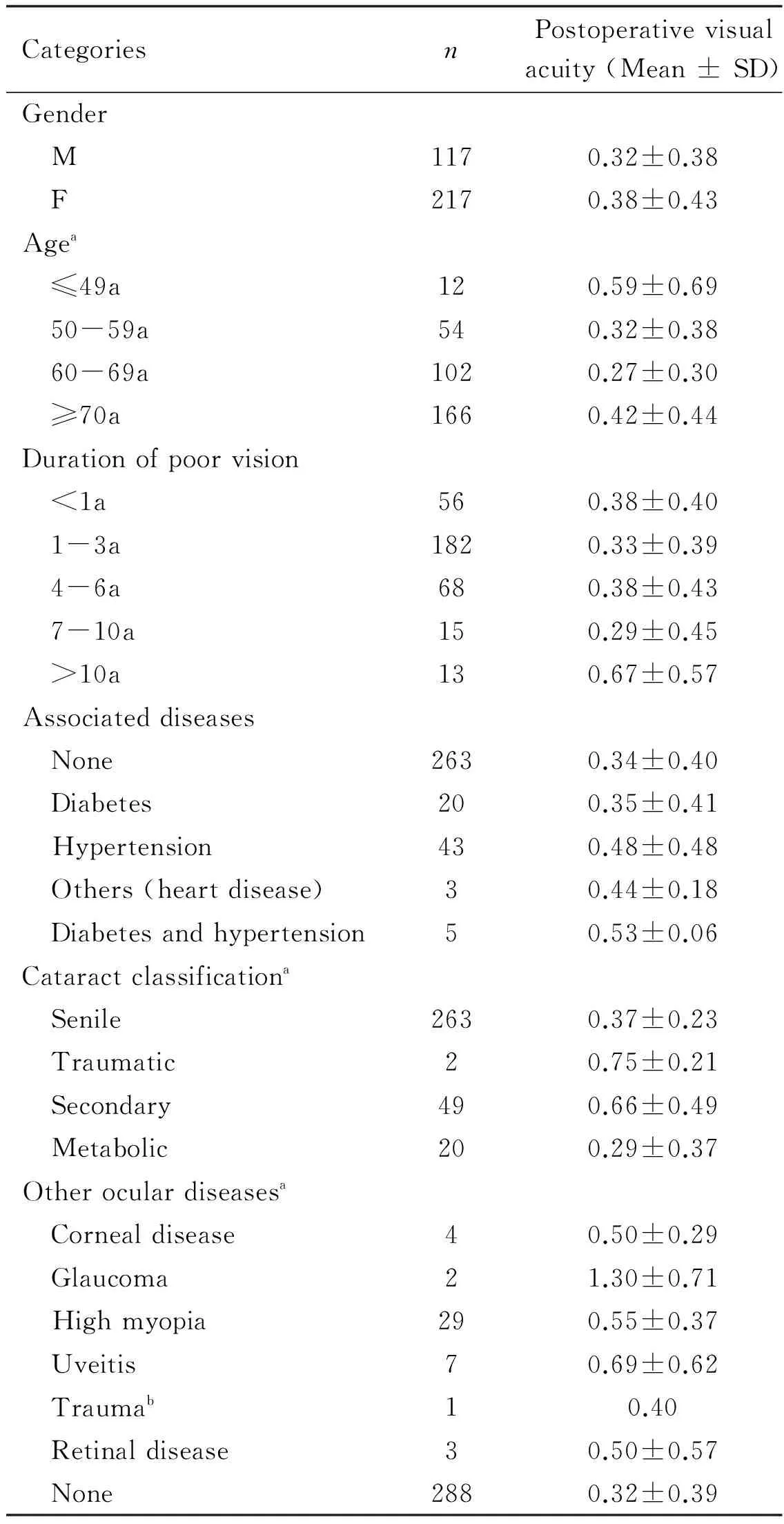
CategoriesnPostoperativevisualacuity(Mean±SD)Gender M1170.32±0.38 F2170.38±0.43Agea ≤49a120.59±0.69 50-59a540.32±0.38 60-69a1020.27±0.30 ≥70a1660.42±0.44Durationofpoorvision <1a560.38±0.40 1-3a1820.33±0.39 4-6a680.38±0.43 7-10a150.29±0.45 >10a130.67±0.57Associateddiseases None2630.34±0.40 Diabetes200.35±0.41 Hypertension430.48±0.48 Others(heartdisease)30.44±0.18 Diabetesandhypertension50.53±0.06Cataractclassificationa Senile2630.37±0.23 Traumatic20.75±0.21 Secondary490.66±0.49 Metabolic200.29±0.37Otheroculardiseasesa Cornealdisease40.50±0.29 Glaucoma21.30±0.71 Highmyopia290.55±0.37 Uveitis70.69±0.62 Traumab10.40 Retinaldisease30.50±0.57 None2880.32±0.39
aP<0.05;bThere is only one eye with trauma, so we cannot calculate the SD value.
Factors Associated with Postoperative Visual AcuityTable 2 shows that age was a significant factor that contributed to postoperative visual acuity; patients with ages between 60-69y had better UCVA than patients with ages of ≤49y and of ≥70y (bothP<0.01). Cataract classification was also a significant factor contributing to postoperative visual acuity; patients with senile cataract and metabolic cataract had better postoperative visual acuity, compared to patients with secondary cataracts and traumatic cataracts (bothP<0.01). Other ocular diseases was a significant factor as well; patients with no other ocular diseases had better postoperative visual acuity, compared to patients with glaucoma, high myopia, and uveitis (allP<0.01). Postoperative visual acuity was not associated with gender, duration of poor vision preoperatively, or associated diseases (allP>0.05).
Table 3Multiple regression analysis investigating factors associated with postoperative visual acuity
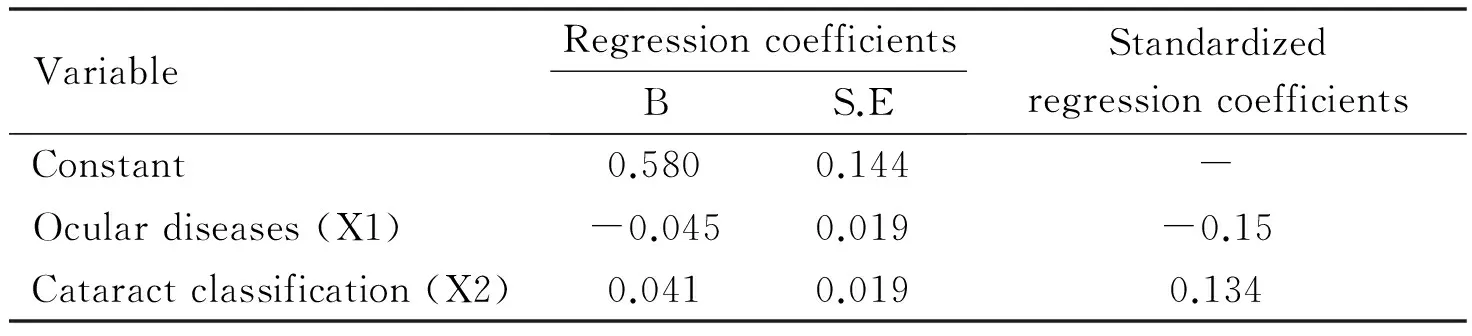
VariableRegressioncoefficientsBS.EStandardizedregressioncoefficientsConstant0.5800.144-Oculardiseases(X1)-0.0450.019-0.15Cataractclassification(X2)0.0410.0190.134
F=10.933,P<0.001.
Multiple regression analysis, adjusting for potentially confounding variables that have been included in the model, revealed that other ocular disease and cataract classification were significant factors for postoperative visual acuity (Table 3). The regression equation was follows:
Y=0.580-0.045X1+0.041 X2
Postoperative Low VisionPostoperative low vision (UCVA <20/70) occurred in 18.2% of eyes (61/334). The duration of poor vision preoperatively, associated disease, cataract classification, other ocular diseases, and preoperative visual acuity were significant factors for postoperative low vision (allP<0.05) (Table 4).
Postoperative Low Vision Logistic Regression AnalysisLogistic regression analysis showed that preoperative low vision and associated other ocular diseases were risk factors for postoperative low vision. The odds ratio (OR) and 95% confidence interval were 6.5 (2.8-14.8) and 1.3 (1.0-1.6), respectively.
Visual Function and Quality of LifeFollowing the cataract surgery, patients’ visual function and quality of life were significantly improved, compared to those before the surgery (allP<0.05) (Table 5).
Intraoperative and Postoperative ComplicationsTable 6 shows the intraoperative and postoperative complications. Intraoperatively, 22 eyes (6.6%) had posterior capsular tear, 5 eyes (1.5%) had lens nucleus in the vitreous cavity, and 17 eyes (5.1%) had anterior vitrectomy.
Cataract Surgery Cost/effectiveness AnalysisThe cost/effectiveness of cataract surgery was 2 708 CNY in patients with LSES, and 8 663 CNY in standard cataract patients. Using the low cost/effectiveness in patients with LSES as standard, the incremental cost/effectiveness in standard cataract patients was 45 798.2 (Table 7).
Table 4Factors associated with postoperative low vision (uncorrected visual acuity <20/70)
aP<0.05;bThere is data loss of 3 preoperative UCVA.
DISCUSSION
Cataract remains the leading cause of blindness worldwide. It reduces visual function and affects patient’s daily life, study, and work. Global blindness among cataract will increase by 50% till 2020[5]. By contrast, China is still a developing country, the incidence of cataract is high, the coverage rate is uneven[6-7]and cataract surgery for prevention of blindness is more important. Especially with the increase of population in our country and the arrival of an aging society, the incidence of senile cataract blindness dramatically increases. Therefore it is important to prevent blindness in the elderly[8].
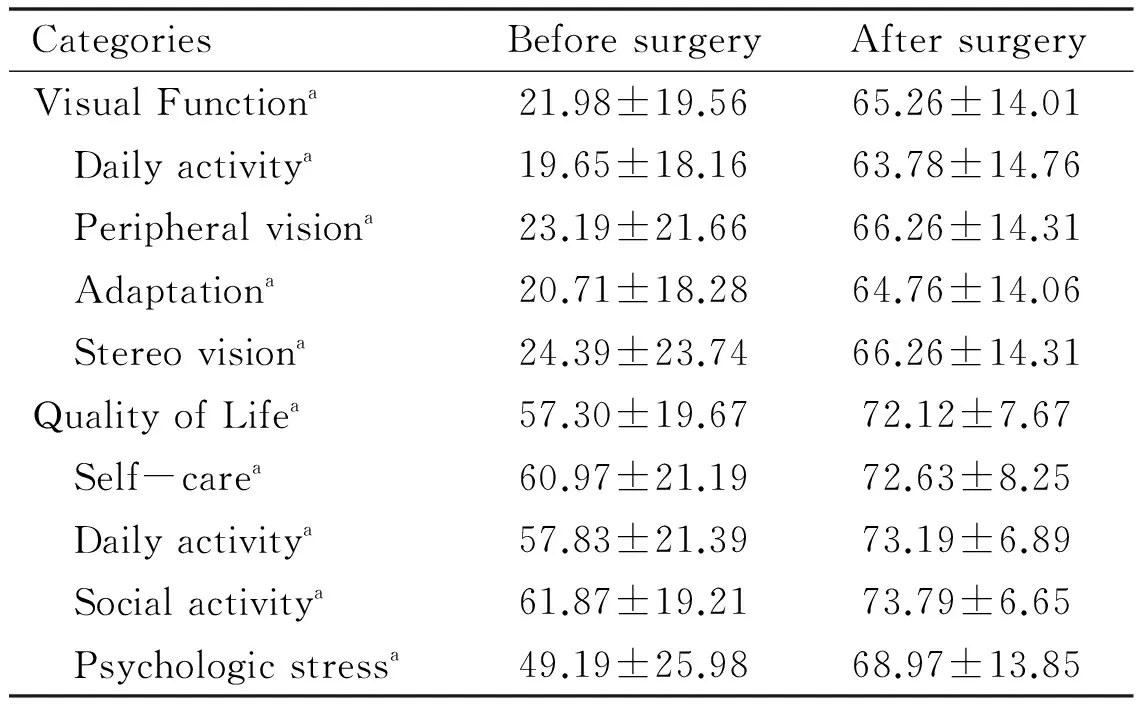
Table 5 Visual function and quality of life before and after surgery (n=83) (Mean±SD)
aP<0.05.
Surgery was the most effective treatment of cataract. Many studies showed that surgery significantly improved the visual quality and quality of life in patients with cataract. In this study, we evaluated the visual acuity, visual function, quality of life, and cost/effectiveness of the cataract surgery in patients with LSES who received government subsidies for free cataract surgery. Our results showed that visual acuity was significantly improved after the surgery, 70.4% of patients had UCVA of 20/40 or better 1wk after the surgery, and visual function and quality of life were significantly better postoperative, consistent with results from other studies[9-12].
In this study, we found that other ocular diseases and cataract classification were factors contributing to postoperative visual acuity. Preoperative poor vision and other ocular diseases were risk factors for postoperative low vision. Due to limited funding, cataract patients with LSES received standard spherical intraocular lenses, and some patients had residual myopia and astigmatism. Some of these patients with postoperative low vision may have improved vision with glasses. Unfortunately, refraction was not performed at 1wk postoperatively. Further study is desirable in this regard. A few patients had uveitis and iris synechiae postoperatively, and 7.5% of patients had posterior capsule opacification. Some of these patients had poor compliance with medication postoperatively and did not see a doctor on time, which may be the cause of low vision and poor quality of life. A better system for postoperative follow-up and patient education is desirable to reduce postoperative complications[13-14].
Studies showed that different surgical procedures and surgeries at different hospitals had different costs[15-16]. With lower surgical cost, higher percentage of patients may undergo the cataract surgery[17]. Our survey results demonstrated that the cost/effectiveness of cataract surgery in patients with LSES was lower than that in standard cataract patients. The surgical cost in patients with LSES was lower, the effectivenss was better, and postoperative visual acuity and quality of life were significantly improved.
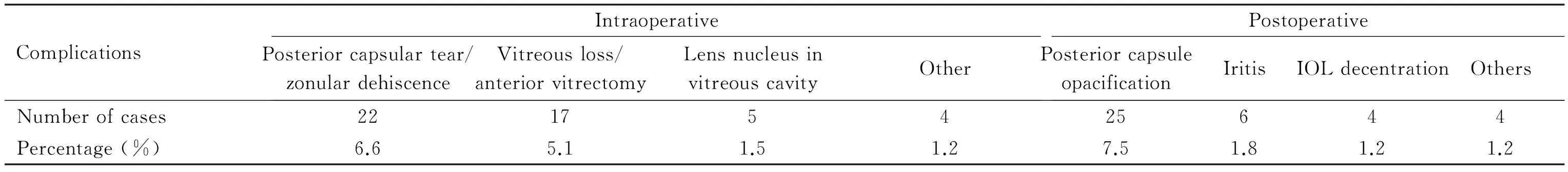
Table 6 Intraoperative and postoperative complications(n=334)
Table 7Cataract surgery cost/effectiveness analysis
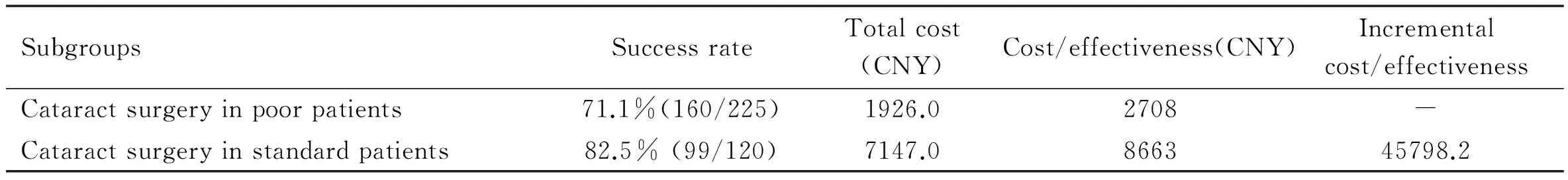
SubgroupsSuccessrateTotalcost(CNY)Cost/effectiveness(CNY)Incrementalcost/effectivenessCataractsurgeryinpoorpatients71.1%(160/225)1926.02708-Cataractsurgeryinstandardpatients82.5%(99/120)7147.0866345798.2
This study had certain limitations. We did not include a control group, and could not compare results, such as visual outcomes and improvements in quality of life, in patients with LSES and patients with standard cataract surgery. Our results were consistent with results from other studies[9-12]. The follow-up of 1wk was short, and manifest refraction and best-corrected visual acuity were not obtained at 1wk postoperatively. Some of the patients with postoperative low vision may have improved vision with glasses. Further studies with longer follow-up are warranted.
In summary, we have made good progress in the prevention of blindness. There are still some problems that need to be solved, such as the slow increase of cataract surgery procedures[18]. This study provides a helpful guide to blindness prevention. The Millions of Poor Cataract Patients’ Extraction Project provides affordable blindness prevention and treatment services for cataract patients[19-21], especially cataract patients with LSES, and explores the suitable, effective, convenient, sustainable, and low cost cataract health service system.
REFERENCES
1 Wood CM. Surgery for cataract.BMJ2007;334(7585):107
2 Zhang H, Dong K, Wang FF, Dai JL. Investigation and analysis of millions of poor cataract patients and engineering service ability of medical institutes of Shanxi Province.ChineseRemedies&Clinics2014;14(2):184-186
3 Fletcher A, Vijaykumar V, Selvaraj S, Thulasiraj RD, Ellwein LB. The Madurai Intraocular Lens Study.III: Visual functioning and quality of life outcomes.AmJOphthalmol1998;125(1):26-35
中國水利:剛剛過去的2011年是“十二五”的開局之年,是中央1號文件發布和中央水利工作會議召開之年,也是《太湖流域管理條例》的發布實施之年。請您談談《條例》頒布施行以來,太湖局作為太湖流域水資源綜合管理的國家派出機構,在圍繞中央1號文件精神、貫徹落實《條例》、推進流域水利工作方面開展了哪些工作?取得了怎樣的成效?
4 Fletcher AE, Ellwein LB, Selvaraj S, Vijaykumar V, Rahmathullah R, Thulasiraj RD. Measurements of vision function and quality of life in patients with cataracts in southern India. Report of instrument development.ArchOphthalmol1997;115(6):767-774
5 Congdon N, Vingerling JR, Klein BE, West S, Friedman DS, Kempen J, O’Colmain B, Wu SY, Taylor HR; Eye Diseases Prevalence Research Group. Prevalence of cataract and pseudophakia aphakia among adults in the United States.ArchOphthalmol2004;122(4):487-494
6 Yao K. The development direction and problems of the development of cataract in China.ChinJOphthalmol2015;51(4):241-244
7 Zhao JL. There is a long way to go about the prevention of the blindness in China.ChinJOphthalmol2012;48(3):193-195
8 Xia Q, Zhang W, Zhang YZ, Shi ZA, Chu DF. Analysis of the causes of blindness and low vision in the elderly.CHINESEJOURNALOFGERIATRICS2004;23(2):96-98
9 Yang H, Qi XY, Ge WZ.Situation analysis of cataract surgery in poverty-stricken region of Yixing in Jiangsu.IntEyeSci2014;14(5):934-936
11 Fan YC, Lei CT, Zhang XQ, Zhu XY, Ma P. Analysis of postoperative visual function of poverty-stricken cataract patients by blindness prevention surgery in Sichuan Province, China.IntEyeSci2008;8(4):736-738
12 Li QQ, Zhao HJ, Jiang HF, Wu ML, Zhao R, Wu XL. Investigation on the postoperative quality of life of cataract patients in Baoshan District, Shanghai.ShanghaiJournalofPreventiveMedicine2015;27(7):409-411
13 Zeng SH, Yang QM, Chen DC, Wu SH. Prevention and control of nosocomial infection from the large number of cataract surgery at Life-line Express.ChineseJournalofPracticalNursing2015;31(30):2290-2292
14 Chen J, Li AG, Guan DY, Zhang XL. Analysis of the efficacy of cataract surgeries by Macao Life line Express “Light”.ChineseJournalofOcularTraumaandOccupationalEyeDisease2015;37(4):292-294
15 Muralikrishnan R, Venkatesh RPrajna NV, Frick KD. Economic cost of cataract surgeryprocedures in an established eye care centre in Southern India.OphthalmicEpidemiol2004;11(5):369-380
16 Fang J, Wang X, Lin Z, Yan J, Yang Y, Li J. Variation of cataract surgerycosts in four different graded providers of China.BMCPublicHealth2010;10:543
17 Zhang XJ, Liang YB, Liu YP, Jhanji V, Musch DC, Peng Y, Zheng CR, Zhang HX, Chen P, Tang X, Lam DS. Implementation of a free cataract surgery program in rural China-a community-based randomized interventional study.Ophthalmology2013;120(2):260-265
18 Zhao JL. To improve the rate of cataract surgery is a pressing matter of the moment of prevention of blindness in China.NationalMedicalJournalofChina2013;93(47):3729-3730
19 Goldzweig CL, Mittman BS, Carter GM, Donyo T, Brook RH, Lee P, Mangione CM. Variations in cataract extraction rates in Medicare prepaid and fee-for-serviee settings.JAMA1997;277(22):1765-1768
20 Zhang H. Major challenges and goals in prevention blindness in rural Shanxi province.SHANXIMEDICALJOURNAL2006;35(4):315-316
21 Zhao JL. Promote general eye health and sustainable development of blindness prevention work in China.ChinJOphthalmol2014;50(3):161-163
Foundation item:Shanxi Soft Science Research (2012041060-02) 中國山西省軟科學研究(2012041060-02)
(作者單位:1030002 中國山西省太原市山西省眼科醫院;277030 美國得克薩斯洲休斯頓市貝勒醫科大學眼科系)
作者簡介:張紅,畢業于山西醫科大學,學士,二級主任醫師(兼職教授),研究方向:眼健康管理和醫院管理。
通訊作者:張紅.sxzhanghong@126.com
DOI:10.3980/j.issn.1672-5123.2016.8.01
關鍵詞:百萬貧困白內障患者復明工程;術后視力和視功能;生存質量分析
中國山西334例“百萬貧困白內障患者復明工程”手術效果分析
張紅1,王芳芳1,劉文潔1,戴江麗1,董魁1,龔元元1,王莉1,2
摘要
·Original article·