毛細血管滲漏指數在膿毒癥并ARDS早期診斷中的應用
梅華鮮 李永勝 陳正平 黃中會 劉鳳丹
?
·臨床研究論著·
毛細血管滲漏指數在膿毒癥并ARDS早期診斷中的應用
梅華鮮李永勝陳正平黃中會劉鳳丹
目的探討毛細血管滲漏指數(CLI)對于預測膿毒癥患者并發ARDS的臨床價值。方法回顧性分析ICU收治的膿毒癥患者288例,檢測患者入院時的CRP、血清白蛋白,并記錄其余各項生理及實驗室指標,根據是否并發ARDS分為ARDS組和非ARDS組,比較2組患者肺損傷預測評分(LIPS)、CLI有無差異,并行Logistic回歸分析確定預測膿毒癥患者并發ARDS的獨立危險因素,采用受試者工作特征(ROC)曲線下面積(AUC)法比較各指標對ARDS早期診斷的價值。結果ARDS組患者血乳酸、CRP、CLI、LIPS、APACHEⅡ評分及病死率均高于非ARDS組,白蛋白低于非ARDS組,差異具有統計學意義(P均<0.05)。多因素回歸分析顯示CLI、LIPS是預測膿毒癥患者并發ARDS的獨立危險因素。ROC曲線法分析顯示CLI、LIPS預測ARDS的價值較大。CLI的AUC為0.807(95%CI0.757~0.856),最佳截斷點4.99,此時敏感度為86.3%,特異度為63.4%;LIPS的AUC為0.823(95%CI0.775~0.870),最佳截斷值為5.25,此時敏感度91.1%,特異度58.5%。結論CLI更簡單易得,可以作為預測膿毒癥患者并發ARDS的較好指標。
膿毒癥;急性呼吸窘迫綜合癥;毛細血管滲漏指數; 預測指標
ARDS是臨床常見的急危重癥,其發病急,病情進展快,治療棘手,死亡率高[1-2]。膿毒癥是機體感染微生物后引起的失控性全身炎癥反應,是急性肺損傷(ALI)/ARDS的重要易感因素;肺臟是膿毒癥中最易受累的靶器官[3]。雖然ARDS的診療技術不斷進步,但其病死率并沒有明顯下降;因此對ARDS的提前預測及早期干預尤顯重要[4]。研究表明毛細血管滲漏指數(CLI)可以評估膿毒癥患者毛細血管的通透性大小,而ARDS的病理特征之一即為肺微血管通透性增高,CLI是否能夠成為預測膿毒癥患者并發ARDS的指標,值得進一步研究[5-7]。
對象與方法
一、研究對象
選取2014年1月至2016年4月我院ICU收治的膿毒癥患者288例,其中男168例、女120例,年齡18~98歲、中位年齡59歲。膿毒癥的診斷參照2012年《國際嚴重膿毒癥和膿毒癥休克指南》[8]。排除年齡<18歲,住院時間<48 h的病例。ARDS的診斷采用2011年柏林新標準[9]。CLI定義為CRP(mg/dl)與血清白蛋白(g/L)的比值×100[5]。肺損傷預測評分(LIPS)的賦值標準見表1。

表1 LIPS賦值標準
續表
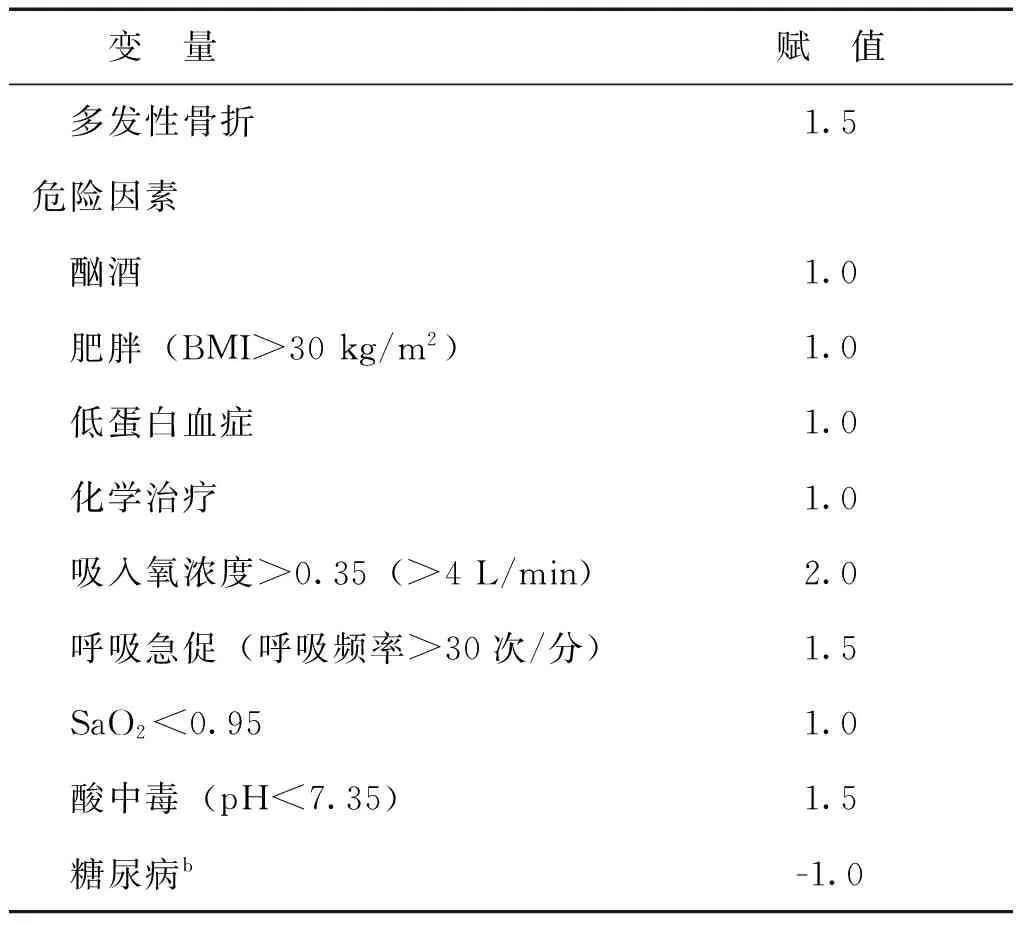
變 量賦 值 多發性骨折1.5危險因素 酗酒1.0 肥胖(BMI>30kg/m2)1.0 低蛋白血癥1.0 化學治療1.0 吸入氧濃度>0.35(>4L/min)2.0 呼吸急促(呼吸頻率>30次/分)1.5 SaO2<0.951.0 酸中毒(pH<7.35)1.5 糖尿病b-1.0
注:a若為急診手術增加1.5分;b僅在膿毒癥時計算
二、研究方法
對符合入選膿毒癥納入標準的患者,入院后均記錄其一般資料(性別 、年齡 、吸煙、飲酒史、基礎疾病)、生命體征指標、并常規送檢血常規、血生化、留取病原學標本并行相關培養。取入院24 h最差值行急性生理功能和慢性健康狀況評分系統Ⅱ(APACHEⅡ),入院當天行LIPS評分。根據是否合并ARDS分2組,ARDS組和非ARDS組。追蹤每例患者28 d的生存結局。
三、統計學處理

結 果
一、2組患者的臨床資料比較
2組患者的年齡、性別、基礎疾病、感染的部位相比,差異均無統計學意義(P均>0.05),具有可比性。ARDS患者的乳酸、CRP、CLI、LIPS、APACHEⅡ評分及病死率均高于非ARDS組,血清白蛋白水平低于非ARDS組,差異均具有統計學意義(P均<0.05),見表2。

表2 ARDS組與非ARDS組患者的臨床資料比較
二、膿毒癥并發ARDS的多因素回歸分析
選取2組間有統計學差異的乳酸、ALB、CRP、CLI、LIPS分別作為協變量,以膿毒癥并發ARDS作為因變量行Logistic回歸分析,結果顯示CLI、LIPS是預測膿毒癥患者并發ARDS的獨立危險因素,見表3。

表3 預測膿毒癥患者發生ARDS的Logistic回歸分析
三、CLI、LIPS預測膿毒癥并發ARDS的ROC曲線
將Logistic 回歸分析所得的各指標對各個體預測概率作為 ROC曲線協變量,以是否合并ARDS作為因變量,得到CLI的AUC為0.807(95%CI0.757~0.856),最佳截斷點4.99,此時敏感度為86.3%,特異度為63.4%;LIPS的AUC為0.823(95%CI0.775~0.870),最佳截斷值為5.25,此時敏感度91.1%,特異度58.5%。見圖1。

圖1 CLI、LIPS預測膿毒癥并發ARDS的ROC曲線
本研究回顧性分析我院ICU收入的288例膿毒癥患者的臨床資料,其中合并ARDS的患者124例,發病率為43.05%,略高于國外文獻報道的40%,考慮與納入的對象有關,危重患者發生ARDS的機率可能更高[10]。與非ARDS組相比,ARDS組患者的APACHEⅡ評分、死亡率更高。一項來自中國22個大型綜合醫院ICU的流行病學調查顯示,嚴重膿毒癥或膿毒性休克所致的ALI/ARDS是導致患者死亡的獨立危險因素,因而臨床醫師需提高對此類患者的重視[11]。
盡管目前ARDS的治療策略在不斷改進和更新,其病死率仍高達40%,究其根源是該疾病的發病機制尚未完全闡明,缺乏可以早期診斷的特異敏感指標及療效確切的治療措施[12-13]。如何提高ARDS的搶救成功率一直是臨床研究的熱點和難點。鑒于ARDS的治療手段有限,目前越來越多的學者認識到,早期診斷早期預防可能對ARDS的治療有著更為重要的意義[14]。
本研究對膿毒癥患者合并ARDS的危險因素行多因素回歸分析結果顯示,LIPS、CLI是膿毒癥患者并發ARDS的獨立預測因子。ROC曲線分析結果也顯示兩者具有較好的預測效能(AUC分別為0.823、0.807)。
LIPS評分是Gajic等[15]于2011年提出的用于預測患者發生ALI的模型。該系統從易感因素、高風險手術、創傷和風險修正等方面進行評分,認為評分越高越容易發生ARDS。該模型數據在患者入院早期即可獲得,與是否機械通氣無關,具有較好的操作性、可實踐性。經臨床檢驗,其具有較好的預測ALI的效力(文獻報道其AUC在 0.79~0.84),與本研究結果大致相仿[16-17]。
CLI是臨床上用于評估毛細血管通透性大小的指標。膿毒癥時,大量炎癥因子和炎癥介質的釋放和活化,導致全身多系統、失控性的毛細血管滲漏,血漿白蛋白等膠體物質也可從血管內滲出到組織間隙,一方面導致嚴重低蛋白血癥,血管內膠體滲透壓下降,另一方面組織間隙膠體滲透壓增加,更多的水分外滲,也加重了間質水腫程度[18]。肺通常是最早受累的器官,且發生率最高,臨床表現為ALI或ARDS[19]。因此,就其本質來說,ARDS是機體炎癥反應失控的結果,是SIRS的肺部表現。CLI由2部分組成,CRP是機體炎癥反應的敏感指標,而血漿白蛋白是維持血管內膠體滲透壓的主要成分,同時具有抗炎、抗氧化、抗休克、協調維持血管內皮完整性的作用[20-21]。CLI結合了兩者的優勢,同時反映全身的炎癥程度及血清白蛋白的水平,故可能成為預測ARDS的較好指標。
綜上所述,CLI是預測膿毒癥并發ARDS的較好指標。相比于LIPS 眾多的評判項目來說,CLI 更簡單易得,有著更好的操作性,值得臨床推廣應用。尤其對于急診、重癥醫學醫生來說,更有利于對病情作出快速準確的判斷,從而大大提高搶救的效率。
[1]Williams JP, Mcbride WH. After the bomb drops: a new look at radiation-induced multiple organ dysfunction syndrome(MODS). Int J Radiat Biol, 2011, 87(8): 851-868.
[2]Sirvent JM, Carmen de la Torre M, Lorencio C, Taché A, Ferri C, Garcia-Gil J, Torres A. Predictive factors of mortality in severe community-acquired pneumonia: a model with data on the first 24h of ICU admission. Med Intensiva, 2013, 37(5): 308-315.
[3]Barbas CS. Acute lung injury and acute respiratory distress syndrome: diagnostic hurdles. J Bras Pneumol, 2007, 33(4): xxv-xxvi.
[4]Festic E, Bansal V, Kor DJ, Gajic O; US Critical Illness and Injury Trials Group: Lung Injury Prevention Study Investigators (USCIITG-LIPS). SpO2/FiO2ratio on hospital admission is an indicator of early acute respiratory distress syndrome development among patients at risk. J Intensive Care Med, 2015, 30(4): 209-216.
[5]Cordemans C, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H, Huber W, Malbrain ML. Fluid management in critically ill patients: the role of extravascular lung water, abdominal hypertension, capillary leak, and fluid balance. Ann Intensive Care, 2012, 2(Suppl 1 Diagnosis and management of intra-abdominal hyperten): S1.
[6]Del Sorbo L, Slutsky A S. Acute respiratory distress syndrome and multiple organ failure. Curr Opin Crit Care, 2011, 17(1): 1-6.
[7]李永勝,冉曉,王進,占大錢,李樹生. 應用脈搏指示連續心排血量監測技術鑒別診斷重度ARDS一例. 新醫學, 2016, 47(1): 61-65.
[8]Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R; Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med, 2013, 41(2): 580-637.
[9]ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin Definition. JAMA, 2012, 307(23): 2526-2533.
[10]Iscimen R, Cartin-Ceba R, Yilmaz M, Khan H, Hubmayr RD, Afessa B, Gajic O. Risk factors for the development of acute lung injury in patients with septic shock: an observational cohort study. Crit Care Med, 2008, 36(5): 1518-1522.
[11]Zhou J, Qian C, Zhao M, Yu X, Kang Y, Ma X, Ai Y, Xu Y, Liu D, An Y, Wu D, Sun R, Li S, Hu Z, Cao X, Zhou F, Jiang L, Lin J, Mao E, Qin T, He Z, Zhou L, Du B; China Critical Care Clinical Trials Group. Epidemiology and outcome of severe sepsis and septic shock in intensive care units in mainland China. PLoS One, 2014, 9(9): e107181.
[12]Phua J, Badia JR, Adhikari NK, Friedrich JO, Fowler RA, Singh JM, Scales DC, Stather DR, Li A, Jones A, Gattas DJ, Hallett D, Tomlinson G, Stewart TE, Ferguson ND. Has mortality from acute respiratory distress syndrome decreased over time? A systematic review. Am J Respir Crit Care Med, 2009, 179(3): 220-227.
[13]Cross LJ, Matthay MA. Biomarkers in acute lung injury: insights into the pathogenesis of acute lung injury. Crit Care Clin, 2011, 27(2): 355-377.
[14]Litell JM, Gong MN, Talmor D, Gajic O. Acute lung injury: prevention may be the best medicine. Respir Care, 2011, 56(10): 1546-1554.
[15]Gajic O, Dabbagh O, Park PK, Adesanya A, Chang SY, Hou P, Anderson H 3rd, Hoth JJ, Mikkelsen ME, Gentile NT, Gong MN, Talmor D, Bajwa E, Watkins TR, Festic E, Yilmaz M, Iscimen R, Kaufman DA, Esper AM, Sadikot R, Douglas I, Sevransky J, Malinchoc M; U.S. Critical Illness and Injury Trials Group: Lung Injury Prevention Study Investigators(USCIITG-LIPS).Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med, 2011, 183(4): 462-470.
[16]Bauman ZM, Gassner MY, Coughlin MA, Mahan M, Watras J. Lung injury prediction score is useful in predicting acute respiratory distress syndrome and mortality in surgical critical care patients. Crit Care Res Pract, 2015, 2015: 157408.
[17]Trillo-Alvarez C, Cartin-Ceba R, Kor DJ, Kojicic M, Kashyap R, Thakur S, Thakur L, Herasevich V, Malinchoc M, Gajic O. Acute lung injury prediction score: derivation and validation in a population-based sample. Eur Respir J, 2011, 37(3): 604-609.
[18]Lesur I, Textoris J, Loriod B, Courbon C, Garcia S, Leone M, Nguyen C. Gene expression profiles characterize inflammation stages in the acute lung injury in mice. PLoS One, 2010, 5(7): e11485.
[19]Piantadosi CA, Schwartz DA. The acute respiratory distress syndrome. Ann Intern Med, 2004, 141(6): 460-470.
[20]McWilliam S, Riordan A. How to use C reactive protein: postscript. Arch Dis Child Educ Pract Ed, 2010, 95(6): 194-195.
[21]李建紅,柴艷芬,曹超. 血清白蛋白聯合急診膿毒癥死亡風險評分對膿毒癥患者預后價值的研究. 中華臨床醫師雜志, 2016, 10(8): 1128-1132.
(本文編輯:楊江瑜)
Application of CLI in the early diagnosis of sepsis complicated with ARDS
MeiHuaxian,LiYongsheng,ChenZhengping,HuangZhonghui,LiuFengdan.
TongjiHospitalAffiliatedtoTongjiMedicalUniversity,HuazhongUniversityofScienceandTechnology,Wuhan430030,China
,LiYongsheng,E-mail:ysli@tjh.tjmu.edu.cn
ObjectiveTo explore the clinical value of capillary leakage index (CLI) in the prediction of sepsis complicated with acute respiratory distress syndrome (ARDS). MethodsClinical data of 288 sepsis patients admitted in the intensive care unit (ICU) of our hospital were retrospectively analyzed. Serum C-reactive protein (CRP), albumin and other psychological and laboratory indexes were collected upon admission. All patients were divided into the ARDS and non-ARDS groups. The lung injury prediction score (LIPS) and CLI were statistically compared between two groups. Logistic regression analysis was used to determine the independent risk factors for sepsis complicated with ARDS. Clinical values of each index in the early diagnosis of ARDS were evaluated with the areas under the receiver operating characteristics (ROC) curve (AUC). ResultsCompared with the non-ARDS group, the lactate level, CRP level, CLI, LIPS, APACHEII score and mortality were significantly higher whereas the albumin level was considerably lower in the ARDS group (allP<0.05). Multi-variate logistic regression revealed that CLI and LIPS were the independent risk factors of sepsis complicated with ARDS. ROC curve analysis demonstrated that the values of CLI and LIPS in predicting ARDS occurrence were relatively significant. The AUC of CLI was 0.807 (95%CI0.757- 0.856). The optimal cut-off value was 4.99 with sensitivity of 86.3% and specificity of 63.4%. The AUC of LIPS was 0.823 (95%CI0.775- 0.870). The optimal cut-off value was 5.25 with sensitivity of 91.1% and specificity of 58.5%. ConclusionsCLI is a simple and convenient index, which can be utilized to predict the incidence of sepsis complicated with ARDS.
Sepsis; Acute respiratory distress syndrome; Capillary leakage index; Predictor
10.3969/j.issn.0253-9802.2016.10.007
430030 武漢,華中科技大學同濟醫學院附屬同濟醫院急診/重癥醫學科
,李永勝, E-mail:ysli@tjh.tjmu.edu.cn
2016-06-06)