Aldynoglia cells and modulation of RhoGTPase activity as useful tools for spinal cord injury repair
Ernesto Doncel-Pérez , Manuel Nieto-Sampedro
1 Grupo de Química Neuro-Regenerativa, Hospital Nacional de Parapléjicos, Servicio de Salud de Castilla La Mancha (SESCAM), Toledo, Spain
2 Grupo de Plasticidad Neural, Instituto Cajal, CSIC, Madrid, Spain
Aldynoglia cells and modulation of RhoGTPase activity as useful tools for spinal cord injury repair
Ernesto Doncel-Pérez1,*, Manuel Nieto-Sampedro2,*
1 Grupo de Química Neuro-Regenerativa, Hospital Nacional de Parapléjicos, Servicio de Salud de Castilla La Mancha (SESCAM), Toledo, Spain
2 Grupo de Plasticidad Neural, Instituto Cajal, CSIC, Madrid, Spain
A combined approach in spinal cord injury (SCI) therapy is the modulation of the cellular and molecular processes involved in glial scarring. Aldaynoglial cells are neural cell precursors with a high capacity to differentiate into neurons, promote axonal growth, wrapping and myelination of resident neurons. These important characteristics of aldaynoglia can be combined with specific inhibition of the RhoGTPase activity in astroglia and microglia that cause reduction of glial proliferation, retraction of glial cell processes and myelin production by oligodendrocytes. Previously we used experimental central nervous system (CNS) injury models, like spinal cord contusion and striatal lacunar infarction and observed that administration of RhoGTPase glycolipid inhibitor or aldaynoglial cells, respectively, produced a significant gain of functional recovery in treated animals. The combined therapy with neuro-regenerative properties strategy is highly desirable to treat SCI for functional potentiation of neurons and oligodendrocytes, resulting in better locomotor recovery. Here we suggest that treatment of spinal lesions with aldaynoglia from neurospheres plus local administration of a RhoGTPase inhibitor could have an additive effect and promote recovery from SCI.
*Correspondence to: Ernesto Doncel-Pérez, Ph.D., ernestod@sescam.jccm.es or Manuel Nieto-Sampedro, Ph.D., mnietosampedro@gmail.com.
orcid: 0000-0002-2704-9782 (Ernesto Doncel-Pérez)
glial scar; astrocyte; microglia; neurospheres; aldaynoglia; axonal growth; myelination; glycoside inhibitor
Following heart and cancer diseases, accidental trauma is the leading cause of death for children and young adults in developed countries. Central nervous system (CNS) lesions cause working incapacity and chronic disability and often occur in individuals below the age of 45 years. Although the outcome of brain or spinal cord injuries depends on the damaged area and the extent of the injury, currently available therapies that can only provide symptoms relief and rehabilitation.
After spinal cord injury (SCI), a dynamic series of cellular and molecular events take place in the affected zone. While blood phagocytes remove cellular debris and secondary neuronal death progresses, neural stem cells migrate near the damaged zone, proliferate and differentiate to astrocytes that enlarge their fibrous processes, forming a glial boundary between the injured area and the uninjured CNS. Fibroblasts from adjacent connective tissue divide and overlay the fibrous astrocytes, depositing collagen, thus completing the formation of the new CNS boundary, called the glial scar, where cells of the scar, mainly reactive astrocytes, reactive microglia, pericytes, fibroblasts and extracellular matrix, make the glial scar a hostile environment for axonal growth. Astrocytes and microglia represent highly reactive CNS cell populations and their principal role in glia scarring has been well documented elsewhere.
The astrocyte response to CNS injury is also characterized by the production of chondroitin sulfate proteoglycans (CSPGs), which present a potent barrier to axon regeneration. The inhibitory action of CSPGs has been attributed to the abundance of negatively charged glycosaminoglycan (GAG) chains that decorate the protein core, which are thought to act as a poor substrate and electrostatically repel growth cones. Protein tyrosine phosphatase sigma (PTPsigma), leukocyte common antigen related phosphatase (LAR) and Nogo receptor (NgR) have been identified as neuronal receptors that functionally interact with and mediate CSPG-dependent inhibition of neuronal growth. Chondroitinase ABC (chABC), a bacterial enzyme that digests the GAG chains, abolishes CSPG-dependent neurite outgrowth inhibition in vitro and improves neurite outgrowth and functional recovery after SCI. Therefore pharmacological targeting of CSPG receptors is a strategy to relieve CSPG-dependent capture of growth cones that has shown some potential. While these studies have identified CSPG receptors as possible targets, future work should focus on developing small molecule inhibitors to achieve better CNS penetration and distribution for earlier and more efficient targeting after injury (Kaplan et al., 2015). In this sense, we consider the design and synthesis of glycoside inhibitors to achieve specific and temporal inhibition of astroglia. This, in turn, would permit a significant reduction of CSPGs production, promote axonal growth and functional recovery of neurons and glial cells (Doncel-Perez et al., 2013; Garcia-Alvarez et al., 2015).

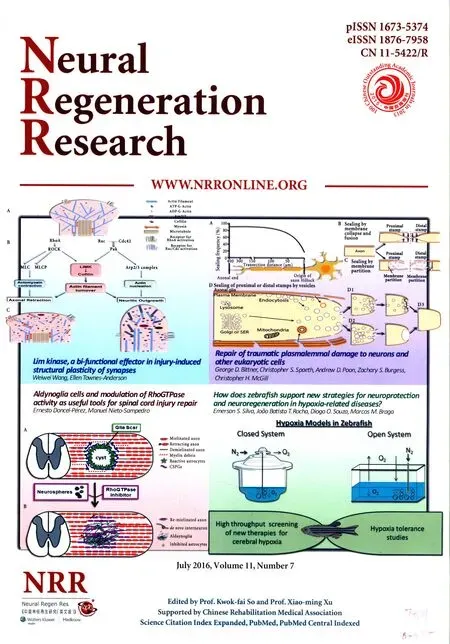
Figure 1 A SCI repair model subjected to treatment with aldynoglia, derived from neurosphere cells, and RhoGTPase inhibition.
CNS myelin derivatives constitute a barrier to axon regeneration at sites of injury. The different types of CNS neurons possess very different regenerative capacities, and specific mechanisms for myelin inhibition related to neuron-type must be considered. But in general, myelin-associated inhibitors (MAIs) including Nogo, myelin-associated glycoprotein (MAG) and oligodendrocyte myelin glycoprotein (OMgp) collapse axonal growth cones and inhibit growth. Targeting these external inhibitory factors has led to some improvements in axonal plasticity and functional recovery after CNS injury. In addition, stimulating intrinsic growth potential by neuronal knockout of negative regulators of growth, including phosphatase and tensin homolog (PTEN) and suppressor of cytokine signaling 3 (SOCS3), can induce striking long-distance axon regeneration after CNS injury (Sun et al., 2011). Furthermore, engraftment of neural stem cells into transected rodent spinal cords can result in impressive long-distance growth of grafted cells (Lu et al., 2012). These studies indicate that an increased intrinsic neuronal growth potential is able to overcome the inhibitory nature of the injured CNS.
The actin-regulating small GTPase RhoA and downstream effector Rho kinase (ROCK), are extensively studied mediators of neurite outgrowth inhibition in the CNS. MAIs have been shown to increase the levels of active GTP-bound RhoA. Inhibition of ROCK, stimulates neurite outgrowth on myelin and infusion of small molecule ROCK inhibitors Y-27632 or fasudil into the injured rat spinal cord improves locomotor recovery. RhoA can be specifically inhibited with Clostridium botulinum exoenzyme C3 transferase, which ADP-ribosylates and inactivates RhoA. Treatment of animals with C3 improves locomotor recovery in contusion and dorsal hemisection injury models. The positive outcomes with C3 have translated into a phase I/II clinical trial with Cethrin (BA-210), a cell-permeable form of C3 that is delivered locally over the dura mater in a fibrin sealant during spinal surgery (Lord-Fontaine et al., 2008; Kaplan et al., 2015).
The ability of implanted neural stem cells (NSCs) to survive and functionally integrate into injured host spinal cord in rodents, also suggests that the inhibitory nature of the injured CNS can be overcome by neurons with vigorous growth capacity. NSCs have been shown to extend long axons throughout the grey and white matter of transected host spinal cords, establishing an electrophysiological bridge across the injury (Lu et al., 2012). Grafted NSCs had the ability to integrate into the host spinal cords, but it was also noted the presence of ectopic colonies of donor cells throughout the spinal cord and brain stem in half of the animals (Steward et al., 2014). This highlights the caution that must be exercised in the development of NSC therapies, as implanted cells may give rise to tumors, and exuberant synaptic connections could result in unfavorable behavioral and sensory side effects, including neuropathic pain. Anyway, the experiments provided proof that neurons from NSCs with high growth capacity were capable of extensive growth in the injured CNS, in spite of the presence of inhibitory factors.
An approach in SCI therapy is the modulation of cellular and molecular process involved in glial scarring. It contains two main elements: i) supporting, preserving and promoting axonal growth of resident and new neurons, and ii) inhibiting glial activation and glial scar formation (Figure 1).
Regarding the first process we obtained aldynoglia, which are growth-promoting glial cells existing in olfactory bulb, hypothalamus, hypophysis and pineal gland, that share with Schwann cells (SCs) the ability to survive and proliferate in culture, to promote neurite outgrowth, and to ensheath and myelinate neurites. The cells typical of these CNS loci, olfactory ensheathing cells (OECs), tanycytes, pituicytes, and pineal interstitial cells, may be identified in culture by their concomitantly expressing a set immunological markers, namely peripheral GFAP, vimentin, p75 NGF receptor, and type α estrogen receptor, showing a mixture of SC-like and astrocyte-like properties. Transplants of aldynoglia have considerable potential for the treatment of CNS injuries. Multipotent NSCs can be isolated from various mammalian CNS regions at different stages of development and cultured as floating neurospheres. Given the appropriate signals, neurosphere cells can differentiate in vitro to neurons, astrocytes, and oligodendrocytes, although their behavior when transplanted is more variable. Rodent neurospheres when transplanted differentiated predominantly to glia, whereas grafts of human embryonic forebrain neurospheres also gave rise to a significant proportion of neurons. We reported that mesencephalic rodent neurospheres differentiated in vitro predominantly to cells with properties similar to aldynoglia, when exposed to OEC-conditioned medium (OEC-CM), This contains a mixture of neurotrophins (NGF, BDNF) and neuregulins, apparently capable of instructing neurospheres to develop into neural progenitors with aldynoglia phenotype. The OEC-CM caused neurosphere cells to differentiate to cells with peripheral glia phenotype, as judged by their expression of mRNA and protein markers (GFAP, vimentin, nestin, and S100 proteins). Neurosphere cells, when co-cultured with dorsal root ganglia (DRG), migrated towards the ganglia, invaded them and contacted DRG neurons. Direct aldaynoglia-neuron interaction was necessary and sufficient to promote neurite outgrowth, ensheathment, and myelination (Doncel-Perez et al., 2009). The possibility of differentiating neurosphere cells to aldynoglia could satisfy the necessity of the great amount of cells in cell transplants required to repair large CNS injuries.
To cover the second process, we tried to inhibit glial cells in a specific manner, while avoiding to affect other neural cell types, i.e., neurons and oligodendrocytes. Over the last years, based on the chemical structure of a natural inhibitor of astroblast and astrocytoma division (neurostatin), we analyzed glycosides as inhibitors of glioma division. Among the compounds tested, sulphated glycolipids presented the highest inhibitory activity for human and rat glioma division. Interestingly, the use of DNA microarray technology revealed that the ARHGDIA gene was repressed. The product of this gene is Rho guanine nucleotide dissociation inhibitor alpha (RhoGDIα), a regulator of RhoGTPases (Doncel-Perez et al., 2013; Garcia-Alvarez et al., 2015). We showed recently that the sulfoglycolypid affected glial cells by interacting with the RhoGDIα protein, causing an increase in the expression of TrkB genes in neural cells, myelin production by oligodendrocytes and promoting axonal growth from DRG neurons. The astroglial cells changed their morphology and this was mainly transduced by the BDNF/TrkBT1/RhoGDIα pathway, which is also operative in microglia. The TrkT1 isoform corresponds to the TrkB truncated form of the receptor with a short cytoplasmic domain of 11 amino acid residues in the C-terminus. This domain interacts with RhoGDIα inducing influx of Ca2+and morphological change in glia cells. The inhibition of the pathway BDNF/TrkB/RhoGDIα in astrocytes and microglial cells, by sequestering RhoGDIα, was proposed as a new target for SCI therapy (Garcia-Alvarez et al., 2015).
Above we mentioned that grafted NSCs could integrate into host spinal cords and brain, but implanted cells may give rise to tumors and neuropathic pain. Here we propose that a combination of NSCs and antiproliferative glycoside could save this obstacle (Figure 1). The antiproliferative properties of the compound diminished the risk of tumor growth (Doncel-Perez et al., 2013) and could facilitate the movement of transplanted NSCs in a less rigid environment by glial laxity.
The axonal growth promotion by aldaynoglia and the inhibition of RhoGTPase activity in glia cells occurred simultaneously. The presence of sulfoglycolipid potentiated the axon outgrowth induced in DRG neurons, and aldynoglial cells were not affected by the glycoside. This indicates that the inhibition of the activity was due to the anti-proliferative effect of the glycoside and did not affect other functions in aldaynoglia. The astrocyte recruitment after injury relies on proliferation and the number of astrocytes recruited to a CNS lesion site is significantly reduced in RhoGTPase deficient mice. In other scenarios, high RhoGTPase activity in aged hematopoietic stem cells (HSC) was causally linked to HSC aging and correlated with a loss of polarity in aged HSCs, and pharmacological inhibition of RhoGTPase Cdc42 activity functionally rejuvenated aged HSCs, increased the proportion of polarized cells in aged HSC population, and restored the level and spatial distribution of histone acetylation to a status similar to that seen in young HSCs (Florian et al., 2012).
Aldaynoglia cells are neural cell precursors with capacity to differentiate to neurons, promote axonal growth, wrapping and myelination. The selective inhibition of RhoGTPase activity in astroglia and microglia by sulfoglicolipid reduced their cell proliferation, induced retraction of glial cell processes and increased myelin production by oligodendrocytes (Doncel-Perez et al., 2009; Muneton-Gomez et al., 2012; Garcia-Alvarez et al., 2015). These properties are desired for SCI therapy where functional potentiation of neurons and oligodendrocytes results in a better motor recovery. Rats with a moderate spinal cord contusion, treated with spinal injection of sulfoglicolipid, showed a significative recovery (Garcia-Alvarez et al., 2015), which was also seen in a rat model of striatal lacunar infarction, where new neurons derived from aldaynoglia integrated into the CNS host circuitry and establishing synaptic contacts (Muneton-Gomez et al., 2012). These data support the use of aldaynoglia and RhoGTPase inhibitors as useful tools for therapy in CNS trauma, particularly in the SCI treatment.
Author contributions: EDP wrote the draft of manuscript and composed the figure. MNS did revision and editing of the manuscript. The authors agree with the final version of this manuscript for publication.
Conflicts of interest: None declared.
Doncel-Perez E, Caballero-Chacon S, Nieto-Sampedro M (2009) Neurosphere cell differentiation to aldynoglia promoted by olfactory ensheathing cell conditioned medium. Glia 57:1393-1409.
Doncel-Perez E, Garcia-Alvarez I, Fernandez-Mayoralas A, Nieto-Sampedro M (2013) Synthetic glycolipids for glioma growth inhibition developed from neurostatin and NF115 compound. Bioorg Med Chem Lett 23:435-439.
Florian MC, Dorr K, Niebel A, Daria D, Schrezenmeier H, Rojewski M, Filippi MD, Hasenberg A, Gunzer M, Scharffetter-Kochanek K, Zheng Y, Geiger H (2012) Cdc42 activity regulates hematopoietic stem cell aging and rejuvenation. Cell Stem Cell 10:520-530.
Garcia-Alvarez I, Fernandez-Mayoralas A, Moreno-Lillo S, Sanchez-Sierra M, Nieto-Sampedro M, Doncel-Perez E (2015) Inhibition of glial proliferation, promotion of axonal growth and myelin production by synthetic glycolipid: A new approach for spinal cord injury treatment. Restor Neurol Neurosci 33:895-910.
Kaplan A, Ong Tone S, Fournier AE (2015) Extrinsic and intrinsic regulation of axon regeneration at a crossroads. Front Mol Neurosci 8:27.
Lord-Fontaine S, Yang F, Diep Q, Dergham P, Munzer S, Tremblay P, McKerracher L (2008) Local inhibition of Rho signaling by cell-permeable recombinant protein BA-210 prevents secondary damage and promotes functional recovery following acute spinal cord injury. J Neurotrauma 25:1309-1322.
Lu P, Wang Y, Graham L, McHale K, Gao M, Wu D, Brock J, Blesch A, Rosenzweig ES, Havton LA, Zheng B, Conner JM, Marsala M, Tuszynski MH (2012) Long-distance growth and connectivity of neural stem cells after severe spinal cord injury. Cell 150:1264-1273.
Muneton-Gomez VC, Doncel-Perez E, Fernandez AP, Serrano J, Pozo-Rodrigalvarez A, Vellosillo-Huerta L, Taylor JS, Cardona-Gomez GP, Nieto-Sampedro M, Martinez-Murillo R (2012) Neural differentiation of transplanted neural stem cells in a rat model of striatal lacunar infarction: light and electron microscopic observations. Front Cell Neurosci 6:30.
Steward O, Sharp KG, Matsudaira Yee K (2014) Long-distance migration and colonization of transplanted neural stem cells. Cell 156:385-387.
Sun F, Park KK, Belin S, Wang D, Lu T, Chen G, Zhang K, Yeung C, Feng G, Yankner BA, He Z (2011) Sustained axon regeneration induced by co-deletion of PTEN and SOCS3. Nature 480:372-375.
How to cite this article: Doncel-Pérez E, Nieto-Sampedro M (2016) Aldynoglia cells and modulation of RhoGTPase activity as useful tools for spinal cord injury repair. Neural Regen Res 11(7)∶1043-1045.
10.4103/1673-5374.187020
2016-06-30
INVITED REVIEW
- 中國神經(jīng)再生研究(英文版)的其它文章
- Recovery of an injured corticospinal tract by subcortical peri-lesional reorganization in a patient with intracerebral hemorrhage
- Dose response and time course of manganeseenhanced magnetic resonance imaging for visual pathway tracing in vivo
- Low-power laser therapy for carpal tunnel syndrome: effective optical power
- Extracellular matrix from human umbilical cordderived mesenchymal stem cells as a scaffold for peripheral nerve regeneration
- Differential temporal expression of matrix metalloproteinases following sciatic nerve crush
- Protective effects of ginsenoside Rg1 against hydrogen peroxide-induced injury in human neuroblastoma cells