Clinical investigation of speech signal features among patients with schizophrenia
Jing ZHANG, Zhongde PAN, Chao GUI, Jie ZHU,*, Donghong CUI,*
Clinical investigation of speech signal features among patients with schizophrenia
Jing ZHANG1,2, Zhongde PAN1,3,4, Chao GUI5, Jie ZHU5,*, Donghong CUI1,3,4,*
schizophrenia; speech; speech signal features; biomarkers; negative symptoms; China
1. Introduction
Schizophrenia is a complex mental disorder caused by multiple factors including heredity, development,and environment.[1]The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)[2]lists the following five prominent psychopathological characteristics of the disorder: delusions, hallucinations,disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms. Negative symptoms include emotional blunting, poverty of speech, avolition,an inability to experience pleasure, and the lack of desire to form relationships. Present methods for determining the diagnosis and for assessing the effectiveness of treatment primarily rely on the subjective judgment of the clinician who uses information provided by family members, the mental status examination, and various clinical symptom scales. In the absence of objective measures and the frequent uncooperativeness of patients – particularly those with prominent negative symptoms – assessing the severity and course of the illness is often challenging for clinicians. To address this fundamental problem, psychiatric researchers are actively searching for objective biomarkers that can be used both in the diagnosis of the condition and in the monitoring of the clinical progress of the disorder.
Fluctuations in speech that parallel patients'physio-psychological state might be suitable candidates as biomarkers for schizophrenia. Studies of signal processing and artificial intelligence find that the features of speech signals can contain substantial emotional information.[3,4]Changes of emotions and the range and variability of emotions can be quantified by changes in speech parameters, particularly by changes in prosody– that is, the vocal pitch (fundamental frequency),loudness (acoustic intensity), and rhythm (phoneme and syllable duration) of speech. For example, when a person is in an angry state, changes in physiological characteristics (e.g., increased heart rate, elevated skin voltage, and elevated blood pressure) are often associated with changes in the rate, volume, and tone of speech.
There is considerable interest in developing methods for extracting the acoustic parameters which ref l ect emotions from speech samples and in assessing the relationship of these parameters to emotionally restrictive states, such as the negative symptoms of schizophrenia. Identification of the emotional content of speech signals is primarily accomplished by two processes: first, the features of the speech signals are extracted from speech samples and then judgments are made about the emotional content of the identified features based on pre-existing models. The quality of the extraction process largely determines the functional quality of the speech identification system.[5,6]Studies about speech identification generally start by investigating the prosodic features and acoustic characteristics of speech content, focusing on the features which are directly relevant to the emotional characteristics of speech.[7]
Patients with schizophrenia who have prominent negative symptoms such as emotional blunting and poverty of speech may be particularly prone to having restricted emotional content in their speech content.This can directly limit their social functioning and make it difficult for clinicians to detect changes in their clinical status over the course of their illness. Identification of the specific speech abnormalities in such patients could both help in monitoring the course of the illness and potentially be used to develop targeted interventions for patients with prominent negative symptoms.Several researchers[8-11]have reported relationships between specific phonetic parameters and the negative symptoms and impaired emotional perception of schizophrenia, but the results to date are far from robust.
The current study assessed the characteristics of the speech signals of patients with schizophrenia with prominent negative symptoms, considered the association between these features and the severity of different types of negative symptoms, and compared the speech signal features in these patients with those in healthy control subjects.
2. Methods
2.1 Participants
The patient group consisted of patients with schizophrenia who were inpatients at the Shanghai Mental Health Center from September 2013 to December 2015. The inclusion criteria were as follows:(a) aged from 18 to 65 years; (b) met the diagnostic criteria of schizophrenia specified in DSM-5[2]as assessed by a psychiatrist using the Mini-International Neuropsychiatric Interview (M.I.N.I. 6.0).[12](c) had prominent negative symptoms of schizophrenia; (d)a minimum of duration of illness of two years; (e) no co-morbid psychiatric or substance abuse disorder;(f) no evidence of severe impulsivity; (g) not using antipsychotic medication that could impair speech; and(h) both the patient and the patient’s family member provided written informed consent to participate in the study, including the use of smartphones to record speech.
We recruited volunteers from the community by advertisement as healthy controls. Volunteers were similar for patients in age and duration of education,underwent a through psychiatric exam (using the M.I.N.I. 6.0) and physical exam. Inclusion criteria for controls were as follows (a) 18 to 65 years of age; (b)Han Chinese ethnicity; (c) no current or past physiopsychological, substance abuse, or serious neurological disorder; (d) no serious physical illness; (e) no history of severe impulsivity; (f) no history of suicide attempt;(g) not using antipsychotic medication that could affect speech; (h) no family history of psychiatric disorder or serious neurological disorder; and (i) provided written informed consent to participate in the study.
2.2 Measures
We explored a smartphone APP which could record the participant’s outgoing speech (i.e., no incoming speech is captured or recorded). Each participant was provided with a preloaded Samsung GALAXY Mega 6.3 (a sampling frequency of 44 kHz and a resolution of 32 bit). Participants (both patients and controls) sat comfortably in a noise-controlled room (background sound below 30 dB) and were asked to use the specially designed smartphone to call a psychiatrist from the study and speak naturally for 15 minutes about any topic of interest.
All call samples were saved in the Advanced Audio Coding (aac) formant. After pre-processing of the data, speech features of interest were extracted and analyzed at the School of Electronic Information and Electrical Engineering of Shanghai Jiao Tong University.We extracted speech features with high emotional identification rates that were identified in previous reports of speech models of bipolar disorder[13,14]and from our own speech model for schizophrenia generated from data in the current study. These parameters include prosodic features (formant 1 to 6 [F1 to F6, unit: Hz], formant bandwidth [unit: Hz], formant amplitude [unit: dB]), and two spectral features (the linear prediction coding [LPC], and the Mel-frequency cepstral coefficient [MFCC]). To assess the stability of the speech data extracted by the software, participants in the patient group repeated the phone call 1 week after the baseline assessment.
In addition, trained attending psychiatrists administered the Positive and Negative Syndrome Scale(PANSS)[15], the Scale for the Assessment of Negative Symptoms (SANS),[16]and the Clinical Global Impression-Schizophrenia Scale (CGI-S)[17]to the participating patients at baseline and 1 week after baseline.
2.3 Statistical analysis
All data were processed and analyzed using SPSS 17.0 software. The in-group comparisons from baseline to 1-week post-baseline were analyzed by paired t-tests.The test-retest reliability of the acoustic parameters was assessed by comparing the baseline and 1-week results using intraclass correlation coefficients (ICCs).For between-group comparisons, continuous data with normal distributions were analyzed using independent t-tests; non-normal continuous variables were analyzed using Mann-Whitney U tests; and nominal data were analyzed using Chi-square tests. In the patient group, we use Pearson correlation analyses to assess the strength of the relationship between the acoustic parameters and the severity of clinical symptoms. All statistical analyses used two-tailed tests and statistical significance was set at p<0.05.
3. Results
As shown in Figure 1, 26 patients completed the two assessments. These patients included 16 males (61.5%);their mean (sd) age was 43.3 (10.9) years; their mean years of education was 9.5 (3.0) years; the mean course of their illness was 21.7 (8.5) years; the mean number of psychiatric admissions was 3.4 (2.4) admissions; and the mean total length of hospitalization was 7.0 (5.4)years. A total of 30 control subjects completed the phonetic assessment; they included 16 males (53.3%),had a mean (sd) age of 37.0 (14.3) years and had a mean duration of education of 11.6 (2.5) years.Comparison between the 26 patients who completed the assessment and the 30 controls who completed the assessment found no statistically significant differences by gender (X2=0.38, p=0.536), by age (t=1.70, p=0.098),or by duration of education (t=1.95, p=0.058).
As shown in Table 1, in the patient group there were no statistically significant differences between the baseline and 1-week assessment of CGI-S, PANSS total and subscale scores, and SANS total and subscale scores. Thus the patients’ clinical status was stable over the 1-week interval.
Table 2 shows the baseline and 1-week results for the acoustic parameters in the patient group and the baseline acoustic parameters in the control group. The test-retest reliability of these measures (only assessed in the patient group) was good, with ICC values ranging from 0.55 to 0.88. The prosody features and formant amplitude and bandwidth were not significantly different between patients and controls at baseline,but the two spectral features were different between the groups: MFCC was significantly lower in the patient group than in the control group and the LPC was significantly higher in the patient group than in the control group.
Table 3 shows the correlation of 17 clinical and demographic measures with the 10 acoustic parameters in the 26 patients. Among the 170 associations considered, ten coefficients were >0.40 and, thus,statistically significant at the p<0.05 level: Formant 1 was negatively correlated with the SANS alogia subscale score, Format 2 was negatively correlated with the PANSS negative symptoms subscale score and the SANS alogia subscale score; Formant 6 was significantly more prominent in male than female respondents; bandwidth was negatively correlated with the SANS affective blunting subscale score and stronger in female respondents than in male respondents;and MFCC was positively correlated with the PANSS general psychopathology subscale score and with the patients’ total number of hospitalizations, and it was more prominent in male respondents than female respondents.
4. Discussion
4.1 Main findings
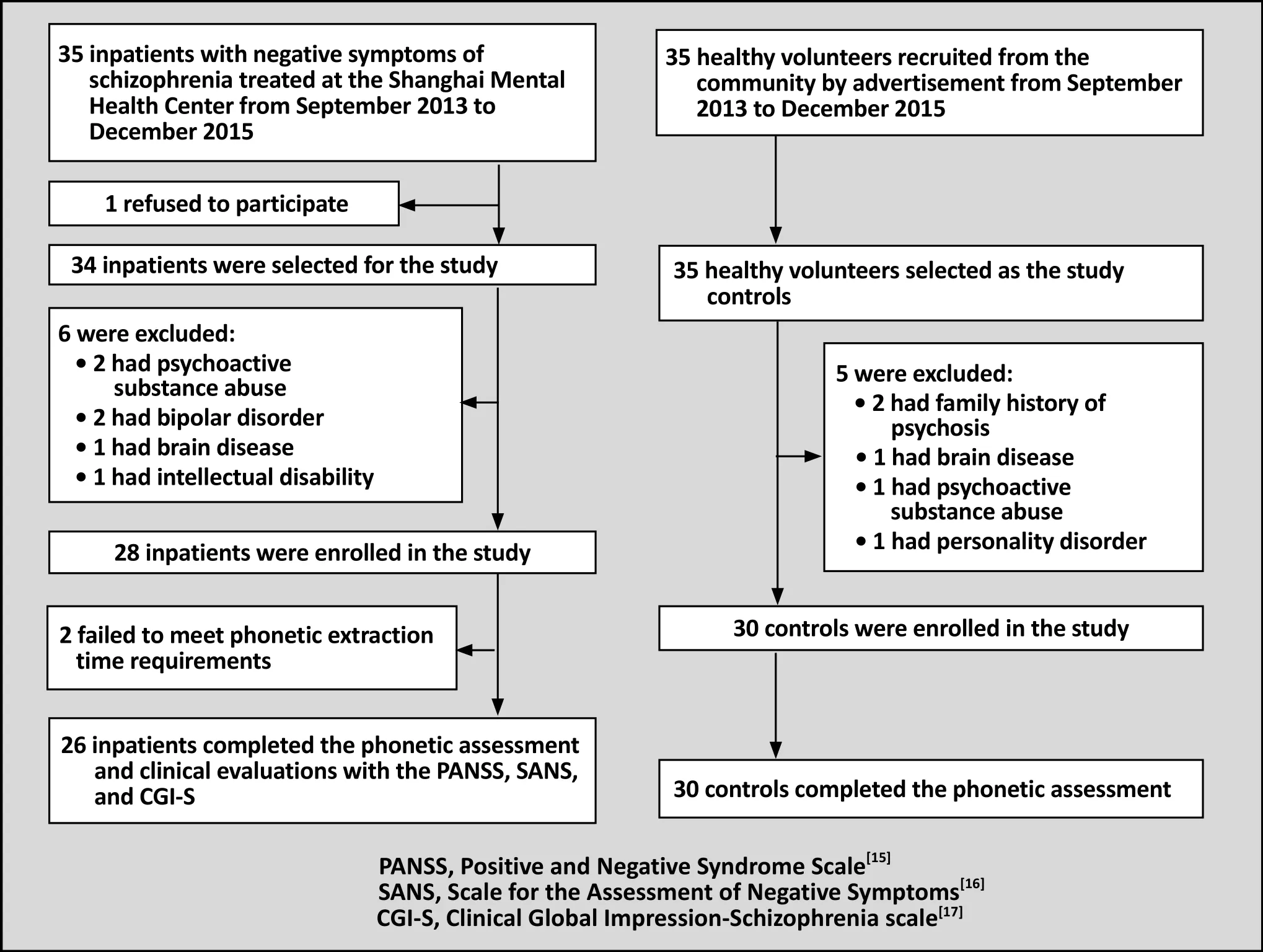
Figure 1. Flowchart of the study
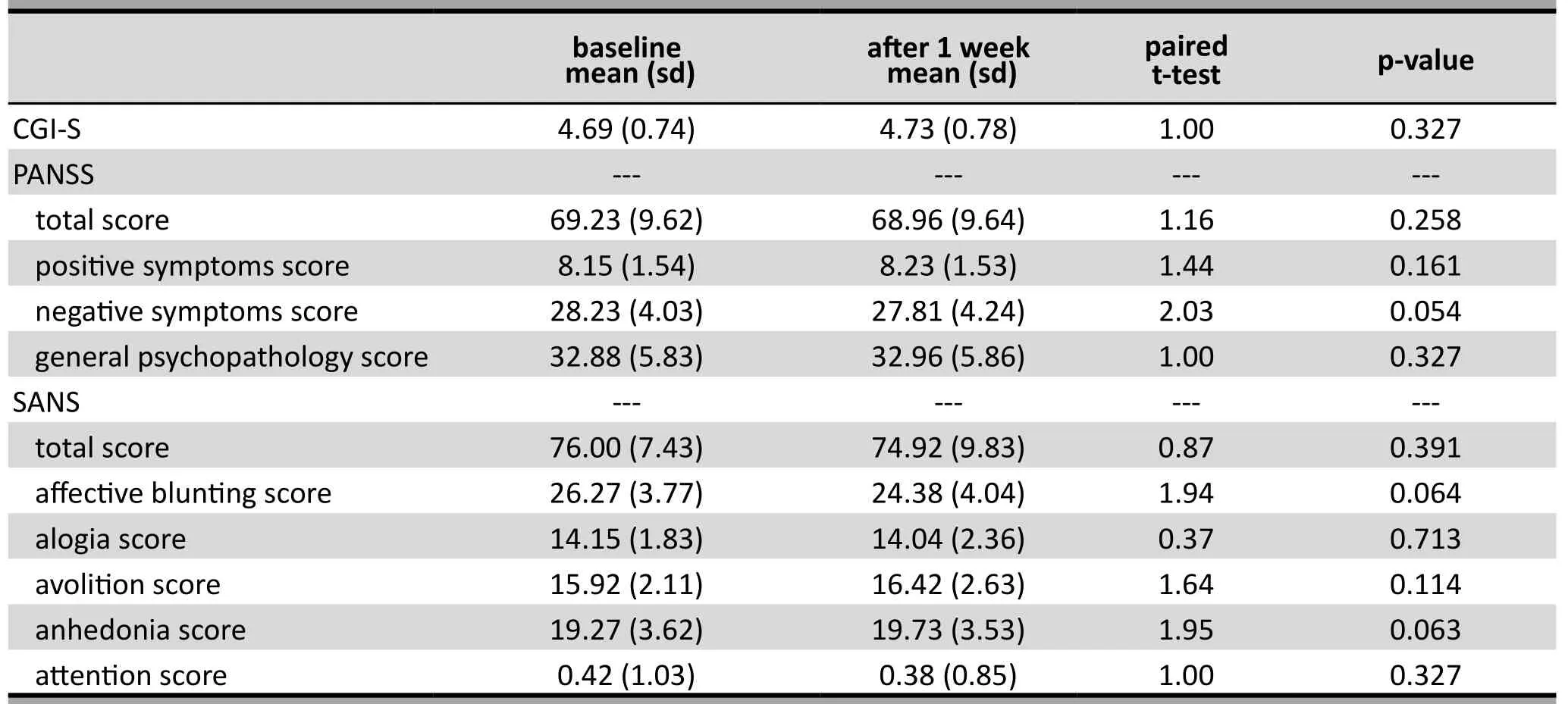
Table 1. Comparisons of clinical symptoms in 26 patients with schizophrenia at baseline and after 1 week

Table 2. Comparisons of speech features at baseline and after 1 week in the patient group and between patient and control groups at baseline
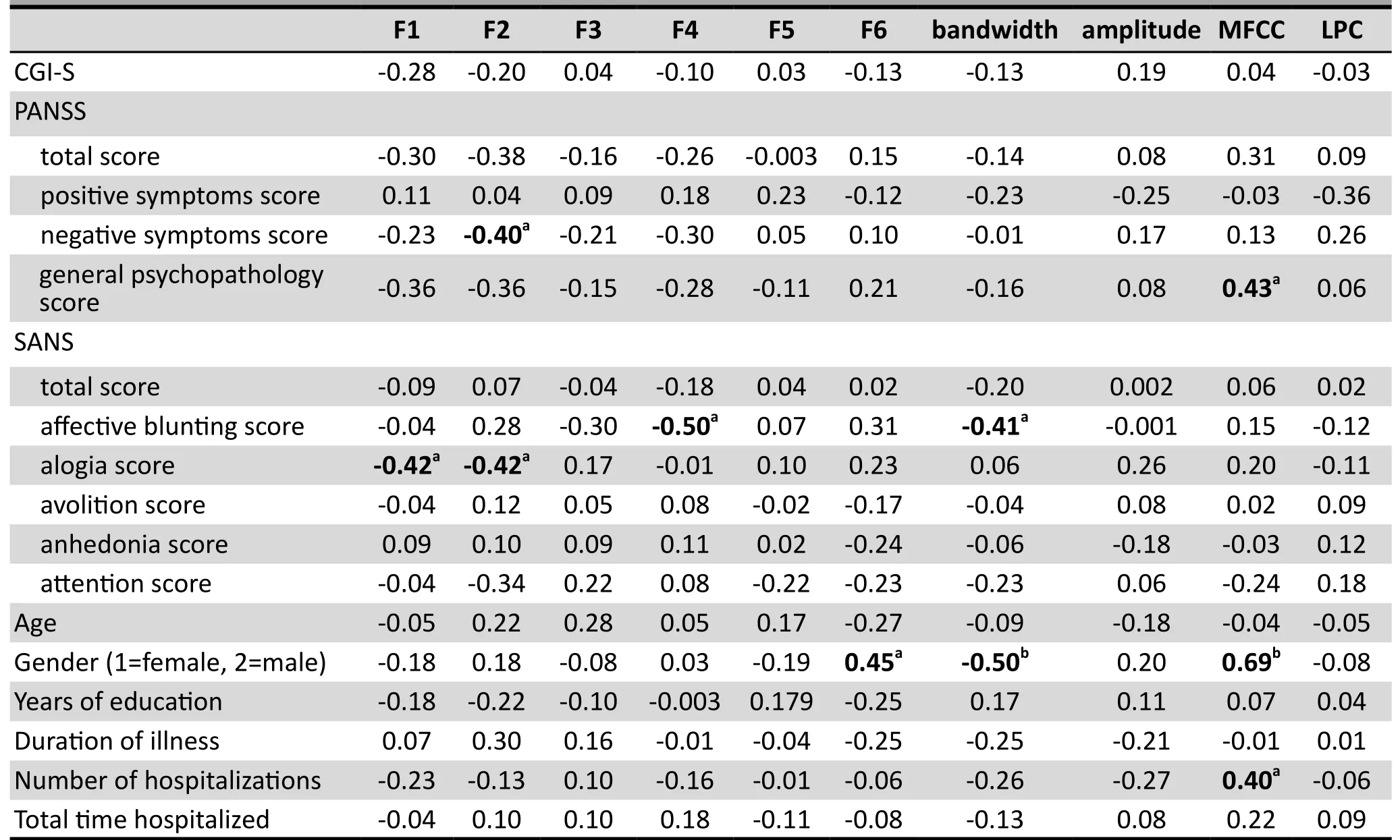
Table 3. Correlation of demographic characteristics and the severity of clinical symptoms (at baseline) with the speech features in 26 patients with schizophrenia (Pearson's r)
We found that when the severity of psychiatric symptoms remains stable, the speech features selected to assess the emotional content of the voice samples of patients with schizophrenia with prominent negative symptoms were also stable over a 1-week period.Correlation analyses of these measures with clinical and demographic characteristics of the patients identified several potentially important relationships, a finding that has been reported in previous studies.[8-10]Comparison of these speech features between patients and matched healthy controls found no statistically significant differences in the prosody features or formant bandwidth and amplitude, but there were significant differences in the two spectral features considered: the MFCC was significantly lower in patients than controls, while the LPC was significantly higher in patients than controls.
Other studies have reported that these two spectral features play an important role in everyday communications.[18]Spectral features have also been found to be useful for discriminating emotions in artificial intelligence studies. The LPC is a relatively efficient and accurate measure of the waveform and spectrum of speech that is used in speech coding,speech synthesis, speech identification, and other applications.[19,20]The MFCC, which modifies external signals in a manner similar to the human ear, is a reliable parameter for discriminating different emotional states.[21,22]Similar to our results, a study by Sun and colleagues[23]found that (when using a sorter based on a Gaussian mixture model [GMM] algorithm) the MFCC was better at discriminating different emotional states than the prosody features. Further work is needed to determine whether or not these spectral features can be used as biomarkers for the identification and monitoring of schizophrenia or of the prominent negative symptom subtype of schizophrenia.
The correlation analysis identified some intriguing associations between 6 of the 10 speech signal features considered (F1, F2, F4, F6, bandwidth, and MFCC)and 6 of the 17 clinical and demographic parameters considered (gender, the PANSS negative symptoms and general psychopathology subscale scores, the SANS affective blunting and alogia subscale scores,and the number of hospitalizations). Other studies have also identified significant correlations between different speech features and the negative symptoms of schizophrenia.[11]This raises the possibility that a subset of acoustic parameters of a standardized speech sample – potentially transmitted over a smart phone to clinicians – could be used to either monitor the severity of negative symptoms or predict the subsequent course of the illness. However, given the small sample size and the large number of potential associations considered in the current study, these results need to be replicated before they can be meaningfully interpreted.
4.2 Limitations
The present study has several limitations that need to be considered when interpreting the results. The speech features selected may not be the most sensitive measures of changes in chronic schizophrenia; further research using a wider range of measures will be needed to find other, potentially more sensitive,measures. The 1-week interval we used to assess the test-retest reliability of the speech features indicated short-term stability in the phonetic parameters, but we are uncertain how stable such measures are over a longer time period. A total of 170 correlations between the 10 speech features assessed and 17 clinical and demographic characteristics are considered, so the statistically significant relationships identified may be chance findings; repeat studies are needed to confirm their importance. The comparison between patients and controls was cross-sectional so we cannot report on the sensitivity of the speech features to changes in clinical symptoms; longitudinal studies that compare changes in the speech features to changes in the clinical measures will be needed to determine their potential utility as biomarkers of clinical changes. All the patients included in the study had a prolonged course of illness and had been on antipsychotic medication for many years, so it is possible that this may have had an effect on the assessed speech features.[15,16,18]Finally, the sample was quite small – only 26 patients – so some of the negative findings (e.g., failure to identify differences between patients and controls) may have been due to Type II errors.
4.3 Importance
This study focused on the negative symptoms of schizophrenia, symptoms that are often not improved with standard antipsychotic medications and that often predict a poor prognosis and progressive deterioration in social functioning.[15]The study is a preliminary assessment of the feasibility of using speech features that assess the emotional characteristics of speech as biomarkers for the severity of negative symptoms in schizophrenia and, thus, as potential predictors of the prognosis of the disorder. The selected speech features included both the prosodic variables used in prior studies (i.e., rate, volume, rhythm, etc.) and two spectral features (MFCC and LPC) that have previously been shown to be useful in the emotional characterization of speech samples. These speech features proved to be stable (over a short period), some of them – the spectral features rather than the prosody features reported in some previous studies – were significantly different between patients and controls, and some of them were significantly correlated with clinical measures of negative symptoms. However, this was a cross-sectional study in a small group of chronic patients, so much more detailed studies using larger samples of more diverse patients that are followed over time will be needed before the potential utility of such speech features can be fully assessed.
Funding
Shanghai public health outstanding academic leader training program (GWDTR201230); Shanghai Jiao Tong University Key Program for the Medical Engineering Cross Project (YG2012ZD04);and Shanghai Key Laboratory of Psychotic Disorders (13dz2260500).
Conflict of interest statement
The authors report no conflict of interest.
Informed consent
Every participant who participated in this study signed a consent form at the beginning of the study.
Ethical review approval
The study has been approved by the Shanghai Mental Health Center Institutional Review Board (approval number: 2011-15).
Authors' contributions
DHC designed the study and revised the manuscript;J Zhang and ZP recruited patients and healthy controls, gathered speech data, and conducted clinical evaluations; J Zhu and CG conducted the phonetic analyses; J Zhang did the statistical analyses and wrote the first draft of the manuscript.
1. Green MF, Bearden CE, Cannon TD, Alan PF, Hellemann GS,Horan WP, et al. Social cognition in schizophrenia, part 1:performance across phase of illness. Schizophr Bull. 2012;38(4): 854-864. doi: http://dx.doi.org/10.1093/schbul/sbq171
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington,VA: American Psychiatric Association; 2013
3. Zhao L, Jiang CH, Zou CR, Wu ZY. [A study on emotional feature analysis and recognition in speech signal]. Dian Zi Xue Bao. 2004; 32(4): 606-608. Chinese. doi: http://dx.chinadoi.cn/10.3321/j.issn:1000-436X.2000.10.004
4. Nwe TL, Foo SW, Silva LCD. Speech emotion recognition using hidden Markov models. Speech Communication.2003; 41(3): 603-623. doi: http://dx.doi.org/10.1016/S0167-6393(03)00099-2
5. Lin YL, Wei G, Yang KC. [A survey of emotion recognition in speech]. Guangzhou Dian Lu Yu Xi Tong Xue Bao. 2007;12(1): 90-91. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1007-0249.2007.01.019
6. Yuan J, Xu HH, He X. [Research progress of speech emotion recognition]. Ji Suan Ji Guang Pan Ruan Jian Yu Ying Yong.2010; 1: 36-38. Chinese
7. Bhatti MW, Wang Y, Guan L. A neural network approach for human emotion recognition in speech (conference paper). Sydney: Circuits and Systems Conference, ISCAS‘04; 2004. p.181-184. doi: http://dx.doi.org/10.1109/ISCAS.2004.1329238
8. Stassen HH, Albers M, Püschel J, Scharfetter C, Tewesmeier M, Woggon B. Speaking behavior and voice sound characteristics associated with negative schizophrenia.J Psychiatr Res. 1995; 29(4): 277-296. doi: http://dx.doi.org/10.1016/0022-3956(95)00004-O
9. Püschel J, Stassen HH, Bomben G, Scharfetter C, Hell D.Speaking behavior and speech sound characteristics in acute schizophrenia. J Psychiatr Res. 1998; 32(2): 89-97. doi:http://dx.doi.org/10.1016/S0022-3956(98)00046-6
10. Leitman DI, Laukka P, Juslin PN, Saccente E, Butler P, Javitt DC. Getting the cue: sensory contributions to auditory emotion recognition impairments in schizophrenia.Schizophr Bull. 2008; 36(3): 545-556. doi: http://dx.doi.org/10.1093/schbul/sbn115
11. Gold R, Butler P, Revheim N, Leitman DI, Hansen JA, Gur RC, et al. Auditory emotion recognition impairments in schizophrenia: relationship to acoustic features and cognition. Am J Psychiatry. 2012; 169(4): 424-432. doi:http://dx.doi.org/10.1176/appi.ajp.2011.11081230
12. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998; 59 (Suppl 20): 22-33
13. Xu D, Zhang J, Zhu J, Cui D. Acoustic Analysis and Identification of Manic Psychosis Patients. London:Intelligent Signal Processing Conference; 2013
14. Gui C, Li W, Pan Z, Zhang J, Zhu J, Cui D. A classifier for diagnosis of manic psychosis state based on SVM-GMM.Sydney: The 10th International Conference on Information Technology and Applications (ICITA2015); 2015
15. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull.1987; 13(2): 261-276. PMID 3616518. doi: http://dx.doi.org/10.1093/schbul/13.2.261.
16. Andreasen NC. Negative symptoms in schizophrenia:definition and reliability. Arch Gen Psychiatry. 1982; 39(7):784-788
17. Haro J, Kamath S, Ochoa S, Novick D, Rele K, Fargas A, et al.The Clinical Global Impression-Schizophrenia scale: a simple instrument to measure the diversity of symptoms present in schizophrenia. Acta Psychiatrica Scandinavica. 2003;107(Suppl 416): 16-23. doi: http://dx.doi.org/10.1034/j.1600-0447.107.s416.5.x
18. Sun Y, Jiang ZC, Wang DF. [Analysis and application of voice spectrum]. Ji Suan Ji Yu Xian Dai Hua. 2010; 4:200-202. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1006-2475.2010.04.054
19. Yu BK, Yu M. [Analysis of the resonance peak of speech signal extracted with LPC method]. Dian Sheng Ji Shu.2000; 3: 3-8. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1002-8684.2000.03.001
20. Nica A, Caruntu A, Toderean G, Buza O. Analysis and synthesis of vowels using Matlab. IEEE Conference on Automation, Quality and Testing, Robotics; 2006. p. 371-374.doi: http://dx.doi.org/10.1109/AQTR.2006.254662
21. Lin W, Yang LL, Xu BL. [Speaker identification in Chinese whispered speech based on modified-MFCC]. Nanjing Da Xue Xue Bao (Zi Ran Ke Xue). 2006; 42(1): 54-61. Chinese. doi: http://dx.chinadoi.cn/10.3321/j.issn:0469-5097.2006.01.008
22. Dave N. Feature extraction methods LPC, PLP and MFCC in speech recognition. Ijaret Org. 2013; 1(6): 1-5
23. Sun MH, Jiang BC. [Analysis and Research on the Emotional Information of Mandarin Speech]. Shandong: Shandong University. 2011; p. 22-24. Chinese
(received, 2016-02-19; accepted, 2016-03-22)

Dr. Jing Zhang graduated from Wannan Medical College with a bachelor’s degree in medicine in 2007.She is now a master’s student at the Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine. She has been working in the Department of Psychiatry as an attending physician in the Jiading District Mental Health Center in Shanghai since 2009. Her main research interest is the diagnostic relevance of speech signals in patients with schizophrenia.
精神分裂癥患者語音信號的臨床分析
張靜, 潘忠德, 桂超, 朱杰, 崔東紅
精神分裂癥;語音;生物標志;陰性癥狀;中國
Background:A new area of interest in the search for biomarkers for schizophrenia is the study of the acoustic parameters of speech called 'speech signal features'. Several of these features have been shown to be related to emotional responsiveness, a characteristic that is notably restricted in patients with schizophrenia,particularly those with prominent negative symptoms.Aim:Assess the relationship of selected acoustic parameters of speech to the severity of clinical symptoms in patients with chronic schizophrenia and compare these characteristics between patients and matched healthy controls.Methods:Ten speech signal features – six prosody features, formant bandwidth and amplitude, and two spectral features – were assessed using 15-minute speech samples obtained by smartphone from 26 inpatients with chronic schizophrenia (at enrollment and 1 week later) and from 30 healthy controls (at enrollment only). Clinical symptoms of the patients were also assessed at baseline and 1 week later using the Positive and Negative Syndrome Scale, the Scale for the Assessment of Negative Symptoms, and the Clinical Global Impression-Schizophrenia scale.Results:In the patient group the symptoms were stable over the 1-week interval and the 1-week test-retest reliability of the 10 speech features was good (intraclass correlation coefficients [ICC] ranging from 0.55 to 0.88). Comparison of the speech features between patients and controls found no significant differences in the six prosody features or in the formant bandwidth and amplitude features, but the two spectral features were different: the Mel-frequency cepstral coefficient (MFCC) scores were significantly lower in the patient group than in the control group, and the linear prediction coding (LPC) scores were significantly higher in the patient group than in the control group. Within the patient group, 10 of the 170 associations between the 10 speech features considered and the 17 clinical parameters considered were statistically significant at the p<0.05 level.Conclusions:This study provides some support for the potential value of speech signal features as indicators(i.e., biomarkers) of the severity of negative symptoms in schizophrenia, but more detailed studies using larger samples of more diverse patients that are followed over time will be needed before the potential utility of such acoustic parameters of speech can be fully assessed.
[Shanghai Arch Psychiatry. 2016, 28(2): 95-102.
http://dx.doi.org/10.11919/j.issn.1002-0829.216025]
1Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
2Jiading District Mental Health Center, Shanghai, China
3Shanghai Key Laboratory of Psychotic Disorders, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
4Key Laboratory of Translational Psychiatry, Shanghai Jiao Tong University School of Medicine, Shanghai, China
5School of Electronic Information and Electrical Engineering, Shanghai Jiao Tong University, Shanghai, China
*co-corresponding authors: Dr. Donghong Cui, Shanghai Key Laboratory of Psychotic Disorders, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, 3210 Humin Road, Shanghai 201108, China. E-mail: manyucc@126.com; Jie Zhu, School of Electronic Information and Electrical Engineering, Shanghai Jiao Tong University, 800 Dongchuan Road, Shanghai, China. E-mail: zhujie@sjtu.edu.cn
A full-text Chinese translation of this article will be available at http://dx.doi.org/10.11919/j.issn.1002-0829.216025 on August 25, 2016.
背景:語音參數是精神分裂癥生物學指標研究的一個全新領域,其中一些已被證明與情感反應相關,情感反應是精神分裂癥患者顯著受限制的一個特點,特別是對那些具有突出陰性癥狀的患者。目標:評估慢性精神分裂癥患者的選擇性語音參數與臨床癥狀嚴重程度之間的關系,并比較患者與所匹配的健康對照者的這些特征。方法:對26例住院慢性精神分裂癥患者(入組時和一周后)和30名健康對照者(僅在入組時)通過電話采集的15分鐘語音樣本,對該樣本進行10項語音測量參數的評估,包括6個語音韻律參數、共振峰帶寬和振幅、以及2個頻譜特征。采用陽性與陰性癥狀量表 (Positive and Negative Syndrome Scale)、陰性癥狀評估量表 (Scale for the Assessment of Negative Symptoms)、臨床總體印象量表-精神分裂癥分量表 (the Clinical Global Impression-Schizophrenia scale) 分別在基線和1周后進行患者臨床特征的評估。結果:患者組癥狀在1周的時間間隔中保持穩定,并且10項語音參數的前后一周重測信度良好(內部相關系數 [intraclass correlation coefficient, ICC] 介于0.55到0.88之間)。語音參數中6項韻律參數、共振峰帶寬和振幅參數在患者組和對照組之間沒有顯著差異,但2項光譜參數在組間有差異:患者組美爾頻率倒譜系數 (the Mel-frequency cepstral coefficient, MFCC) 評分顯著低于對照組,并且患者組的線性預測系數 (linear prediction coding, LPC) 評分顯著高于對照組。在患者組中,在10個本研究所考慮的語音參數和17個所考慮的臨床參數之間構成的170個相關性中,有10個達到了p<0.05的統計學顯著性水平(相關系數>0.40)。結論:這項研究支持了語音參數具有作為精神分裂癥陰性癥狀嚴重程度指標(即,生物指標)的潛在價值,但在這些語音參數的潛在效用獲充分評估前,我們需要對更多樣化的患者進行更大樣本量、更詳細的隨訪研究。
本文全文中文版從2016年8月25日起在http://dx.doi.org/10.11919/j.issn.1002-0829.216025可供免費閱覽下載
- 上海精神醫學的其它文章
- Treatment resistant depression or dementia: a case report
- Behavioral and emotional manifestations in a child with Prader-Willi syndrome
- Is the DSM-5 hoarding disorder diagnosis valid in China?
- Disability, psychiatric symptoms, and quality of life in infertile women: a cross-sectional study in Turkey
- A community-based controlled trial of a comprehensive psychological intervention for community residents with diabetes or hypertension
- Huperzine A for treatment of cognitive impairment in major depressive disorder: a systematic review of randomized controlled trials