在MRSA系統(tǒng)性感染模型中Pam3CSK4預處理降低小鼠腎組織的炎癥反應①
黃釗霞 易夏玉 侯曉睿 王湘豫 朱 平 劉北一
(南方醫(yī)科大學基礎醫(yī)學院免疫學教研室,廣州 510515)
·臨床免疫學·
在MRSA系統(tǒng)性感染模型中Pam3CSK4預處理降低小鼠腎組織的炎癥反應①
黃釗霞 易夏玉 侯曉睿 王湘豫 朱 平 劉北一
(南方醫(yī)科大學基礎醫(yī)學院免疫學教研室,廣州 510515)
目的在耐甲氧西林金葡菌(MRSA)系統(tǒng)性感染模型中,觀察低劑量TLR2激動劑Pam3CSK4預處理對小鼠腎組織中炎癥反應的影響并初步探討其機制。方法于感染前48 h、24 h對BALB/c小鼠行尾靜脈注射 Pam3CSK4 (10 μg/100 μl/只);2×107CFU/只MRSA經(jīng)靜脈感染小鼠,ELISA和熒光實時定量PCR(Q-PCR)檢測細胞因子水平,Q-PCR檢測TLR2、IRAKs等相對表達量,Western blot檢測NF-κB p65磷酸化、IRAK-M及A20表達。結(jié)果與對照組相比,預處理組在感染6 h后腎組織中TNF-α、IL-6、IL-1β、CCL3和IFN-γ含量顯著減少,iNOS表達量降低,IL-10和TGF-β表達量增高,TLR2表達下降;處理組腎組織在感染12 h后IRAK-1表達無明顯增加,而IRAK-M表達量顯著增加;Western blot結(jié)果顯示Pam3CSK4預處理組NF-κBp65磷酸化降低,IRAK-M表達明顯增高。結(jié)論Pam3CSK4預處理降低MRSA系統(tǒng)性感染小鼠腎組織的炎癥反應,這可能與誘導IRAK-M表達相關。
TLR2;Pam3CSK4;耐甲氧西林金葡菌;炎癥;IRAK-M
金黃色葡萄球菌(Staphylococcus aureus,S.aureus)是一種常見的G+菌,是社區(qū)和院內(nèi)感染的主要致病菌之一,除可引起輕度的皮膚和軟組織感染外,還可引發(fā)危及生命的肺炎、心內(nèi)膜炎、膿毒癥等[1]。由于抗生素廣泛應用,導致細菌耐藥情況嚴重,甚至出現(xiàn)耐甲氧西林(MRSA)和耐萬古霉素的超級耐藥菌,給臨床治療帶來極大困難。機體在應對感染中產(chǎn)生大量促炎性細胞因子以增強中性粒細胞及單核-巨噬細胞清除細菌,然而促炎性細胞因子的過度分泌則導致組織損傷,甚至參與膿毒癥性休克、多器官功能衰竭的發(fā)生與發(fā)展[2],因此在針對MRSA系統(tǒng)性感染中,除尋找新型抗生素藥物外,人們嘗試利用免疫調(diào)節(jié)以達到抗感染和炎癥反應的平衡。
TLR2是重要的模式識別受體,廣泛表達于單核-巨噬細胞、樹突狀細胞、肥大細胞和嗜堿性粒細胞等固有免疫細胞表面[3]。TLR2與TLR1或TLR6構成異二聚體,識別G+菌中多種成分,包括肽聚糖(Peptidoglycan,PGN)、脂磷壁酸(Lipoteichoic acid,LTA)以及脂蛋白[4]。TLR2/TLR1或TLR2/TLR6在識別配體后,激活胞內(nèi)Toll/IL-1 受體同源區(qū)TIR(Toll/IL-1 receptor homologous region,TIR),白介素1受體相關蛋白激酶-1(IL-1R associated kinase-1,IRAK-1)磷酸化,最終激活核因子κB(Nuclear factor κB,NF-κB)并誘導炎癥因子的表達[5]。
Pam3CSK4是TLR1/TLR2配體,為人工合成的三酰脂肽。有文獻表明Pam3CSK4預處理后可保護小鼠抵御MRSA感染所致肺炎、眼內(nèi)炎[6,7];Pam3CSK4注射降低鉤端螺旋體在倉鼠體內(nèi)致病性、提高其生存率[8],但對于Pam3CSK4處理降低感染過程中炎癥反應機制不清。基于腎臟是MRSA感染的主要器官,TLR2豐富表達于腎髓質(zhì)處的腎小管、腎小球以及血管內(nèi)皮細胞[9],本文觀察Pam3CSK4預處理對MRSA菌血癥模型中腎組織中炎癥反應的影響,并初步探討其降低炎癥反應的機制。
1 材料與方法
1.1實驗材料、試劑 4~6周齡SPF級 BALB/c小鼠購于南方醫(yī)科大學實驗動物中心;MRSA43300購自溫州康泰生物技術有限公司;Pam3CSK4購自Invivogen公司;TNF-α、IL-6、IFN-γ、IL-1β、CCL3 ELISA試劑盒購于eBioscience公司,總RNA提取試劑盒(RNAiso Plus)、逆轉(zhuǎn)錄試劑盒、PCR擴增試劑盒為TaKaRa公司產(chǎn)品;兔抗IRAK-M 多克隆抗體和兔抗NF-κB p65單抗購自Abcam公司,兔抗phospho-NF-κB p65 (Ser468)抗體、兔抗β-actin抗體、抗A20單克隆抗體、10×RIPA及Protease/Phosphatase Inhibitor Cocktail購自CST公司;BCA蛋白定量試劑盒和ECL購于碧云天公司;引物為廣州英濰捷基公司合成,其余試劑均為國產(chǎn)分析純。
1.2實驗方法
1.2.1MRSA(ATCC 43300)的培養(yǎng) 常規(guī)培養(yǎng)細菌至對數(shù)期(4~5 h),于600 nm處測定光密度(OD)估算細菌量(1 OD600≈1×109CFU/ml),以無菌生理鹽水調(diào)整細菌至所需菌量。
1.2.2Pam3CSK4預處理及MRSA系統(tǒng)性感染 BALB/c小鼠(雌性,4~6周)隨機分組,每組5~10只,實驗組在感染前48 h、24 h分別以10 μg/(100 μl·只)連續(xù)兩次尾靜脈注射Pam3CSK4,對照組在同一時間點尾靜脈注射無菌PBS 100 μl/只,末次處理24 h后尾靜脈注射MRSA(2×107CFU/只)。
1.2.3ELISA檢測細胞因子含量 按1.2.2方法預處理及感染BALB/c鼠6 h,收取同側(cè)腎組織,于無菌PBS中研磨臟器,4℃ 2 000 r/min離心10 min,分離上清和細胞,按eBioscience ELISA試劑盒檢測上清液中TNF-α、IL-6、IL-1β、CCL3和IFN-γ含量。
1.2.4real-time PCR 按1.2.2方法預處理及感染BALB/c小鼠;按1.2.3收集腎組織研磨后的細胞沉淀,提取總RNA,按TaKaRa試劑盒逆轉(zhuǎn)錄cDNA,real-time PCR檢測腎組織中IL-10、TGF-β、iNOS、TLR2、TLR1、TLR6、NOD2、IRAK-1、IRAK-4、IRAK-M、A20、SOCS1及SHP1基因的相對表達量。引物序列見表1。
1.2.5Western blot 按1.2.2方法預處理及感染BALB/c鼠,在感染后不同時間收取預處理組和對照組小鼠同側(cè)腎組織于研磨器中,加含Protease/Phosphatase Inhibitor Cocktail的1×RIPA,冰浴研磨,4℃ 14 000 r/min離心10 min,收取上清。BCA法蛋白定量。配制SDS-PAGE (5%積層膠、10%分離膠),以30 μg/泳道上樣、電泳,電轉(zhuǎn)移至PVDF膜,5%BSA/TBST封閉,洗膜后分別加兔抗Phospho-NF-κB p65(Ser468)單抗、兔抗NF-κB p65、兔抗IRAK-M及兔抗A20抗體,4℃ 過夜孵育,洗膜后加HRP-羊抗兔多抗(Jackson,1∶10 000)室溫孵育2 h,洗膜后加ECL,曝光。Stripping buffer洗膜30 min,洗滌后加抗β-actin抗體室溫孵育2 h,加ECL,曝光。
1.3統(tǒng)計學處理 統(tǒng)計數(shù)據(jù)采用SPSS20.0軟件分析,兩組間比較采用Students′t-test,不同組別間比較采用One-way ANOVA。使用Graph Pad Prism5.0軟件作圖。P<0.05為差異具有統(tǒng)計學意義。
2 結(jié)果
2.1系統(tǒng)性感染模型中,Pam3CSK4預處理組小鼠腎臟中炎性細胞因子含量降低,而抑炎性細胞因子表達量增高 由于腎臟是金葡菌系統(tǒng)性感染的首要臟器,我們首先觀察Pam3CSK4預處理是否可以降低小鼠腎臟組織中促炎性細胞因子含量。結(jié)果顯示與PBS處理組相比,MRSA系統(tǒng)性感染6 h后Pam3CSK4預處理組小鼠腎臟中TNF-α、IL-6、IL-1β、IFN-γ和CCL3含量顯著降低(圖1A~E);iNOSmRNA相對表達量降低(圖1F)。Real-time PCR結(jié)果顯示感染6 h后腎臟中具有抑制炎癥反應的IL-10和TGF-β mRNA相對表達量明顯升高(圖1G、H)。上述結(jié)果提示在MRSA感染早期Pam3CSK4預處理降低腎臟中炎癥反應。
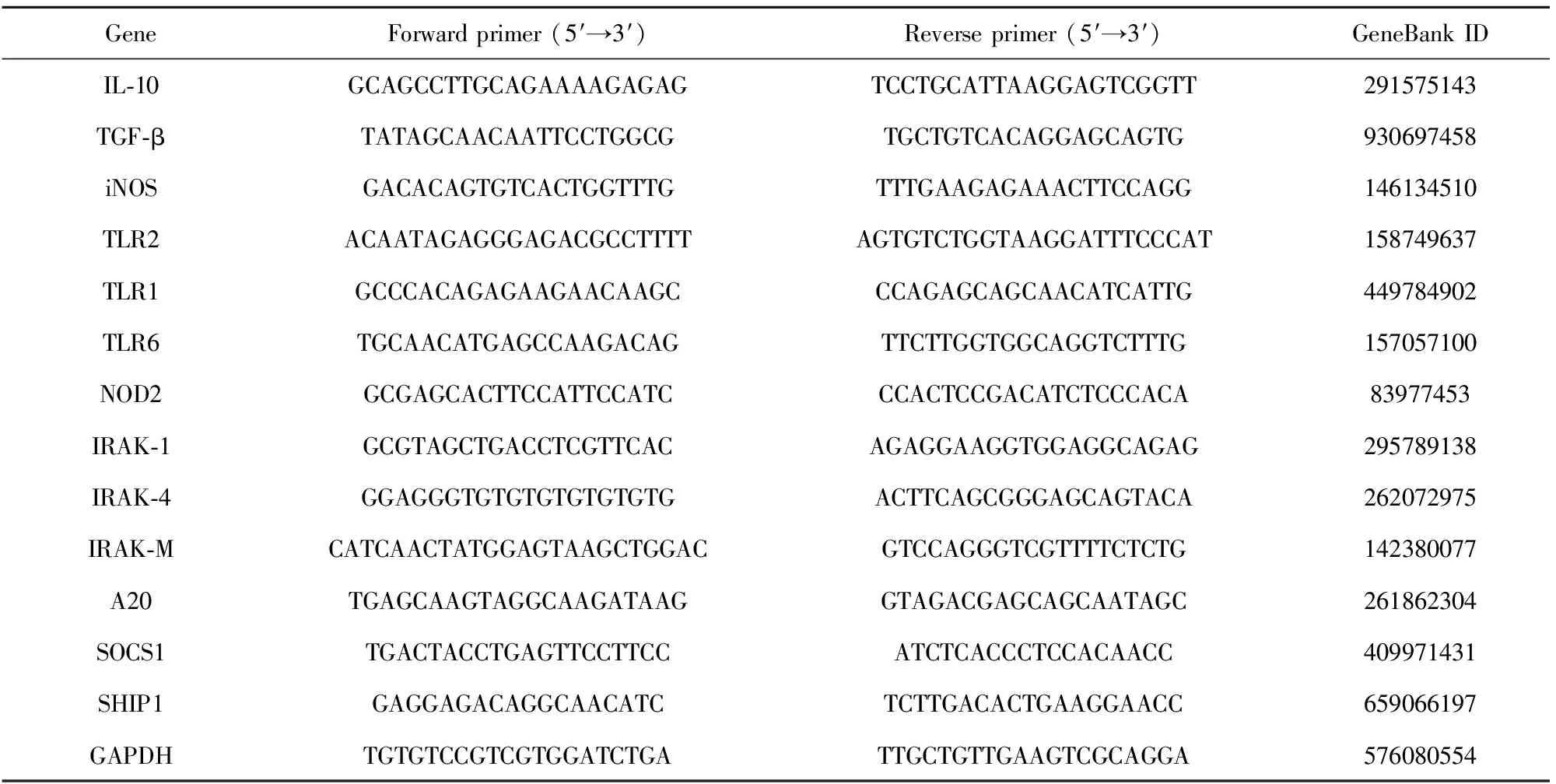
表1 Real-time PCR引物序列

圖1 系統(tǒng)性感染模型中Pam3CSK4預處理組小鼠腎組織中細胞因子水平Fig.1 Detection of levels of cytokines in renal tissue from mice with Pam3CSK4 or PBS treatment post MRSA systemic infectionNote:The level of TNF-α (A),IL-6 (B),IL-1β (C),IFN-γ (D),CCL3 (E) and the relative mRNA expression of iNOS (F),IL-10 (G) and TGF-β (H) in kidney from mice with Pam3CSK4 or PBS treatment post infection.Experiments were performed three times in duplicate wells and the results are shown as ±s.* .P<0.05,***.P<0.001 versus PBS pretreatment.
2.2MRSA系統(tǒng)性感染6 h,Pam3CSK4預處理組小鼠腎組織TLR2表達顯著降低,而TLR1、TLR6、NOD2表達無明顯改變 基于TLR2可分別與TLR1、TLR6形成異二聚體以識別金葡菌,以及NOD2也能識別金葡菌主要成分PGN[10],我們進一步比較在MRSA感染后兩組間TLR1、TLR2、TLR6表達的區(qū)別。結(jié)果顯示MRSA系統(tǒng)性感染6 h后,Pam3CSK4預處理組腎組織中TLR2 mRNA表達量明顯降低(圖2A),而TLR1、TLR6和NOD2的相對表達量在兩組間無明顯差別(圖2B~D)。上述結(jié)果提示Pam3CSK4預處理可能通過調(diào)節(jié)TLR2信號傳導通路以降低腎組織中炎癥反應。
2.3MRSA系統(tǒng)性感染后,Pam3CSK4預處理組小鼠腎組織細胞內(nèi)NF-κB p65磷酸化降低 TLR2信號通路激活后,NF-κB磷酸化、轉(zhuǎn)位至細胞核,細胞因子如TNF-α、IL-6表達并分泌。基于上述促炎性細胞因子在Pam3CSK4處理組顯著降低(圖1),我們首先檢測NF-κB p65亞單位磷酸化,WB結(jié)果顯示,與對照組相比,Pam3CSK4處理組小鼠在感染0 min時NF-κBp65磷酸化即降低,至感染后60 min則無法檢測到,而NF-κB p65總蛋白及作為內(nèi)參的β-actin在各泳道一致(圖3A),提示Pam3CSK4預處理抑制NF-κB p65激活及磷酸化。IRAKs家族中IRAK-1和IRAK-4是TLRs信號傳導通路中的重要分子,TLR識別配體后,胞內(nèi)IRAK-4和IRAK-1激活、磷酸化,繼而激活NF-κB和細胞因子分泌,因此IRAKs分子被認為參與炎癥反應、腫瘤發(fā)展[11,12]。Real-time PCR結(jié)果顯示,PBS處理組IRAK-1在感染后12 h升高并達到高峰,顯著高于Pam3CSK4處理組(圖3B),而Pam3CSK4處理組IRAK-1在感染后6 h雖與對照組無差別,但至12 h無明顯升高(圖3B);兩組間IRAK-4表達在感染后6~24 h無明顯差別(圖3C)。上述結(jié)果提示Pam3CSK4預處理抑制IRAK-1激活。
2.4MRSA系統(tǒng)性感染后,Pam3CSK4預處理組小鼠腎組織中IRAK-M表達顯著增高 與IRAKs家族中IRAK-1和IRAK-4不同,IRAK-M沒有激酶活性,是TLRs信號傳導通路中的負調(diào)控分子,IRAK-M通過抑制IRAK-1激活和磷酸化,抑制IRAK-1/MyD88解離,阻斷IRAK-1/TRAF6復合體形成[13,14];以及下調(diào)CD80信號而達到抑制TLR-NF-κB/AP-1通路激活[15],從而發(fā)揮負調(diào)控作用。IRAK-M豐富表達于小鼠單核-巨噬細胞、中性粒細胞、成纖維細胞和B淋巴細胞,也表達于肺、小腸和肝導管的上皮細胞;在小鼠胸腺、肝臟、心臟、腦及腎臟均表達[16,17]。基于上述觀察到Pam3CSK4預處理組在感染后組織中IRAK-1表達量無明顯增加(圖3B),我們進一步檢測可抑制IRAK-1激活的分子IRAK-M。結(jié)果顯示,與PBS處理組相比,Pam3CSK4預處理組腎組織中IRAK-M表達量在感染后12 h顯著升高(圖4A,P<0.01),其后下降,至感染后24 h兩組間IRAK-M表達無明顯統(tǒng)計學差異(圖4A)。研究表明,除IRAK-M外,SOCS1、SHP-1、A20等負調(diào)控分子也參與下調(diào)TLRs信號通路從而抑制炎癥反應[14,18-20],因此我們進一步檢測這些負調(diào)控分子的表達。與文獻相符的是在感染早期發(fā)揮負調(diào)控作用的A20[21],在PBS組感染后6 h顯著升高(圖4B),其后下降,在感染后12 h至24 h兩組之間無明顯差別,與此不同的是,Pam3CSK4預處理組A20在感染后(0~24 h)無明顯改變。在感染后6 h和12 h,PBS處理組SOCS1顯著高于Pam3CSK4處理組(圖4C,6 h,P<0.05;24 h,P<0.01),而Pam3CSK4處理組在感染后SOCS1無明顯改變;感染后兩組的SHP1表達均逐漸升高,但在兩組間無明顯差異(圖4D)。Western blot結(jié)果進一步顯示Pam3CSK4預處理組在感染后腎組織IRAK-M表達顯著高于對照組,與real-time PCR結(jié)果相符的是A20卻無明顯增高(圖4E),而PBS處理組在感染后A20明顯增高,而IRAK-M表達水平無明顯增加(圖4E)。上述結(jié)果提示IRAK-M表達可能是參與調(diào)控Pam3CSK4預處理降低腎組織中炎癥反應的關鍵分子。

圖2 MRSA感染6 h Pam3CSK4預處理組腎組織中TLR2 mRNA相對表達量降低Fig.2 mRNA relative expression of TLR2 in renal tissue from Pam3CSK4-treated mice was significantly decreased post MRSA infectionNote:The relative mRNA expression of TLR2 (A),TLR1 (B),TLR6 (C) and NOD2 (D) were detected by using real-time PCR.Data were analyzed using the 2-ΔΔCT method;mRNA expression is shown as the fold difference compared to that from PBS-treated mice.Experiments were performed three times in duplicate wells and the results are shown as ±s.ns.No significance,* .P<0.05.

圖3 MRSA感染后,Pam3CSK4預處理組小鼠腎組織中NF-κBp65磷酸化降低、IRAK-1表達量降低Fig.3 Pretreatment with Pam3CSK4 inhibit phosphorylation of NF-κB p65 and expression of IRAK-1 in renal tissue post infection with live S.aureusNote:Phosphorylation of NF-κBp65 was detected by Western blot (A).The relative mRNA expression of IRAK-1(B) and IRAK-4(C) were measured by real-time PCR.Data were analyzed using the 2-ΔΔCT method;mRNA expression is shown as the fold difference compared to that from PBS-treated mice.Experiments were performed three times in duplicate wells and the results are shown as ±s.ns.No significance,* .P<0.05 versus PBS pretreatment cells.

圖4 Pam3CSK4預處理組小鼠在感染后IRAK-M表達顯著增高Fig.4 Pretreatment with Pam3CSK4 induced expression of IRAK-M in renal tissue after MRSA systemic infectionNote:The relative mRNA expression of IRAK-M (A),A20 (B),SOCS1 (C) and SHIP1 (D) was detected by real-time PCR,respectively.Data were analysed using the 2-ΔΔCT method;mRNA expression is shown as the fold difference compared to that from PBS-treated mice.Experiments were performed three times in duplicate wells and the results are shown as mean ± SEM.ns.No significant;*.P<0.05,**.P<0.01 versus PBS pretreatement cells.E.The expression of IRAK-M in kidney from mice treated with PBS(left) or Pam3CSK4(right) was detected by Western blot.
3 討論
MRSA系統(tǒng)性感染中促炎性細胞因子過度分泌加重機體炎癥反應及組織損傷。研究表明MRSA感染以及萬古霉素治療甚至加劇急性腎損傷[22]。因此本文探討了Pam3CSK4預處理對MRSA感染中腎組織炎癥反應的調(diào)節(jié)。結(jié)果顯示在MRSA感染早期(6 h)低劑量Pam3CSK4預處理小鼠腎組織中促炎性細胞因子TNF-α、IL-6、IL-1β、CCL3、IFN-γ及iNOS水平顯著降低,而抑制炎癥反應的IL-10、TGF-β相對表達量增高。
與以往研究不同[6,23],本文發(fā)現(xiàn)低劑量(10 μg/只)Pam3CSK4連續(xù)處理小鼠兩次即能降低MRSA感染后的炎癥反應,這種抑制炎癥反應機制可能體現(xiàn)為針對TLR2信號通路中多個分子,如抑制TLR2表達、短暫下調(diào)TLR信號通路中IRAK-1(圖3B,感染后6~12 h表達量無明顯升高,此后緩慢升高,至24 h后與對照組無差別)及上調(diào)負調(diào)控分子IRAK-M(圖4,感染后12 h內(nèi)表達量明顯增高,12~24 h迅速下降,至24 h與對照組無差別)。提示Pam3CSK4可以作為免疫調(diào)節(jié)劑調(diào)控MRSA感染中腎組織的炎癥反應。
不同的TLRs配體(如LPS、PGN以及LTA)能刺激單核-巨噬細胞胞內(nèi)IRAK-M表達[24-26]。IRAK-M表達降低流感病毒感染所致病理損傷以及哮喘患者中性粒細胞所誘導的組織損傷和重構[27,28],Lech等[29]研究表明在急性腎損傷中IRAK-M充分表達有利于腎組織結(jié)構和功能修復,而IRAK-M缺失則加重腎組織炎癥反應,甚至促進慢性腎功能衰竭,此外IRAK-M缺陷個體易發(fā)炎性腸炎[30]。我們的研究顯示Pam3CSK4預處理降低細菌感染中的炎癥反應并誘導感染早期IRAK-M短暫性表達,因此IRAK-M適度表達有利于控制炎癥及降低感染個體膿毒性休克和多器官衰竭的發(fā)生[16],同時也提示IRAK-M有望作為調(diào)控炎癥反應的靶點。
Hu等[18]發(fā)現(xiàn)A20是Pam3CSK4誘導THP-1細胞耐受的關鍵分子;Günthner等[31]的研究表明LPS可刺激人和小鼠PBMC持續(xù)表達A20和IRAK-M,說明這兩種負調(diào)控分子在抑制炎癥反應中的重要性。而我們的研究顯示在MRSA感染早期,Pam3CSK4預處理上調(diào)IRAK-M,但A20的表達并未明顯增高,其中機制尚不清楚,推測可能與所用實驗體系不同有關。
綜上,本文研究表明低劑量Pam3CSK4預處理降低MRSA系統(tǒng)性感染中小鼠腎組織中的炎癥反應,這種抑炎作用可能與感染早期降低TLR2表達、抑制IRAK-1表達和誘導IRAK-M表達相關。
[1] Lowy FD.Staphylococcus aureus infections[J].N Engl J Med,1998,339(8):520-532.
[2] Wiersinga WJ,Leopold SJ,Cranendonk DR,etal.Host innate immune responses to sepsis[J].Virulence,2014,5(1):36-44.
[3] Chang ZL.Important aspects of Toll-like receptors,ligands and their signaling pathways[J].Inflamm Res,2010,59(10):791-808.
[4] Schenk M,Belisle JT,Modlin RL.TLR2 looks at lipoproteins[J].Immunity,2009,31(6):847-849.
[5] Pietrocola G,Arciola CR,Rindi S,etal.Toll-like receptors (TLRs) in innate immune defense against Staphylococcus aureus[J].Int J Artif Organs,2011,34(9):799-810.
[6] Chen Y,Zhang Y,Deng L,etal.Control of Methicillin-Resistant Staphylococcus aureus Pneumonia Utilizing TLR2 Agonist Pam3CSK4[J].PLoS One,2016,11(3):e149233.
[7] Kochan T,Singla A,Tosi J,etal.Toll-like receptor 2 ligand pretreatment attenuates retinal microglial inflammatory response but enhances phagocytic activity toward Staphylococcus aureus[J].Infect Immun,2012,80(6):2076-2088.
[8] Zhang W,Zhang N,Xie X,etal.Toll-Like Receptor 2 Agonist Pam3CSK4 Alleviates the Pathology of Leptospirosis in Hamster[J].Infect Immun,2016,84(12):3350-3357.
[9] Shigeoka AA,Holscher TD,King AJ,etal.TLR2 is constitutively expressed within the kidney and participates in ischemic renal injury through both MyD88-dependent and-independent pathways[J].J Immunol,2007,178(10):6252-6258.
[10] Girardin SE,Boneca IG,Viala J,etal.Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection[J].J Biol Chem,2003,278(11):8869-8872.
[11] Suzuki N,Suzuki S,Duncan GS,etal.Severe impairment of interleukin-1 and Toll-like receptor signalling in mice lacking IRAK-4[J].Nature,2002,416(6882):750-756.
[12] Jain A,Kaczanowska S,Davila E.IL-1 receptor-associated kinase signaling and its role in inflammation,cancer progression,and therapy resistance[J].Front Immunol,2014,5:553.
[13] Kobayashi K,Hernandez LD,Galan JE,etal.IRAK-M is a negative regulator of Toll-like receptor signaling[J].Cell,2002,110(2):191-202.
[14] Liew FY,Xu D,Brint EK,etal.Negative regulation of toll-like receptor-mediated immune responses[J].Nat Rev Immunol,2005,5(6):446-458.
[15] Nolan A,Kobayashi H,Naveed B,etal.Differential role for CD80 and CD86 in the regulation of the innate immune response in murine polymicrobial sepsis[J].PLoS One,2009,4(8):e6600.
[16] Hubbard LL,Moore BB.IRAK-M regulation and function in host defense and immune homeostasis[J].Infect Dis Rep,2010,2(1):9.
[17] Rosati O,Martin MU.Identification and characterization of murine IRAK-M[J].Biochem Biophys Res Commun,2002,293(5):1472-1477.
[18] Hu J,Wang G,Liu X,etal.A20 is critical for the induction of Pam3CSK4-tolerance in monocytic THP-1 cells[J].PLoS One,2014,9(1):e87528.
[19] Siedlar M,Frankenberger M,Benkhart E,etal.Tolerance induced by the lipopeptide Pam3Cys is due to ablation of IL-1R-associated kinase-1[J].J Immunol,2004,173(4):2736-2745.
[20] Xiong Y,Medvedev AE.Induction of endotoxin tolerance in vivo inhibits activation of IRAK4 and increases negative regulators IRAK-M,SHIP-1,and A20[J].J Leukoc Biol,2011,90(6):1141-1148.
[21] Oshima N,Ishihara S,Rumi MA,etal.A20 is an early responding negative regulator of Toll-like receptor 5 signalling in intestinal epithelial cells during inflammation[J].Clin Exp Immunol,2010,159(2):185-198.
[22] Hammoud K,Brimacombe M,Yu A,etal.Vancomycin trough and acute kidney injury:a large retrospective,cohort study[J].Am J Nephrol,2016,44(6):456-461.
[23] Feterowski C,Novotny A,Kaiser-Moore S,etal.Attenuated pathogenesis of polymicrobial peritonitis in mice after TLR2 agonist pre-treatment involves ST2 up-regulation[J].Int Immunol,2005,17(8):1035-1046.
[24] Siedlar M,Frankenberger M,Benkhart E,etal.Tolerance induced by the lipopeptide Pam3Cys is due to ablation of IL-1R-associated kinase-1[J].J Immunol,2004,173(4):2736-2745.
[25] Nakayama K,Okugawa S,Yanagimoto S,etal.Involvement of IRAK-M in peptidoglycan-induced tolerance in macrophages[J].J Biol Chem,2004,279(8):6629-6634.
[26] Kim HG,Kim NR,Gim MG,etal.Lipoteichoic acid isolated from Lactobacillus plantarum inhibits lipopolysaccharide-induced TNF-alpha production in THP-1 cells and endotoxin shock in mice[J].J Immunol,2008,180(4):2553-2561.
[27] Seki M,Kohno S,Newstead MW,etal.Critical role of IL-1 receptor-associated kinase-M in regulating chemokine-dependent deleterious inflammation in murine influenza pneumonia[J].J Immunol,2010,184(3):1410-1418.
[28] Balaci L,Spada MC,Olla N,etal.IRAK-M is involved in the pathogenesis of early-onset persistent asthma[J].Am J Hum Genet,2007,80(6):1103-1114.
[29] Lech M,Grobmayr R,Ryu M,etal.Macrophage phenotype controls long-term AKI outcomes--kidney regeneration versus atrophy[J].J Am Soc Nephrol,2014,25(2):292-304.
[30] Weersma RK,Oostenbrug LE,Nolte IM,etal.Association of interleukin-1 receptor-associated kinase M (IRAK-M) and inflammatory bowel diseases[J].Scand J Gastroenterol,2007,42(7):827-833.
[31] Günthner R,Kumar VR,Lorenz G,etal.Pattern-recognition receptor signaling regulator mRNA expression in humans and mice,and in transient inflammation or progressive fibrosis[J].Int J Mol Sci,2013,14(9):18124-18147.
[收稿2017-03-20 修回2017-06-03]
(編輯 倪 鵬)
PretreatmentwithPam3CSK4decreasesinflammationinrenaltissuefrommicewithsystemicMRSAinfection
HUANGZhao-Xia,YIXia-Yu,HOUXiao-Rui,WANGXiang-Yu,ZHUPing,LIUBei-Yi.
DepartmentofImmunology,SchoolofBasicMedicalSciences,SouthernMedicalUniversity,Guangzhou510515,China
Objective:To observe whether pretreatment with Pam3CSK4,a TLR2 agonist,could decrease the inflammation response in kidney from mice with systemic MRSA infection,and to investigate the mechanism of the attenuation of inflammation with Pam3CSK4 pretreatment.MethodsBALB/c mice were pretreated with Pam3CSK4 (10 μg/100 μl/each mouse) or PBS via tail vein once daily for two consecutive days.All mice were infected with live MRSA (ATCC43300) at 2×107CFU/each mouse (via tail vein) 24 h after the second treatment.The levels of cytokines in kidney were measured by ELISA and real-time PCR,respectively.The relative expression of TLR2,IRAKs etc.were detected by real-time PCR.Western blot was performed to detect the phosphorylation of NF-κB,the expression of IRAK-M and A20,respectively.ResultsThe level of TNF-α,IL-6,IL-1β,CCL3 and IFN-γ in renal tissue from mice pretreated with Pam3CSK4 was decreased significantly compared with that from PBS-treated mice,respectively.Pam3CSK4 pretreatment down-regulated the relative expression of TLR2,inhibited the expression of IRAK-1 and the phosphorylation of NF-κB post infection.The expression of IRAK-M,one of the negative regulators in TLRs signaling pathway was increased significantly in renal tissue from Pam3CSK4-treated mice post infection.ConclusionPam3CSK4 pretreatment attenuated the inflammation response in kidney from mice with systemic MRSA infection,and these attenuation is related with up-regulation of IRAK-M.
TLR2;Pam3CSK4;MRSA;Inflammation;IRAK-M
①本文受國家自然科學基金(31270980)資助。
R392.11
A
1000-484X(2017)10-1530-06
10.3969/j.issn.1000-484X.2017.10.018
黃釗霞(1990年-),女,碩士,主要從事抗感染免疫方面研究,E-mail:ningsi1990@163.com。
及指導教師:劉北一(1969年-),女,博士,副教授,碩士生導師,主要從事抗感染免疫和疫苗方面研究,E-mail:lbydodo@163.com。

