Multidisciplinary team therapy for left giant adrenocortical carcinoma: A case report
Zheng Zhou, Hong-Mei Luo, Jian Tang, Wu-Jun Xu, Bin-Hui Wang, Xu-Hui Peng, Heng Tan, Li Liu, Xiang-Yang Long, Yu-De Hong, Xiao-Bin Wu, Jian-Ping Wang, Bai-Qi Wang, Hai-Hui Xie, Yong Fang, Yong Luo,Rong Li, Yi Wang
Zheng Zhou, Jian Tang, Wu-Jun Xu, Bin-Hui Wang, Xu-Hui Peng, Heng Tan, Li Liu, Xiang-Yang Long, Yu-De Hong, Xiao-Bin Wu, Yi Wang, Department of Urology, The Second Affiliated Hospital, University of South China, Hengyang 421001, Hunan Province, China
Hong-Mei Luo, Department of Histology and Embryology, Clinical Anatomy and Reproductive Medicine Application Institute, University of South China, Hengyang 421001, Hunan Province,China
Jian-Ping Wang, Department of Endocrinology, The Second Affiliated Hospital of University of South China, Hengyang 421001, Hunan Province, China
Bai-Qi Wang, Department of Oncology, The Second Affiliated Hospital, University of South China, Hengyang 421001, Hunan Province, China
Hai-Hui Xie, Department of Radiotherapy , The Second Affiliated Hospital, University of South China, Hengyang 421001, Hunan Province, China
Yong Fang, Department of Pathology, The Second Affiliated Hospital , University of South China, Hengyang 421001, Hunan Province, China
Yong Luo, Department of ICU, The Second Affiliated Hospital, University of South China,Hengyang 421001, Hunan Province, China
Rong Li, Department of Clinical Pharmacy, The Second Affiliated Hospital, University of South China, Hengyang 421001, Hunan Province, China
Abstract BACKGROUND Adrenocortical carcinoma (ACC) is a rare malignant epithelial tumor originating from adrenocortical cells that carries a very poor prognosis. Metastatic or inoperable diseases are often considered incurable, and treatment remains a challenge. Especially for advanced cases such as ACC complicated with renal venous cancer thrombus, there are few cumulative cases in the literature.CASE SUMMARY The patient in this case was a 39-year-old middle-aged male who was admitted to the hospital for more than half a month due to dizziness and chest tightness.Computed tomography (CT) findings after admission revealed a left retroperitoneal malignant space-occupying lesion, but the origin of the formation of the left renal vein cancer thrombus remained to be determined. It was speculated that it originated from the left adrenal gland, perhaps a retroperitoneal source, and left adrenal mass + left nephrectomy + left renal vein tumor thrombus removal +angioplasty were performed under general anesthesia. Postoperative pathology results indicated a diagnosis of ACC. Postoperative steroid therapy was administered. At 3 mo after surgery, abdominal CT reexamination revealed multiple enlarged retroperitoneal lymph nodes and multiple low-density shadows in the liver, and palliative radiotherapy and mitotane were administered, considering the possibility of metastasis. The patient is currently being followed up.CONCLUSION ACC is a highly malignant tumor. Even if the tumor is removed surgically, there is still the possibility of recurrence. Postoperative mitotane and adjuvant chemoradiotherapy have certain benefits for patients, but they cannot fully offset the poor prognosis of this disease.
Key Words: Adrenocortical carcinoma; Ki-67; Multidisciplinary team; Cancer thrombus;Mitotane; Case report
INTRODUCTION
Adrenocortical carcinoma (ACC) is a rare malignant epithelial tumor that originates from adrenocortical cells and is infrequently seen in the clinic. ACC can be divided into functional and nonfunctional types, with the latter accounting for approximately 40% of cases[1]. Its incidence in the population is 1-2 per million cases per year in North America and 4-12 cases per million cases per year worldwide[2]. The 5-year survival rate and median survival time reported by various medical centers vary to some extent[3-5], with 5-year survival ranging from 16%-47%[6]. The molecular mechanism of ACC is not completely clear at present and may be related to the inactivation of tumor suppressor genes (TP53, Men-1, p57Kip2, and H19), abnormal activation of proto-oncogenes (deletion of GAS, RAS, ACTH receptors), overexpression of growth factor IGF-2, and abnormal activation of the B-catenin gene[7]. In general[8], ACC patients have a poor prognosis and high recurrence rate, even if they actively undergo surgical resection. Ki-67 is a very important prognostic index for determining localized ACC immunohistochemically; if Ki-67 > 10%, the risk of recurrence is significantly increased. In this case, the patient underwent surgical resection of a large ACC from his left side. In a short period of time, the patient’s weight had significantly decreased, and his clinical symptoms had improved.However, postoperative computed tomography (CT) reexamination showed obvious metastatic lesions. After describing this case in detail and providing a review of the literature, we further discuss the treatment and prognosis of ACC patients.
CASE PRESENTATION
Chief complaints
The patient was a 39-year-old middle-aged male who was admitted to the hospital for more than half a month due to dizziness and chest tightness, and he had gained approximately 30 kg in the past 3 mo. CT examination conducted in the local hospital 5 d before admission suggested a left retroperitoneal space-occupying lesion.
History of present illness
The patient presented with numbness of the hands and feet, increased nocturia,nocturia approximately 3-4 times/night, no obvious abdominal pain, abdominal distension, no frequent urination, no urgency, and no hematuria or other symptoms.
History of past illness
The patient was generally healthy and had no special disease history.
Personal and family history
His medical history and family history were unremarkable.
Physical examination
T: 36 ℃, P: 78 times/min, R: 19 times/min, BP: 164/120 mmHg. There was no localized bulge in the bilateral kidney area, no tenderness at the bilateral costal ridge angles, no percussion pain the kidneys, and no obvious tenderness or rebound pain in the entire abdomen.
Laboratory examinations
The results of laboratory examination upon admission revealed the following: alanine aminotransferase: 115 U/L (reference < 40 U/L), uric acid: 526 μmol/L (reference< 420 μmol/L), brain natriuretic peptide: 14,157 pg/mL (reference < 400 pg/mL),aldosterone (sitting up): 616 pg/mL (reference 70-300 pg/mL), aldosterone (recumbent position) 610 pg/mL (reference 30-160 pg/mL), angiotensin II: 86 pg/mL (reference 25-60 pg/mL), K: 2.58 mmol/L (reference 3.5-5.5 mmol/L).
Imaging examinations
CT suggested malignant left retroperitoneal mass with left renal vein cancer thrombus,source to be determined: Left adrenal gland source? (Pheochromocytoma? Cortical cancer?) Retroperitoneal origin? (Leiomyolipoma? Sarcoma?) (Figure 1) and right adrenal atrophy.
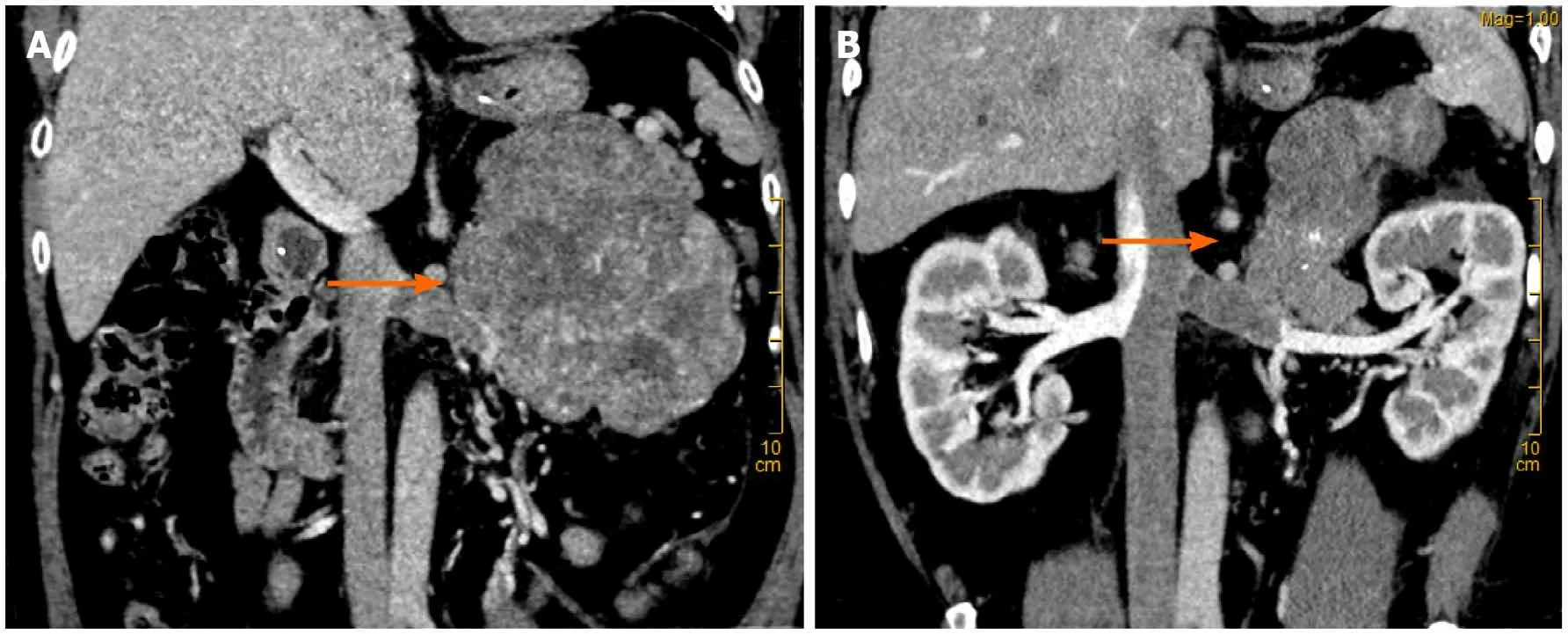
Figure 1 Computerized tomography scan after admission. A: Computer three-dimensional reconstruction (the arrow indicates a retroperitoneal mass); B:Uneven heterogeneous enhancement in the arterial phase.
FINAL DIAGNOSIS
The final diagnosis of the presented case is ACC complicated with renal venous cancer thrombus. Postoperative pathological results are shown in the (Figure 2).
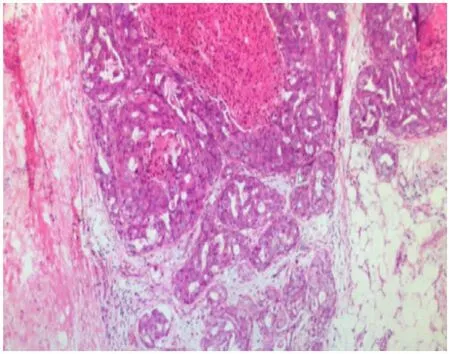
Figure 2 Postoperative pathological results: The tumor cells showed alveolar, solid, trabecular and other growth modes, and the tumor cells showed clear nucleoli and atypia. Some areas of mitotic phase > 20/50 high-power field showed focal necrosis and partial mucinous degeneration.Tumor thrombus could be seen in the vessel. The mass size was 20 cm × 10 cm × 7 cm and was consistent with adrenocortical carcinoma. No renal invasion was observed.Tumor thrombus was observed in the renal vein.Immunohistochemical results revealed the following:S100(-),HMB-45(-),Melan-A(weakly positive),Inhibin-α (weakly positive), CgA(-), CKpan (local focus+), Vimentin(+), Syn(+), TFE3 (nucleus individual+), PAX-8(-), P53 (20% nucleus+), CD34(+), and Ki-67 (15%).
TREATMENT
After admission, the patient was treated with symptomatic treatment to lower blood pressure, correct electrolyte imbalances, protect the liver and diuresis. At 2 d after admission, the patient experienced sudden chest pain and shortness of breath without obvious inducement and coughed up pink foam-like sputum. Considering acute left heart failure, the patient was transferred to the intensive care unit (ICU) for treatment to strengthen the heart, diuresis, protect the liver and stomach, lower blood pressure and correct electrolyte imbalances. After 1 wk of conservative treatment, multiple departments within the hospital were consulted, and surgical treatment was considered based on the opinions of various departments. It was determined that preoperative vasodilation for 2 wk (prazosin 2 mg q8h + spirolactone 80 mg q8h)would be administered. Under general anesthesia, the patient underwent laparoscopic resection of left renal retroperitoneal mass resection + left nephrectomy + left renal vein tumor thrombus removal + angioplasty. A large mass with a hard texture approximately 20 cm × 10 cm × 7 cm in size located in the adrenal region was observed intraoperatively (Figure 3), and the patient’s blood pressure increased significantly when the mass was squeezed. Due to the difficult of laparoscopic separation of the renal pedicle and the inner and lower parts of the mass, a transabdominal laparoscopic approach was used to cut the left peritoneum, and the mass was found to be closely adhered to the pancreas. After careful separation, the pancreatic capsule was sutured with silk thread. After the pedicle was exposed, obvious varicose renal veins were observed, and thrombectomy became difficult under laparoscopic. Therefore,conversion to open surgery was decided for thrombectomy, which was performed by a vascular surgeon. The liver, pancreas, stomach, colon and adrenal gland were not invaded, and no lymph node metastasis was observed. After surgery, he was transferred to the intensive care unit for symptomatic supportive treatment such as correcting heart failure, improving cardiac function, controlling blood pressure, and maintaining homeostasis. In addition, based on the related problems arising from treatment, consultation with a multidisciplinary team was performed half a month after the operation to provide supportive management such as anti-infection treatment, stomach and kidney support, hypotensive control, nutritional support,hemodialysis, and steroid therapy. During the first 3 d after surgery, the patient received hydrocortisone (100 mg q8h). The postoperative multidisciplinary team summary plan was as follows: intravenous hydrocortisone (100 mg q8h) with a gradual dose reduction (50 mg q8h). After 38 d, the prednisone dosage was changed to oral administration of 15 mg early and 5 mg late and hydrocortisone tablets at a dosage of 10 mg early and 5 mg late. After treatment, the general condition of the patient improved, his tolerance for activity increased, and the patient was discharged 48 d after surgery.

Figure 3 The 20 cm × 10 cm × 7 cm adrenal mass (A and B).
OUTCOME AND FOLLOW-UP
CT reexamination 3 mo after surgery indicated the following (Figure 4A): changes after left retroperitoneal mass resection + changes after left nephrectomy; multiple low-density shadows adjacent to enlarged retroperitoneal lymph nodes and the liver indicating a high possibility of metastasis; and right adrenal atrophy was the same as before. Palliative radiotherapy for metastatic left adrenal cortical carcinoma (PTV1: 30 Gy/10F, PTV2: 35 Gy/10F, PTV3: 35 Gy/10F 5 times/wk twice. Mitotane 500 mg q6h.CT reexamination 5 mo after surgery indicated (Figure 4B) local recurrence with invasion and metastasis of the spleen, along with multiple liver metastases and multiple retroperitoneal lymph node metastases that were more advanced than before.Metastases of the sacrum, chest, and lumbar vertebrae were also present. The patient was treated with amlotinib 12 mg qd × 12 d + mitotane 1 g qd + hydrokedasone 30 mg qd. The patient is currently being followed up.

Figure 4 Multiple retroperitoneal lymph node metastases increased (the arrow on the left indicates hepatic metastases, the arrow on the right indicates spleen metastases). A: After the peritoneum was visible in the operative area, a nodular soft tissue density shadow with a size of approximately 15 mm × 19 mm could be seen. Multiple patchy slightly low-density shadows could be seen scattered in the liver parenchyma with fuzzy boundaries (the arrow indicates a nodular soft tissue density shadow in the retroperitoneal area); B: Local recurrence and invasion of the spleen were observed, with near-elliptical lowdensity foci of approximately 17 mm × 24 mm in the leading edge of the spleen. The number of multiple metastases in the liver increased.
DISCUSSION
ACC is a rare highly invasive endocrine tumor. The vast majority of ACC tumors are larger than 5 cm in diameter, but the size is not the only characteristic for the identification of benign and malignant tumors of the adrenal gland because some of the smaller adrenocortical tumors can shift[9]. Surgery is the main treatment for early metaphase ACC. Resection combined with postoperative adjuvant therapy provides the best possibility for long-term survival and a potential cure for local disease against a recurrent attack on tissues and organs. Interventional surgery, radiofrequency ablation or radiotherapy are options for oligometastases in parenchymal organs. In late ACC, operations cannot generally be performed, and patients may benefit from systemic treatment, including chemotherapy, radiotherapy, immunotherapy, and targeted therapy. Mitotane is now the most effective drug in the treatment of ACC and is applicable to cases that cannot be operated, have failed to shift or where surgery failed to completely resect the ACC. The pharmacological effects of mitotane can lead to adrenal cortical zona fasciculata and zona reticularis necrosis, and it is the only drug approved for use in the United States by the Food and Drug Administration for ACC clinical stages. It was listed as a rare disease drug by the European Medicines Agency in 2004[10]. To avoid drug-induced adrenal insufficiency, appropriate glucocorticoid supplementation can be considered[11]. A total of 177 ACC patients in Italy and Germany were treated with mitotane after radical resection[12], and the results showed that the duration of recurrence-free survival (RFS) in the mitotane group was significantly longer (42 mo) than that in the two control groups (10 mo and 25 mo),and the overall survival rate increased. Other foreign studies have shown that adjuvant therapy with mitotane can prolong the time of RFS (but cannot improve the overall survival rate), especially in combination with radiotherapy. Some patients diagnosed with advanced ACC and low tumor load benefit from monotherapy with mitotane. In patients with metastatic disease, mitotane monotherapy may not be an option. In such patients, the opportunity to combine mitotane with cytotoxic agents should be evaluated. Fassnachtet al[13] conducted a randomized study (including 304 patients) that confirmed that patients treated with mitotane combined with EDP(etoposide + cisplatin + epirubicin) had a significantly higher response and longer median progression-free survival than those treated with mitotane combined with streptocin. Mitotane in combination with EDP is also considered to be the preferred therapy in cases requiring a more aggressive treatment approach. Immunotherapy for ACC is still in the preliminary research stage. Studies have shown that adjuvant radiotherapy for ACC patients shows no significant improvement in overall survival and disease-free survival, but it can reduce the possibility of local tumor recurrence[14]. High tumor load, high tumor grade, high Ki-67 index and uncontrollable symptoms are the main factors affecting the prognosis of patients with advanced disease[15].
CONCLUSION
ACC is a rare disease that has a very poor prognosis, with a 5-year survival rate of less than 50%. Surgical treatment can be used for patients with early-/mid-stage disease confined to the adrenal gland. If the tumor is already in an advanced stage and has metastasized, tumor reduction surgery combined with radiotherapy and chemotherapy is the main treatment, and the overall prognosis of these patients is poor. We report the case of a patient with a large left adrenal mass and tumor thrombus in the left renal vein. The patient experienced recurrence 3 mo after surgery and is currently undergoing radiotherapy and chemotherapy and receiving regular follow-up.
 World Journal of Clinical Cases2021年20期
World Journal of Clinical Cases2021年20期
- World Journal of Clinical Cases的其它文章
- Corrigendum to “Probiotic mixture VSL#3: An overview of basic and clinical studies in chronic diseases”
- Role of gastrointestinal system on transmission and pathogenesis of SARS-CoV-2
- COVID-19: Considerations about immune suppression and biologicals at the time of SARS-CoV-2 pandemic
- Histopathology and immunophenotyping of late onset cutaneous manifestations of COVID-19 in elderly patients: Three case reports
- Hemorrhagic transformation of ischemic cerebral proliferative angiopathy: A case report
- Splenosis masquerading as gastric stromal tumor: A case report
