Management and outcome of bronchial trauma due to blunt versus penetrating injuries
INTRODUCTION
Tracheobronchial injury has long been considered a rare occurrence. The incidence of tracheobronchial injury is 2%-6% among patients with chest trauma[1-5]. Of these patients, approximately 80% die before they arrive at the hospital[5-9]. With the improvement of prehospital care, the number of patients who arrive at the hospital alive has increased[4,6,10]; thus, early diagnosis and treatment should be considered to improve their survival. In view of some differences between the trachea and bronchus, this study examined only bronchial trauma (BT).
MATERIALS AND METHODS
Patients
Data from all patients with chest trauma treated at the Chongqing Emergency Medical Center from July 2005 to June 2020 were reviewed, and BT data were screened for inclusion in a retrospective analysis according to sex, age, injury mechanism, diagnostic and therapeutic methods, and outcome. Patients were divided into two groups according to the injury mechanism: Blunt BT (BBT) and penetrating BT (PBT).
Because no human subjects were involved in this study and because only deidentified data were used, the requirements for ethical review and informed consent were waived by the Institutional Review Board of Chongqing Emergency Medical Center (CEMC), China.
現代物流不僅指原材料、產品等從生產到消費的全程實物流動,還包括伴隨物流活動過程中的物流信息交流,而且,現代物流在使用信息技術以及網絡技術,將以往分離的物流、商流、信息流和運輸、采購、代理、倉儲、配送等環節緊密聯系起來,成為了一條完整的供應鏈。因此可以講,現代物流又是信息流、貨物流、資金流和人才流的統一。
Inclusion and exclusion criteria
Injury involving the main bronchus (grade I branch), lobar bronchus (grade II branch), and segmental bronchus (grade III branch).

Blunt and penetrating lung injury combined with subsegmental bronchus (≤ grade IV) injury.
Diagnosis
此時用戶的隱私泄露,而社交網絡服務提供方難以保護。因為是用戶主動發言,攻擊者所選用參數在現實生活中又難以保密,這就是基于隱私悖論所進行的一次社會工程學攻擊檢測。
In the PBT group, using FAST examinations, hemothorax with shock was observed, emergency thoracotomy was performed, and a BT diagnosis was obtained intraoperatively in all patients; however, a few patients without hemothorax were submitted to CT and FB.
2005年7月,在八國峰會召開前幾天,法國總統希拉克同俄羅斯總統普京和德國總理施羅德在俄國舉行私人會晤時,希拉克開玩笑地說:“英國人為歐盟農業所做的惟一貢獻就是瘋牛病……”
2.原有軟件的基礎上根據實際情況增加相應的功能模塊,使整個ERP系統更加完善且人性化專業化。更加企業自身的個性化需求來定制相應的功能模塊,這樣一來就能使ERP系統更貼合企業的實際,做到更加簡便高效。通過當前的大數據分析以及與軟件供應商的溝通,實現將分散數據進行有效傳遞的信息整理功能,進而提升ERP系統的兼容性與高效性。
Treatment
Chest tube drainage was performed for tension pneumothorax or hemothorax cases; in this process, if respiratory distress worsened, single lumen intubation was immediately performed to reach the contralateral main bronchus to ensure ventilation. Mediastinal drainage was performed for tension pneumomediastinum. Massive hemothorax in penetrating injuries required blood transfusion. In moribund patients, emergency thoracotomy including EDT was required without any preoperative treatment.
After opening the chest cavity, the control method for turbulent bleeding involves temporary clamping of the pulmonary hilum. This maneuver yields the following four benefits: (1) It controls massive hemorrhage and exposes the operative field; (2) When the main bronchus is ruptured, contralateral ventilation is ensured; (3) It prevents the blood from the injured side from flowing into the healthy side of the lung and causing asphyxia; and (4) If the pulmonary vein is injured, coronary artery air embolism can be prevented.
Statistical analysis
All 38 patients in the BBT group had dyspnea, and among them, 13 presented with hemoptysis. All patients received a chest X-ray (
= 6) or CT scan (
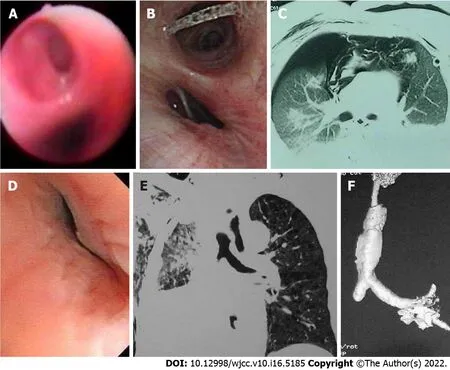
= 29), but three had to undergo EDT due to worsening tension pneumothorax. Positive signs included pneumothorax in 32 (27 tension and 9 hemopneumothorax), subcutaneous emphysema in 29, pneumomediastinum in 15 (8 tension and 1 associated with pneumoperitoneum), total or lobar atelectasis in 28, “fallen lung sign”[3] in 5, pulmonary contusion in 28, rib fracture in 25, clavicle fracture in 9, and sternal fracture in 7. Most patients had both dyspnea and hemoptysis at the same time. Among them, 19 patients with pneumothorax developed delayed atelectasis 5-10 d after injury. Furthermore, clear proof of BT was observed by 3D-spiral CT in 76% (22/29) of patients undergoing this examination. In all 35 patients without EDT, BT was confirmed by FB (Figures 1-5). The median time of definite diagnosis was 68 h (0.5 h to 52 d) after injury, and the diagnosis was delayed over 48 h in 21 (55.3%) patients. All 38 patients underwent emergency or delayed thoracotomy.
RESULTS
A total of 73 patients with BT were admitted during the study period. The proportion of BTs in the entire cohort of chest trauma was 2.4% (73/3018). There were 49 men and 24 women with ages ranging from 16 to 62 years (average, 36.68 ± 11.32 years). In the BBT group (
= 38), the cause of injury was traffic accidents in 17, falls in 10, impacts in 6, and collapses in 5. In the PBT group (
= 35), there were 32 stab wounds and 3 gunshot wounds.
Polytrauma patients accounted for 81.6% of patients in the BBT group and 22.9% in the PBT group; the mean Injury Severity Score was 38.22 ± 8.13 and 21.33 ± 6.12, respectively. The most common intrathoracic-associated injury was pulmonary contusion. On admission, 31.6% of BBT group patients had hemorrhagic shock due to associated injuries, and 88.6% of PBT group patients had shock due to hemothorax.
In the BBT group, the injury was on the left in 16 and on the right in 22, including 18 main bronchi (6 left, 12 right), 12 lobar bronchi (5 left, 7 right), and 8 segmental bronchi (5 left, 3 right). Of the 12 patients with right main bronchial injury, one had simultaneous left lobar bronchial rupture. In the PBT group, there were 25 left and 10 right bronchi, including 2 main bronchi (1 left, 1 right), 11 lobar bronchi (6 left, 5 right), and 22 segmental bronchi (18 left, 4 right).
帶殼烘焙種籽衣的制備:將完整松籽在130 ℃條件下烘焙,取出冷卻至室溫。將松籽剝殼,手工去皮得到種籽衣,密封,避光保存備用。
All data are expressed as the mean ± SD. Comparisons between groups were performed using SPSS 17 by Student’s
test or the chi-square test, as appropriate. Differences were considered significant at
< 0.05.
In the BBT group, among patients sustaining severe chest trauma, the clinical manifestations and physical signs were closely observed. Focused assessment with sonography for trauma (FAST) was performed, but a few patients had to undergo emergency department thoracotomy (EDT) due to tension pneumothorax. Once a BT was suspected, spiral computed tomography (CT) with three-dimensional (3D) reconstruction and fiberoptic bronchoscopy (FB) were performed.
Among the 35 patients in the PBT group, 31 presented with hemothorax with shock, and of them, 12 exhibited hemoptysis. Emergency thoracotomy was performed soon after admission, and the average time from admission to operation was 1.22 ± 0.35 h (0.5 to 6 h). In the remaining four patients without shock, thoracotomy was performed within 12 h after admission because of ongoing hemothorax. Of these 35 patients, eight had preoperative chest X-rays, and seven had CT scans. All images showed hemothorax with no direct evidence of BT. During the operation, BT was found. The surgical methods and outcomes of the 73 patients are shown in Table 1.

In this series, the overall mortality rate was 6.9% (5/73), and it was 7.9% (3/38) in the BBT group and 5.7% (2/35) in the PBT group. Among the three deaths in the BBT group, one died of severe ventilation disturbance caused by bilateral large bronchus injury, one was due to prolonged total atelectasis with pneumonia due to a missed diagnosis of main bronchus injury 48 d later, and another was due to pulmonary hypertension and right heart failure 1 year after pneumonectomy. The causes of two deaths in the PBT group were exsanguination from the hilum during the operation and sepsis after the operation.
In the BBT group, postoperative complications included atelectasis (
= 8), five cases of which were due to stenosis. Therapy included respiratory physiotherapy and diathermy or cryotherapy of granulation
FB. Mechanical ventilation was administered cautiously after surgery in three patients. Three cases required reoperation (Table 1). In the PBT group, no significant complications were observed.
many修飾可數名詞復數,much修飾不可數名詞;many和much都可和表示程度副詞so,too,as,how連用。
然而本文的主要目的,不只是抒發以上自己閱讀了微小說《等》之后的感慨,而是想著重賞析一下它的表現形式與表達技巧,因為這能有效地幫助或啟發更多的微小說創作者去進行更好的文學創作。為什么要這樣做呢?因為表現形式與表達技巧都是為作品內容和作品主題服務的。新穎的表現形式和貼切的表達技巧,一定會增強文學作品的閱讀吸引力和藝術感染力。下面就分別對微小說《等》的新穎的表現形式與貼切的表達技巧進行賞析。
DISCUSSION
The number of BT patients has increased due to improvements in prehospital care, as well as CT and FB. Failure to diagnose BT early can lead to catastrophic outcomes, such as lethal tension pneumothorax and stubborn atelectasis with pneumonia due to stenosis (Figures 2A, 2E, 3A-D, 4B, and 5D). Early diagnosis and treatment clearly decrease morbidity and mortality. Unfortunately, the diagnosis of BBT is often delayed until refractory atelectasis with pneumonia occurs, and many cases are diagnosed by FB only weeks after the injury[11-14]. In the BBT group of this series, 55.3% of patients were diagnosed more than 48 h after the injury. In victims of high-energy blunt thoracic trauma, BT should be strongly considered to detect the associated injuries. Common presenting signs include dyspnea, subcutaneous emphysema, and hemoptysis. X-ray or CT findings are most commonly pneumothorax, pneumomediastinum, atelectasis, pulmonary contusion, and rib fractures. There was one case of tension pneumomediastinum with pneumoperitoneum in this series. This rare phenomenon is considered pneumoperi-toneum caused by air passing through the aortic and esophageal hiatus[15,16]. Among the abovementioned conditions, pneumothorax (or pneumomediastinum) and atelectasis are the most important. The former appears immediately after injury, while the latter can be in the early or late stage or from early pneumothorax to late atelectasis.



There are two main causes of atelectasis after blunt chest trauma: Pulmonary contusion and BT. In the first condition, atelectasis is caused by a decrease in pulmonary compliance due to edema, effusion, bleeding, and obstruction of the bronchial lumen due to clotting and secretions. In BT patients, atelectasis can be caused by obstruction of the lumen due to clots or the dislocation of injured cartilage in the acute phase and by bronchial stenosis with granulation in the delayed phase. Therefore, differential diagnosis is required when posttraumatic atelectasis exists. The most important diagnostic methods are 3D-spiral CT and FB, especially FB, which is recognized as the gold standard for diagnosis[14,15,17-19].
The study was reviewed and approved for publication by the Institutional Review Board of Chongqing Emergency Medical Center (CEMC), China.

Once BT is confirmed or highly suspected, thoracotomy should be performed immediately. The surgical method primarily depends on the location and degree of injury. If the tear is less than 1/3 of the circumference of the tube or is longitudinal, a simple suture can be placed in the main or lobar bronchus; otherwise, different procedures should be performed according to the bronchial grade. When the disruption is in the lobar or segmental bronchus, lobectomy or segmental resection can be performed. In this condition, trying to repair the damage is unlikely to succeed because of stenosis after the operation. However, if the damage involves the main bronchus, bronchorrhaphy, end-to-end anastomosis, and sleeve resection are the correct procedures. When accompanied by vascular injury, it should be repaired simultaneously. Many authors have indicated that pneumonectomy should be avoided if possible[7,10,14,20]. Pneumonectomy inevitably leads to pulmonary hypertension and right heart failure. One patient in this group suffered such an outcome (Table 1). Debridement should be performed before anastomosis; otherwise, the rate of failure or complications, such as leakage and stenosis due to granulation, will increase[2,3,14,17]. If the lung can be expanded, anastomosis can be performed. BT that causes total atelectasis can be repaired with a return of pulmonary function for many years after the injury[19]. In this group, one patient underwent reoperation for scar resection and anastomosis with a satisfactory return of pulmonary function 3 years after the injury (Figures 5D and 5E, Table 1). Of course, these issues should be addressed early. After the operation, if pulmonary compliance is poor, mechanical ventilation is needed to maintain lung expansion. The pressure should not be too high, and close observation is needed. There were three such cases in this group, and no leakage was induced.
All 68 survivors were followed for 6 to 42 (23 ± 6.4) mo to observe their clinical manifestations, and they underwent CT, FB, and pulmonary function examinations. All surviving patients exhibited normal lung function and healthy conditions, but three required reoperation, as described above. Comparisons between the two groups are shown in Table 2.
Long-term delayed diagnosis of main bronchial injury leading to atelectasis with severe pneumonia is life-threatening. One patient was admitted to a local hospital after injury and underwent thoracotomy. Unfortunately, BT was missed during the operation. She was subsequently transferred to our hospital 45 d after the injury, and left main BT was confirmed by FB. However, she developed serious pneumonia due to long-term atelectasis and died 3 d later.
研究數據利用SPSS19.0統計學軟件進行分析,計數資料采用x2檢驗,計量采用t檢驗,計量指標用均數± 標準差(±s)表示,P<0.05為差異有統計學意義。
Penetrating BT is different from blunt BT in many aspects and is perhaps much simpler (Table 2). In fact, it is primarily based on two differences: (1) Although there are many explanations for the mechanism of blunt BT, the main explanation is the shearing force. The accompanying vessels are seldom damaged at the same time due to their toughness, so most patients do not have massive hemothorax and shock. In contrast, penetrating BT often involves blood vessels as well, causing massive hemothorax and shock; and (2) Blunt trauma is characterized by extensive injury, including pulmonary parenchyma and extrathoracic injuries. However, penetrating injuries are limited; when PBT occurs, there are fewer pulmonary and extrathoracic injuries. For the above reasons, in penetrating BT, emergency thoracotomy is often required to stop the bleeding, and it is difficult to miss the diagnosis. Preoperative imaging is often absent, and there are fewer postoperative complications. Among the 35 patients in the PBT group, 31 underwent emergency thoracotomy soon after admission, and 4 underwent emergency thoracotomy within 12 h after admission.
When a diagnosis of BT was confirmed or highly suspected, emergency or delayed posterolateral thoracotomy was performed. Repair procedures for bronchial injury included simple suture, debridement and end-to-end anastomosis (including simultaneous repair of vascular injury), partial pneumonectomy (lobe or segment), sleeve resection, or pulmonary tractotomy for ligation of injured vessels and bronchi.
陣列A、陣列B的首、尾端間距偏移時域上的變化情況見圖9。陣列A、陣列B的設計間距為55.126 m。圖9中y軸表示相對設計間距A、陣列B間距的偏差大小。陣列A、陣列B的首、尾端間距均呈現周期性間距變化程度。
Unnecessary pneumonectomy should especially be avoided because there is less lung tissue damage in PBT. Since the 1980s, we have treated deep lung lacerations, including hilar injury, by opening the wound tract, ligating the injured blood vessels and bronchioles, and then suturing the lung laceration without postoperative necrosis or infection of lung tissue. Wall
[21] reported a similar treatment protocol.
In this series, there were more BBTs on the right side, which is similar to most reports[1,3,6,8,22]. However, most of the PBTs were on the left side, and most of them were segmental branch injuries. The reason for this is that most assailants use their right hand, corresponding to the injury being in the left middle and lower part of the chest. Another reason for the fewer penetrating main bronchus injuries is that a hilar penetrating injury is often complicated with massive hemorrhage, which is difficult to survive, even in the hospital.
CONCLUSION
In summary, the difference between blunt and penetrating BTs is obvious. In BBT, patients generally have no vessel injury, and the diagnosis and treatment are easily delayed and missed. The main cause of death is ventilation disturbance due to tension pneumothorax early and refractory atelectasis with pneumonia late. However, in PBT, most patients require emergency thoracotomy because of simultaneous vessel trauma and massive hemothorax; a delayed diagnosis is infrequent. The leading cause of death is hemorrhagic shock. BT focuses on blunt injury. In patients with blunt chest injury, we must be vigilant, perform CT and FB in time to make a clear diagnosis, and strive for early treatment to reduce morbidity and mortality.
ARTICLE HIGHLIGHTS

Research conclusions
The difference between blunt and penetrating BT is obvious. In BBT, patients generally have no vessel injury, and the diagnosis and treatment are easily delayed and missed. The main cause of death is ventilation disturbance due to tension pneumothorax early and refractory atelectasis with pneumonia late. However, in PBT, most patients require emergency thoracotomy because of simultaneous vessel trauma and massive hemothorax; a delayed diagnosis is infrequent. The leading cause of death is hemorrhagic shock.
Research perspectives
Treatment of bronchial injuries should focus more on early diagnosis and timely management.
FOOTNOTES
Gao JM, Li H, Du DY, Yang J, Kong LW, Wang JB, He P, and Wei GB contributed to data collection and analysis; Gao JM contributed to study design, and manuscript writing and editing; Li H, Yang J, and Wei GB reviewed the manuscript.
The first task of emergency treatment is to relieve ventilatory dysfunction, including rapid decompression and drainage of the tension pneumothorax and pneumomediastinum. However, Mattox[11] indicated that when bronchial transection exists, chest tube drainage can result in evacuation of the total tidal volume. In this series, one victim was sent to the emergency department 15 min after injury, and thoracic drainage was immediately placed for bilateral tension pneumothorax. However, her breathing stopped suddenly during the process. EDT showed that the right main and left lobar bronchi were transected, and the total amount of bilateral chest blood was < 500 mL. The patient died of severe ventilation disturbance half an hour after the injury (Table 1). Therefore, when addressing tension pneumothorax resulting from bronchial rupture, thoracic drainage alone is not sufficient. In this case, single lumen intubation should be performed immediately to reach the contralateral main bronchus to ensure ventilation of the contralateral lung. This is also a damage control surgery measure; if there is another injury requiring priority surgery, it can be performed. We do not advocate for double-lumen intubation because it may aggravate bronchial injury. Shemmeri and Vallières[3] have the same opinion. Another alternative is clamping the proximal end of the main bronchus by EDT. When BT is suspected, mechanical ventilation should not be blindly used because it can aggravate the injury or worsen the condition[5,20].
Because no human subjects were involved in this manuscript and because only deidentified data were used, the requirement for ethical review and informed consent were waived by the Institutional Review Board of Chongqing Emergency Medical Center (CEMC), China.
The authors have no conflicts of interest to report.
All the data are available in the article.
The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Jin-Mou Gao 0000-0001-6612-213X; Hui Li 0000-0002-8176-4103; Ding-Yuan Du 0000-0003-2929-5896;Jun Yang 0000-0002-2919-8095; Ling-Wen Kong 0000-0001-7017-5664; Jian-Bai Wang 0000-0002-4505-0955; Ping He 0000-0003-3160-0685; Gong-Bin Wei 0000-0002-7565-571X.
(三)在學習“健康的生活”一章內容時,教材中提到“拒絕毒品、遠離毒品”。青少年時期是一個“出生牛犢不怕虎”的時期,對什么都感到好奇,對什么都想試一試,再加上對毒品的危害認識不清,致使受害人數較多。青少年時期正是迅速生長發育的時期,若吸毒危害比成年人更為嚴重,所以我們要在青少年中開展禁毒教育,使之充分認識毒品的危害,自覺抵制毒品、遠離毒品。在每年的6月26日,制作相關內容的展板,宣傳相關的禁毒知識,并開展講座,以具體事例教育學生,真正從思想上樹立高度警惕意識。
Wang JJ
1.3 觀察指標 分析兩組患者術中出血量、手術時間、術后排氣時間、術后拔管時間、術后腹腔引流量、進食時間、住院時間。于手術前后抽取兩組患者5 ml的空腹靜脈血,以轉速3 000 r/min離心15 min。分離血清后,提取上清液,使用酶法檢測血清膽紅素(total bilirubin,TBIL)、間接膽紅素(indirect bilirubin,IBIL)水平。采取干化學法檢測堿性磷酸酶(alkaline phosphatase,ALP)、淀粉酶(amylase,AMY)水平。
Wang TQ
Wang JJ
1 Madani A, Pecorelli N, Razek T, Spicer J, Ferri LE, Mulder DS. Civilian Airway Trauma: A Single-Institution Experience.
2016 ; 40 : 2658 -2666 [PMID: 27255938 DOI: 10 .1007 /s00268 -016 -3588 -9 ]
2 Welter S, Essaleh W. Management of tracheobronchial injuries. J Thorac Dis 2020 ; 12 : 6143 -6151 [PMID: 33209452 DOI: 10 .21037 /jtd-2019 -as-05 ]
3 Shemmeri E, Vallières E. Blunt Tracheobronchial Trauma. Thorac Surg Clin 2018 ; 28 : 429 -434 [PMID: 30054080 DOI:10 .1016 /j.thorsurg.2018 .04 .008 ]
4 Madden BP. Evolutional trends in the management of tracheal and bronchial injuries. J Thorac Dis 2017 ; 9 : E67 -E70[PMID: 28203439 DOI: 10 .21037 /jtd.2017 .01 .43 ]
5 Bagga B, Kumar A, Chahal A, Gamanagatti S, Kumar S. Traumatic Airway Injuries: Role of Imaging.
2020 ; 49 : 48 -53 [PMID: 30446292 DOI: 10 .1067 /j.cpradiol.2018 .10 .005 ]
6 van Roozendaal LM, van Gool MH, Sprooten RTM, Maesen BAE, Poeze M, Hulsewé KWE, Vissers YLJ, de Loos ER.Surgical treatment of bronchial rupture in blunt chest trauma: a review of literature.
2018 ; 10 : 5576 -5583[PMID: 30416808 DOI: 10 .21037 /jtd.2018 .08 .22 ]
7 Prokakis C, Koletsis EN, Dedeilias P, Fligou F, Filos K, Dougenis D. Airway trauma: a review on epidemiology,mechanisms of injury, diagnosis and treatment.
2014 ; 9 : 117 [PMID: 24980209 DOI:10 .1186 /1749 -8090 -9 -117 ]
8 Rieth A, Varga E, Kovács T, Ottlakán A, Németh T, Furák J. Contemporary management strategies of blunt tracheobronchial injuries.
2021 ; 52 Suppl 1 : S7 -S14 [PMID: 32674886 DOI: 10 .1016 /j.injury.2020 .07 .026 ]
9 Díaz C, Carvajal DF, Morales EI, Sangiovanni S, Fernández-Trujillo L. Right main bronchus rupture associated with blunt chest trauma: a case report.
2019 ; 12 : 39 [PMID: 31823714 DOI: 10 .1186 /s12245 -019 -0258 -3 ]
10 Alassal MA, Ibrahim BM, Elsadeck N. Traumatic intrathoracic tracheobronchial injuries: a study of 78 cases.
2014 ; 22 : 816 -823 [PMID: 24585278 DOI: 10 .1177 /0218492313516777 ]
11 Mattox KL. Thoracic injury requiring surgery. World J Surg 1983 ; 7 : 49 -55 [PMID: 6837066 DOI: 10 .1007 /BF01655912 ]
12 Demondion P, Fabre D, Herve P, Dartevelle P. Posttraumatic main left bronchial rupture. Ann Thorac Surg 2014 ; 97 : e25[PMID: 24384219 DOI: 10 .1016 /j.athoracsur.2013 .08 .070 ]
13 Maskey N, Sapkota R, Thapa B. Bronchial injuries: a tale of differing presentations.
2019 ; 35 : 245 -248 [PMID: 33061017 DOI: 10 .1007 /s12055 -018 -00783 -x]
14 Li Y, Wang G, Wu C, Pan Z, Li H, Wang Q, Wang Y, Dai J. Experience of diagnosis and treatment of traumatic bronchial rupture in children in a single clinical center.
2020 ; 36 : 1019 -1025 [PMID: 32572599 DOI:10 .1007 /s00383 -020 -04703 -2 ]
15 Grewal HS, Dangayach NS, Ahmad U, Ghosh S, Gildea T, Mehta AC. Treatment of Tracheobronchial Injuries: A Contemporary Review.
2019 ; 155 : 595 -604 [PMID: 30059680 DOI: 10 .1016 /j.chest.2018 .07 .018 ]
16 Hong SB, Lee JY, Lee J, Choi KB, Suh JH. Right Main Bronchus Rupture Presenting with Pneumoperitoneum.
2018 ; 51 : 216 -219 [PMID: 29854669 DOI: 10 .5090 /kjtcs.2018 .51 .3 .216 ]
17 Saleh ME, Beshir H, Mohammed WH, Sanad M. Tracheobronchial injuries: tertiary center experience.
2020 ; 28 : 22 -28 [PMID: 31779465 DOI: 10 .1177 /0218492319893822 ]
18 Lin WT, Su SY, Hsieh CF, Lai CC, Chao CM. Traumatic Thoracic Burst Fracture Associated with Bronchial Rupture.
2017 ; 53 : 260 -261 [PMID: 28648782 DOI: 10 .1016 /j.jemermed.2017 .04 .024 ]
19 Carretta A, Melloni G, Bandiera A, Negri G, Voci C, Zannini P. Conservative and surgical treatment of acute posttraumatic tracheobronchial injuries.
2011 ; 35 : 2568 -2574 [PMID: 21901327 DOI:10 .1007 /s00268 -011 -1227 -z]
20 Hsu WC, Schweiger C, Hart CK, Smith M, Varela P, Gutierrez C, Ormaechea M, Cohen AP, Rutter MJ. Management of the Disrupted Airway in Children.
2021 ; 131 : 921 -924 [PMID: 32902861 DOI: 10 .1002 /lary.29051 ]
21 Wall MJ Jr, Hirshberg A, Mattox KL. Pulmonary tractotomy with selective vascular ligation for penetrating injuries to the lung.
1994 ; 168 : 665 -669 [PMID: 7978015 DOI: 10 .1016 /s0002 -9610 (05 )80141 -2 ]
22 Chowdhury S, Griniatsos J. Right main bronchus rupture due to blunt chest trauma. Clin Case Rep 2019 ; 7 : 242 -243[PMID: 30656055 DOI: 10 .1002 /ccr3 .1953 ]
 World Journal of Clinical Cases2022年16期
World Journal of Clinical Cases2022年16期
- World Journal of Clinical Cases的其它文章
- Practical points that gastrointestinal fellows should know in management of COVID-19
- Electroconvulsive therapy plays an irreplaceable role in treatment of major depressive disorder
- Pleural involvement in cryptococcal infection
- Advances in the clinical application of oxycodone in the perioperative period
- Endoscopic surgery for intraventricular hemorrhage: A comparative study and single center surgical experience
- Pediatric acute myeloid leukemia patients with i(17)(q10) mimicking acute promyelocytic leukemia: Two case reports
