微粒體甘油三酯轉運蛋白基因rs1800591變異與老年人群非酒精性脂肪性肝病發生風險的關系
趙錦涵 張晶 張洋 徐瀟藝 勾鈺淞 徐航飛 萬妍 吳劍
摘要:目的 探討老年人群微粒體甘油三酯轉運蛋白(MTTP)基因rs1800591多態性與非酒精性脂肪性肝病(NAFLD)發病風險的關系。方法 本研究的臨床隊列建立在北京京煤集團總醫院門礦醫院,2020年1月11日—2021年9月30日在北京門頭溝社區共招募參加健康體檢1098例老年志愿者,其中NAFLD患者614例,非NAFLD患者484例,采用基因芯片法檢測MTTP rs1800591基因型,收集人口學資料并檢測受試者的血液生化指標。
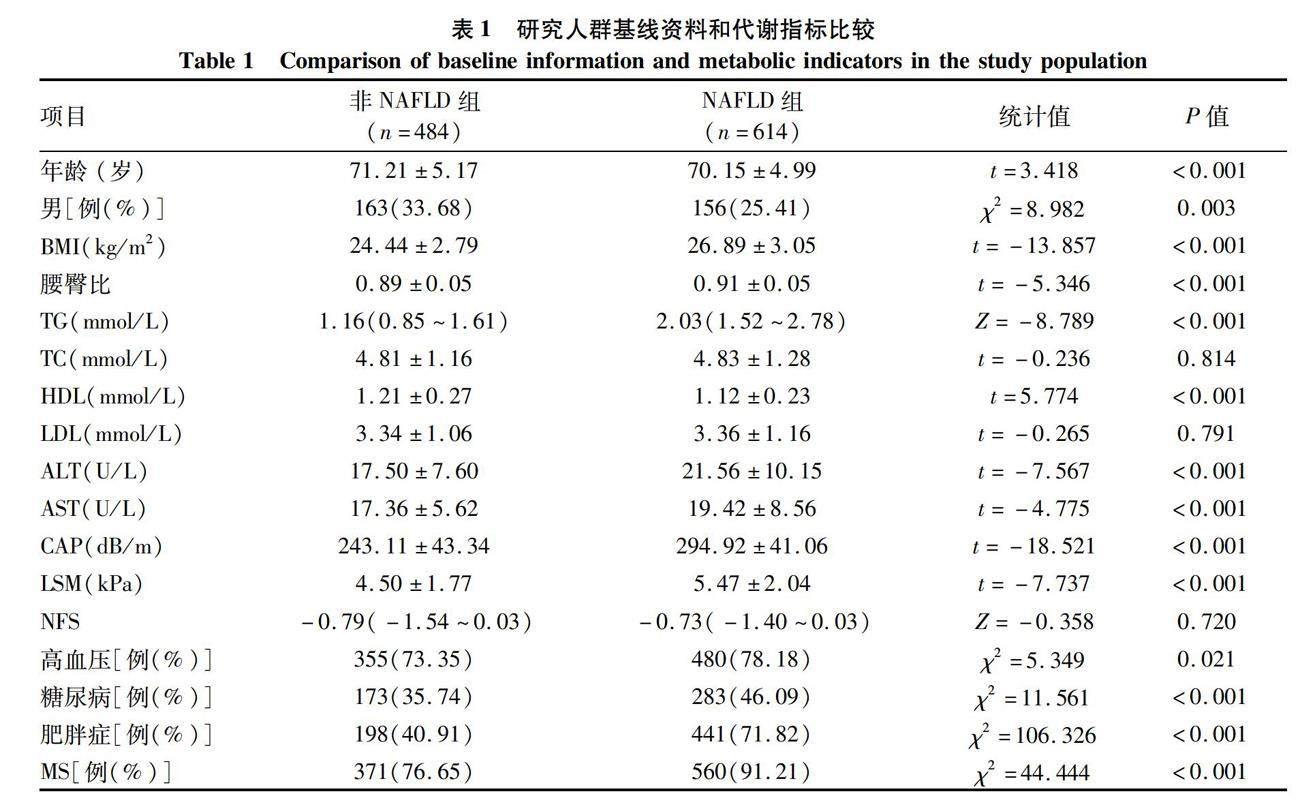
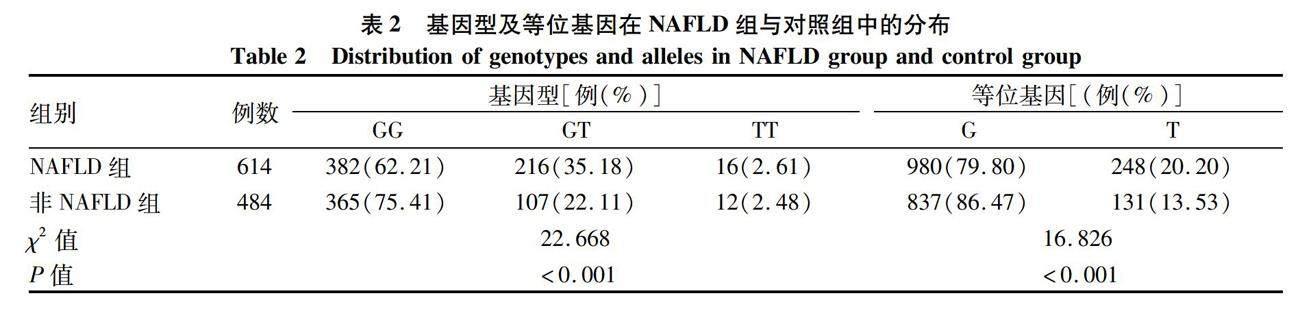
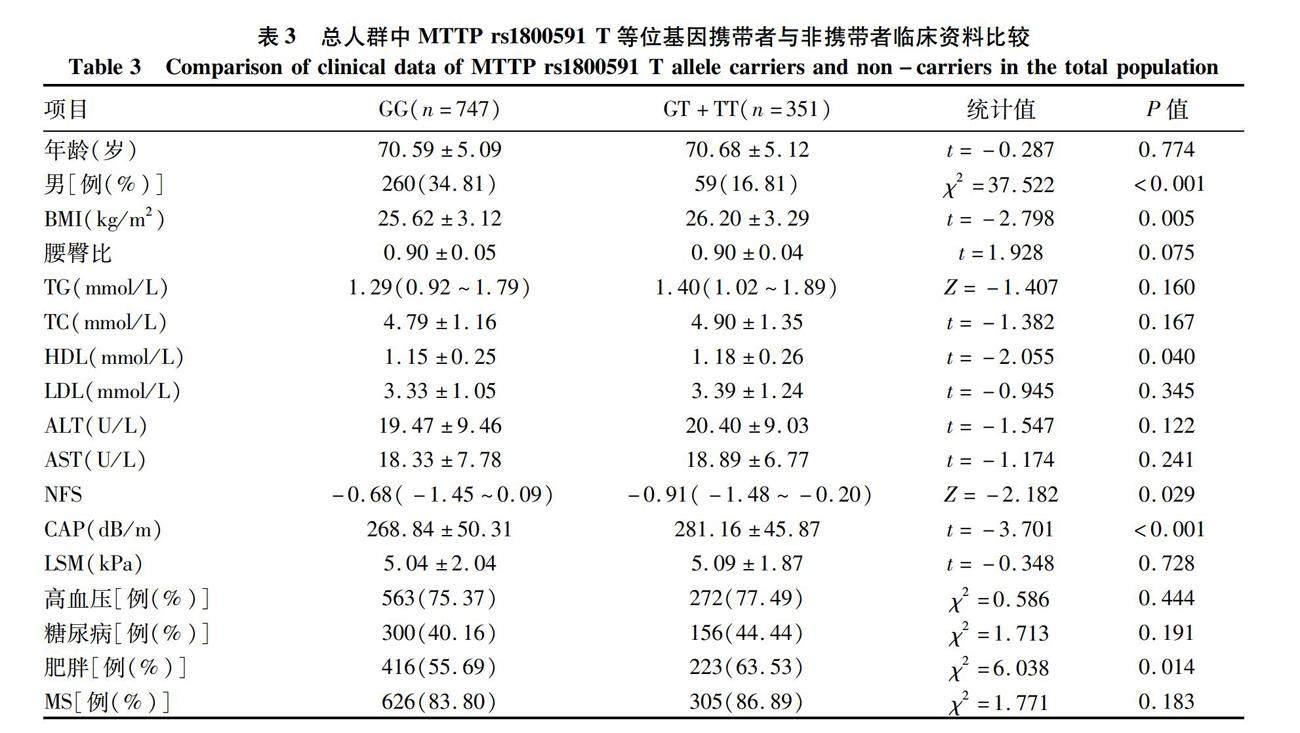
符合正態分布的計量資料兩組間比較采用獨立樣本t檢驗;對非正態分布的計量資料兩組間比較采用Mann-Whitney U檢驗;計數資料兩組間比較采用χ2檢驗。應用χ2檢驗分析基因型頻率的分布是否符合Hardy-Weinberg (H-W) 平衡檢驗以確認樣本的群體代表性。以非條件Logistic回歸模型計算比值比(OR)及其95%CI以評估基因多態性與NAFLD發生風險及其他合并癥的關系。結果 兩組間性別、年齡差異均有統計學意義(P值均<0.05)。相比于非NAFLD組,NAFLD組的BMI、腰臀比、TG、ALT、AST、CAP、LSM水平均顯著提高,而HDL明顯降低(P值均<0.05)。NAFLD組中高血壓、糖尿病、肥胖及代謝綜合征患者的比例也均高于非NAFLD組(P值均< 0.05)。MTTP rs1800591多態性在對照組基因型頻率分布符合Hardy-Weinberg平衡(χ2=1.097,P=0.29)。MTTP rs1800591不同基因型及等位基因分布在NAFLD患者與對照組中均有顯著性差異(P值均<0.001)。總人群中T等位基因(GT+TT,n=351)攜帶率在男性中比例偏低,而BMI和CAP值顯著高于非攜帶者(GG,n=747)(P值均<0.001)。相比于非攜帶者,T等位基因攜帶者(GT+TT,n=232)中肥胖患者比例明顯提高,但NFS評分卻顯著降低(P值均<0.05)。在NAFLD受試者中,T等位基因攜帶者男性比例和腰臀比顯著降低, T等位基因攜帶者HDL高于非攜帶者(GG,n=382),T等位基因攜帶者NFS評分仍明顯低于非攜帶者(P值均<0.05)。非條件Logistic回歸分析表明,在校正性別、年齡、BMI混雜因素后,MTTP rs1800591 GT+TT型仍顯著增加了NAFLD的發生風險(OR=1.643, 95%CI:1.226~2.203, P=0.001),而T等位基因攜帶則增加了總人群中肥胖的發生風險(OR=1.371, 95%CI:1.051~1.788, P=0.02)。結論 老年人群中MTTP rs1800591多態性與NAFLD的發生有關,T等位基因攜帶者可能促進了NAFLD肝臟脂肪變性,增加肥胖癥發生風險,但可能抑制了肝纖維化進展。
關鍵詞:非酒精性脂肪性肝病; 基因; 老年人
基金項目:北京市百千萬人才工程資助項目(2019A15); 北京市屬醫學科研院所公益發展改革試點項目(京醫研2021-10)
Association between the rs1800591 variation of the microsomal triglyceride transfer protein gene and the risk of nonalcoholic fatty liver disease in the elderly population
ZHAO Jinhan1, ZHANG Jing1, ZHANG Yang2, XU Xiaoyi1, GOU Yusong1, XU Hangfei1, WAN Yan3, WU Jian3. (1. Third Department of Liver Disease Center, Beijing YouAn Hospital, Capital Medical University, Beijing 100069, China; 2. Beijing Institute of Hepatology, Beijing 100069, China; 3. Capital University of Physical Education and Sports, Beijing 100191, China)
Corresponding author:
WU Jian, wujiancupes@126.com (ORCID:0000-0001-6690-4561)
Abstract:
Objective To investigate the association between the polymorphism of the microsomal triglyceride transport protein (MTTP) gene at rs1800591 locus and the risk of nonalcoholic fatty liver disease (NAFLD) in the elderly population. Methods The clinical cohort of this study was established in Menkuang Hospital, Beijing Jingmei Group General Hospital. A total of 1098 healthy elderly volunteers were recruited for physical examination in communities in Mentougou District of Beijing, China, from January 11, 2020 to September 30, 2021, among whom there were 614 patients with NAFLD and 484 individuals without NAFLD. Gene microarray was used to determine the genotypes of MTTP rs1800591; demographic data were collected, and blood biochemical parameters were measured. The independent samples t-test was used for comparison of normally distributed continuous data between groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between groups; the chi-square test was used for comparison of categorical data between groups. The chi-square test was used to investigate whether the distribution of genotype frequency was in accordance with Hardy-Weinberg equilibrium. The unconditional logistic regression model was used to calculate odds ratio (OR) and its 95% confidence interval (CI) to investigate the association of gene polymorphism with the risk of NAFLD and other comorbidities. Results There were significant differences in sex and age between the two groups (P<0.05). Compared with the non-NAFLD group, the NAFLD group had significantly higher levels of body mass index (BMI), waist-hip ratio, triglyceride, alanine aminotransferase, aspartate aminotransferase, controlled attenuation parameter (CAP), and liver stiffness measurement and a significantly lower level of high-density lipoprotein (HDL) (all P<0.05). Compared with the non-NAFLD group, the NAFLD group had a significantly higher proportion of patients with hypertension, diabetes, obesity, and metabolic syndrome (all P<0.05). The distribution of genotype frequency at MTTP rs1800591 locus was in accordance with Hardy-Weinberg equilibrium in the control group (χ2=1.097, P=0.29). There were a significant differences in the genotype and the distribution of alleles at MTTP rs1800591 locus between the patients with NAFLD and the control group (all P<0.001). In the total population, there was a significantly lower carrying rate of T allele (GT+TT, n=351) in male individuals, and the individuals carrying T allele had significantly higher BMI and CAP than those carrying GG allele (n=747) (P<0.001). Compared with the individuals who did not carry T allele, the individuals carrying T allele (GT+TT, n=232) had a significantly higher proportion of patients with obesity and a significantly lower NFS score (P<0.05). As for the individuals with NAFLD, the individuals carrying T allele had a significantly lower proportion of male individuals, a significantly lower waist-hip ratio, and a significantly higher level of HDL compared with those who did not carry T allele (GG, n=382), and the GT+TT group had a significantly lower NFS score than the GG group (all P<0.05). The non-conditional logistic regression analysis showed that after adjustment for the confounding factors of sex, age, and BMI, the GT+TT genotype at MTTP rs1800591 locus significantly increased the risk of NAFLD (OR=1.643, 95%CI: 1.226-2.203, P=0.001), and carrying T allele also increased the risk of obesity in the total population (OR=1.371, 95%CI: 1.051-1.788, P=0.02). ConclusionMTTP rs1800591 polymorphism is associated with the development of NAFLD in the elderly population, and carrying T allele may promote hepatic steatosis and increase the risk of obesity in NAFLD, while it may inhibit the progression of liver fibrosis.
Key words:
Non-alcoholic Fatty Liver Disease; Genes; Aged
Research funding:
Beijing Hundred Thousand Talents Project (2019A15); Beijing Municipal Institute of Public Medical Research Development and Reform Pilot Project (2021-10)
非酒精性脂肪性肝病(NAFLD) 是一種代謝應激性肝損傷,其全球患病率約為25%,我國目前有超過2.4億的患者[1]。NAFLD的病理進程可由單純脂肪變性進展為非酒精性脂肪性肝炎 (NASH)、纖維化、肝硬化和肝細胞癌,目前尚無有效的治療藥物[2]。此外,我國也面臨著迅速發展的老齡化問題,數據顯示[3]我國60歲及以上人口超2.64億,占全人口總數的18.7%,預計2050年將達到4.8億。在老齡化人群中,NAFLD將增加肝臟并發癥和肝外疾病發生風險,嚴重影響老年人群的生活質量,老年NAFLD患者亟需得到早期關注[4]。
NAFLD是遺傳因素和環境因素共同作用的結果,遺傳背景在其發生發展中的作用約占50%[5]。多個關鍵基因的單核苷酸多態性 (single nucleotide polymorphism, SNP)已被證明與NAFLD的遺傳易感性密切相關。近年來,基于微粒體甘油三酯轉運蛋白 (microsomal triglyceride transfer protein, MTTP)多態性 (rs1800591)與脂質代謝的密切關系,陸續開展了幾項MTTP多態性與NAFLD關系的研究,但多集中于歐美及非洲人群,對亞洲隊列的研究極少,目前尚無中國老年NAFLD人群與MTTP多態性的研究報道。
MTTP是一種異二聚體伴侶,主要在肝細胞和腸細胞中表達[6]。它是組裝和分泌極低密度脂蛋白 (very low density lipoprotein, VLDL)及乳糜微粒的關鍵酶[7],通過與載脂蛋白B (apolipoprotein B, apoB) 的特異性結合在脂蛋白生物合成中發揮重要作用[8]。研究表明,MTTP rs1800591多態性 (G>T) 可能與NAFLD的易感性相關。非洲學者Gouda等[9]在包括174例平均年齡40歲的NAFLD隊列中發現,MTTP rs1800591 TT基因型相比G等位基因攜帶者血清TG和VLDL明顯降低,歐洲Musso等[10]研究結果與此一致,表明其可引發肝臟脂代謝的異常,是NAFLD發病的重要致病因素。Namikawa等[11]對63例活檢證實的NASH日本患者進行了MTTP rs1800591多態性研究發現,G等位基因增加了NASH及肝臟脂肪變性的發生風險。與上述研究不同,在意大利[12](114例NASH) 和巴西人群[13](129例NASH) 的病例對照研究則顯示,rs1800591多態性與NAFLD、其臨床或組織學特征無顯著相關性。我國僅有一項相關研究[14]在平均年齡44歲的580例NAFLD患者中進行,結果也顯示rs1800591與NAFLD無顯著相關性。盡管大量研究提示MTTP rs1800591與NAFLD的發生發展密切相關,但仍有少數研究發現二者并無關聯,其原因可能是MTTP功能更易受到種族、地域、飲食、年齡、性別等因素的影響。為此,需要在不同種族不同年齡段的更多人群中進一步明確其易感性和風險等位基因,以及與NAFLD脂肪變性和纖維化進展的關系。
基于上述研究背景和目前我國老齡化現狀,我們以65歲以上人群為目標,建立了一個社區老年脂肪肝病的隊列,并開展了MTTP rs1800591多態性的檢測工作。探究MTTP rs1800591多態性與NAFLD之間的臨床相關性,為老年人群NAFLD綜合診治提供研究基礎。
1 資料與方法
1.1 研究對象 本研究的臨床隊列建立在北京京煤集團總醫院門礦醫院,2020年1月11日—2021年9月30日在北京門頭溝社區共招募參加健康體檢1098例老年志愿者,分為NAFLD組(n=614)和非NAFLD組(n=484)。NAFLD診斷標準符合中華醫學會肝病學分會NAFLD標準[2]。納入標準:年齡≥65歲[15];所有NAFLD患者均經B超診斷。排除標準: 有過量飲酒史和其他可以導致脂肪肝的特定疾病;患有嚴重的肝、腎、心臟和腦部疾病以及惡性腫瘤者[2]。
1.2 臨床及化驗資料 2名訓練有素的研究人員負責招募體檢患者,從社區健康記錄中提取人口統計學指標和病史。對受試者的身高、體質量、腰圍、臀圍進行標準測量,并計算BMI和腰臀比。使用FibroScan (法國Echosens公司,502 型,M探針) 對患者進行肝脂肪的定量測定,結果以受控衰減參數CAP表示,并測量肝臟硬度值(LSM)。研究對象于12 h空腹后在上午取靜脈血進行生化分析,檢測受試者的肝功能、脂質譜、空腹血漿葡萄糖(FPG)、糖化血紅蛋白等指標。
1.3 纖維化及合并癥定義 使用NAFLD纖維化評分(NAFLD fibrosis score, NFS) 來評估肝纖維化的嚴重程度。NFS=-1.675+0.037×年齡 (歲) +0.094×BMI (kg/m2)+1.13×空腹血糖受損/糖尿病 (是=1,否=0)+0.99×(AST/ALT)-0.013×PLT(×109/L)-0.66×白蛋白 (g/dL)[16]。合并癥的診斷標準如下:收縮壓≥130 mmHg或舒張壓≥85 mmHg或服用降壓藥時,診斷為高血壓[17]。Ⅱ型糖尿病診斷為:FPG≥7.0 mmol/L或口服葡萄糖耐量試驗餐后2 h血糖≥11.1 mmol/L或既往有確切糖尿病病史[18]。肥胖癥被定義為BMI≥25 kg/m2[19]。代謝綜合征 (metabolic syndrome, MS) 的標準定義[20],需至少存在以下3項或3項以上:(1)肥胖,即BMI≥25 kg/m2和/或男性腰圍>90 cm(女性腰圍>80 cm);(2)高三酰甘油血癥,即三酰甘油≥1.7 mmol/L,或患者因脂質異常而接受治療;(3)低HDL-C血癥,即男性HDL-C<1.03 mmol/L,女性HDL-C<1.29 mmol/L;(4)高血壓,即收縮壓≥130 mmHg和/或舒張壓≥85 mmHg,或患者被診斷出患有高血壓并曾接受過藥物治療;(5)高血糖,即空腹血糖升高(≥5. 6 mmol/L),或患者被診斷出患有Ⅱ型糖尿病并曾接受過藥物治療。
1.4 基因組DNA提取和基因分型 從患者全血標本中提取基因組DNA。DNA通過分光光度法 (Nanodrop 2000, Thermo Scientific, Wilmington, DE) 測定DNA的濃度和質量,并在基因分型前標準化至約50 ng/mL。MTTP rs1800591的G和T等位基因探針由美國富魯達公司設計和合成 (Fluidigm, South San Francisco, CA, USA), 使用96.96微液流動態芯片(IFC)和JunoTM系統(Fluidigm, South San Francisco, CA, USA)對隊列樣品進行SNP分型分析,采用Fluidigm SNP基因分型分析軟件(4.5.1版) 對MTTP rs1800591不同等位基因的分布進行分析。
1.5 統計學方法 數據的統計分析采用SPSS 26.0統計軟件。符合正態分布的計量資料以x±s表示,兩組間比較采用獨立樣本t檢驗;對非正態分布的計量資料,以M(P25~P75)表示,兩組間比較采用Mann-Whitney U檢驗;計數資料兩組間比較采用χ2檢驗。應用χ2檢驗分析基因型頻率的分布是否符合Hardy-Weinberg (H-W) 平衡檢驗以確認樣本的群體代表性。以非條件Logistic回歸模型計算比值比(OR)及其95%CI以評估基因多態性與NAFLD發生風險及其他合并癥的關系。P<0.05為差異有統計學意義。
2 結果
2.1 一般資料 NAFLD組共收集614例,非NAFLD組484例。兩組間性別、年齡差異均有統計學意義(P值均< 0.05)。相比于非NAFLD組,NAFLD組的BMI、腰臀比、TG、ALT、AST、CAP、LSM水平均顯著提高(P值均<0.05),而HDL明顯降低(P<0.05)。NAFLD組中高血壓、糖尿病、肥胖及MS患者的比例也均高于非NAFLD組(P值均<0.05) (表1)。
2.2 MTTP-rs1800591基因型及等位基因的分布 MTTP rs1800591多態性在對照組基因型頻率分布符合Hardy-Weinberg平衡 (χ2=1.097,P=0.29)。MTTP rs1800591不同基因型及等位基因分布在NAFLD患者與對照組中均有顯著性差異 (P值均<0.001)(表2)。
2.3 總人群中MTTP rs1800591 T等位基因攜帶者與非攜帶者臨床資料比較 為明確T等位基因對NAFLD的影響,將研究對象分為T等位基因攜帶者 (GT+TT,n=351) 及非T等位基因攜帶者 (GG,n=747) 兩組,并在兩組間進行了臨床資料比較。結果顯示,總人群中T等位基因攜帶率在男性中比例偏低,而BMI和CAP值顯著高于GG等位基因攜帶者(P值均<0.001)。進一步分析表明相比于非攜帶者,T等位基因攜帶者中肥胖患者比例明顯提高,但NFS評分卻顯著降低(P值均<0.05)(表3)。
2.4 NAFLD患者中MTTP rs1800591基因多態性的臨床資料比較 在NAFLD受試者中,T等位基因攜帶者男性比例和腰臀比顯著降低(P值均<0.05), T等位基因攜帶者HDL高于非攜帶者,T等位基因攜帶者NFS評分仍明顯低于非攜帶者(P值均<0.05)(表4)。
2.5 MTTP rs1800591 T等位基因與NAFLD及相關疾病風險分析 非條件logistic回歸分析表明,在校正性別、年齡、BMI混雜因素后,MTTP rs1800591 GT+TT型仍顯著增加了NAFLD的發生風險 (OR=1.643, 95%CI:1.226~2.203, P=0.001) (表5)。而T等位基因攜帶則增加了總人群中肥胖的發生風險 (OR=1.371, 95%CI:1.051~1.788, P=0.02),但與高血壓、糖尿病、MS的發生風險無關 (圖1)。
3 討論
NAFLD以肝臟內脂肪累積和慢性炎癥為主要表現,是一種高度異質性的疾病,其異質性來自于年齡、性別、種族、飲食、遺傳因素等[21]。其中,不同種族群體中NAFLD的患病率、臨床特征、組織學嚴重程度和預后存在顯著差異,表明遺傳因素發揮了重要作用[22]。SNP是NAFLD異質性的主要機制之一,在脂肪肝的發生發展約占50%的驅動作用[5]。MTTP是肝臟中脂質代謝的關鍵蛋白[23],在肝細胞內VLDL的組裝和分泌中發揮重要作用。MTTP在脂蛋白組裝的早期階段可以催化TG轉移到新生的ApoB,形成原始的VLDL顆粒,進而去除肝細胞內TG的聚集狀態。研究[24-26]表明,MTTP活性降低或缺失會促進肝臟脂質聚集,導致肝脂肪變性的發生。
MTTP rs1800591是近年來被證明與NAFLD發生發展密切相關的新遺傳基因SNP[27-28],其與肝脂肪變性的關系已在相關研究中得以證實。2004年,Namikawa等[11]對63例NASH患者和150例健康對照組進行MTTP rs1800591多態性研究發現,GG基因型NASH患者肝脂肪變性程度明顯高于GT基因型(無TT基因型攜帶NASH患者)。肝活檢也表明與GT基因型患者相比,GG基因型肝小葉脂肪面積更大。Bernard等[29]對217例糖尿病患者的研究中也證明,MTTP rs1800591的G等位基因可以顯著增加患者肝脂肪變性的遺傳易感性,GG基因型與GT+TT型肝臟脂肪變性比例分別為36%和17%。Gambino等[30]通過研究29例非肥胖非糖尿病NASH患者MTTP rs1800591多態性后發現,NASH人群中GG型攜帶者的TG和游離脂肪酸顯著高于其他基因型。與之相反,一項涉及意大利人群的研究[12]顯示rs1800591多態性與NAFLD、其臨床或組織學特征之間無顯著的相關性。Oliveira等[13]在巴西人群的研究也顯示,GG和GT基因型攜帶者分別在NAFLD組與對照組,以及NAFL組和NASH組比較中無明顯臨床病理差異。2014年Peng等[14]在包含580例NAFLD患者[平均年齡(46.12±12.88)歲]和580例健康對照組[平均年齡(44.86±13.55)歲] 的中國漢族人群中的研究顯示rs1800591與NAFLD無相關性。介于MTTP是血脂調節中的重要因子,其功能更易受到飲食和各種環境因素的影響,上述研究也提示MTTP rs1800591多態性在不同種族、地域和人群中,也許發揮著不同的功能。
利用當前社區老年脂肪肝病的隊列發現,GT+TT基因型攜帶者的NAFLD發病風險顯著增加,與非攜帶者相比T等位基因攜帶者CAP值顯著升高,反映了T等位基因可以增加肝臟脂肪含量。同時,無論是在總人群還是NAFLD人群中,GG等位基因型攜帶者NFS評分都顯著升高,表明GG等位基因在老年NAFLD人群中可能參與了纖維化進展。這種不同等位基因與不同脂肪肝病病理進程的相關性,可能取決于MTTP本身的功能。研究[31]表明在小鼠肝特異性敲除MTTP可以減少VLDL和ApoB-100的表達,并發展為中度脂肪肝。小鼠肝過表達MTTP會導致ApoB及VLDL的分泌增加,提高了高脂血癥的發病率[32]。而采用藥物抑制MTTP的表達,不僅會降低LDL-C和TG,也會存在胃腸道不良事件和肝臟脂肪含量增加的副作用[33]。MTTP在肝細胞內的動態平衡,在維持血脂和肝臟脂肪水平穩定上起重要作用。另外,有研究[34]表明T等位基因可以促進未成熟的VLDL顆粒酯化,從而減少VLDL到LDL的輸入,反而導致LDL-C、TC和ApoB的水平降低,進而促進肝內脂質的聚集,這可能是T等位基因增加NAFLD發病風險的原因之一。而T等位基因是脂肪肝和MS的危險因子也被其他臨床研究[35-37]所證實。此外,MTTP在胰腺和腸道等其他組織中也發揮重要的作用。Musso等[10]在NASH患者中證明相比于GT/TT基因型,GG攜帶者具有更嚴重的胰島β細胞功能障礙。Iqbal等[38]也證明在小鼠腸道內敲除MTTP,可以增加腸道內TG水平,并減少其通過乳糜微粒的運輸,這也許會進一步導致腸道菌群的紊亂,促進肝纖維化的進展。這些研究表明相比于T等位基因,G等位基因引起MTTP表達和活性降低,血脂水平持續的改變,協同其他組織的病理性變化,進而在促進肝纖維化的進展中起到主導作用。本研究是在中國北方漢族老年人群中開展,老年人常合并如糖尿病和肥胖等多種慢性疾病,NAFLD發病特征及影響因素有其自身的特點[39],這可能是在該隊列中發現G等位基因與肝纖維化密切相關的主要原因。
此外,本研究還首次對rs1800591多態性與肥胖、高血壓、糖尿病、MS等疾病的相關性進行探究,發現MTTP rs1800591多態性的GT+TT基因攜帶者肥胖癥比例明顯升高。非條件Logistic回歸在校正性別、年齡、BMI等混雜因素后仍顯示T等位基因可以增加總人群中肥胖發生的風險(OR=1.371, 95%CI:1.051~1.788),表明T等位基因攜帶可能是老年人群肥胖發生的獨立危險因素。其可能的機制有以下兩點:(1)最新研究[40]表明,在脂肪細胞中,MTTP可以與脂肪甘油三酯脂肪酶 (adipose triglyceride lipase, ATGL) 蛋白質相互作用,調節ATGL的TG水解酶活性。MTTP在小鼠脂肪細胞中特異性敲除可以提高ATGL活性,促進TG降解,抵抗飲食誘導的肥胖,而這一新功能是獨立于MTTP脂質轉移活性的。為此推測相比于T等位基因,G等位基因攜帶者脂肪組織中MTTP表達及活性減低,ATGL活性增加,進而促進脂肪降解,抵抗肥胖的發生,這可能是本研究發現T等位基因增加肥胖癥發生風險的主要原因。(2)正如前文所述,MTTP 中T等位基因可能導致循環中TC,LDL-C和ApoB水平降低[41],而低水平的ApoB已被報道[42]可以促進肥胖的發生, 這可能是另一重要機制。
本研究也存在一些不足。首先,本研究為單中心橫斷面研究,不能代表更普遍的老年群體,要進一步明確MTTP rs1800591與NAFLD發病風險的相關性還需進行更大規模的多中心前瞻性研究;其次,納入對象年齡較大,吸煙、飲酒、用藥史及既往病史等為檔案查找及患者的自我報告,存在一定回憶偏倚;鑒于本研究隊列老年人群血脂異常者居多,且服用降脂藥物情況復雜,基因多態性與血脂的相關性可靠性不強。最后,腹部超聲對輕度脂肪肝敏感性較低,結果可能存在偏倚,且不能對NAFLD脂肪變及纖維化嚴重程度進一步分級。
綜上所述,本研究報道了MTTP rs1800591多態性在老年人群中與NAFLD發病風險的相關性,具有T等位基因的個體可能增加NAFLD脂肪變性的風險,且T等位基因攜帶是老年人群肥胖癥發生的獨立危險因素。同時T等位基因攜帶者NFS評分顯著降低,可能抑制了纖維化進展。上述結果不僅首次闡明了MTTP rs1800591多態性在老年NAFLD人群中的臨床特征,為進一步的機制研究奠定了基礎,還為NAFLD患者早期篩選提供一個可靠的遺傳基因位點,促進了老年NAFLD患者的精確醫療和臨床防治的發展。
倫理學聲明:本研究方案于2020年10月26日經由首都醫科大學附屬北京佑安醫院倫理委員會審批,批號:京佑科倫意[2020]-272。所納入患者均簽署知情同意書。
利益沖突聲明:本研究不存在研究者、倫理委員會成員、受試者監護人以及與公開研究成果有關的利益沖突。
作者貢獻聲明:趙錦涵、張晶負責課題設計,資料分析,論文撰寫;張洋負責修改文章關鍵內容;徐瀟藝、勾鈺淞、徐航飛、萬妍參與收集數據,統計分析解釋;吳劍負責擬定寫作思路,指導撰寫文章及最后定稿。趙錦涵和張晶對本文貢獻等同,同為第一作者。
參考文獻:
[1]
ZHOU J, ZHOU F, WANG W, et al. Epidemiological features of NAFLD From 1999 to 2018 in China[J]. Hepatology, 2020, 71(5): 1851-1864. DOI: 10.1002/hep.31150.
[2]
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34(5): 947-957. DOI: 10.3969/j.issn.1001-5256.2018.05.007.
中華醫學會肝病學分會脂肪肝和酒精性肝病學組, 中國醫師協會脂肪性肝病專家委員會. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 臨床肝膽病雜志, 2018, 34(5): 947-957. DOI: 10.3969/j.issn.1001-5256.2018.05.007.
[3]LI J, YAO YS, DONG Q, et al. Characterization and factors associated with sleep quality among rural elderly in China[J]. Arch Gerontol Geriatr, 2013, 56(1): 237-243. DOI: 10.1016/j.archger.2012.08.002.
[4]ALQAHTANI SA, SCHATTENBERG JM. NAFLD in the elderly[J]. Clin Interv Aging, 2021, 16: 1633-1649. DOI: 10.2147/CIA.S295524.
[5]LOOMBA R, SCHORK N, CHEN CH, et al. Heritability of hepatic fibrosis and steatosis based on a prospective twin study[J]. Gastroenterology, 2015, 149(7): 1784-1793. DOI: 10.1053/j.gastro.2009.03.065
[6]PEREIRA IV, STEFANO JT, OLIVEIRA CP. Microsomal triglyceride transfer protein and nonalcoholic fatty liver disease[J]. Expert Rev Gastroenterol Hepatol, 2011, 5(2): 245-251. DOI: 10.1586/egh.11.22.
[7]WETTERAU JR, AGGERBECK LP, BOUMA ME, et al. Absence of microsomal triglyceride transfer protein in individuals with abetalipoproteinemia[J]. Science, 1992, 258(5084): 999-1001. DOI: 10.1126/science.1439810.
[8]BRADBURY P, MANN CJ, KCHL S, et al. A common binding site on the microsomal triglyceride transfer protein for apolipoprotein B and protein disulfide isomerase[J]. J Biol Chem, 1999, 274(5): 3159-3164. DOI: 10.1074/jbc.274.5.3159.
[9]GOUDA W, ASHOUR E, SHAKER Y, et al. MTP genetic variants associated with non-alcoholic fatty liver in metabolic syndrome patients[J]. Genes Dis, 2017, 4(4): 222-228. DOI: 10.1016/j.gendis.2017.09.002
[10]MUSSO G, GAMBINO R, CASSADER M. Lipoprotein metabolism mediates the association of MTP polymorphism with beta-cell dysfunction in healthy subjects and in nondiabetic normolipidemic patients with nonalcoholic steatohepatitis[J]. J Nutr Biochem, 2010, 21(9): 834-840. DOI: 10.1016/j.jnutbio.2009.06.007.
[11]NAMIKAWA C, SHU-PING Z, VYSELAAR JR, et al. Polymorphisms of microsomal triglyceride transfer protein gene and manganese superoxide dismutase gene in non-alcoholic steatohepatitis[J]. J Hepatol, 2004, 40(5): 781-786. DOI: 10.1016/j.jhep.2004.01.028.
[12]CARULLI L, CANEDI I, RONDINELLA S, et al. Genetic polymorphisms in non-alcoholic fatty liver disease: interleukin-6-174G/C polymorphism is associated with non-alcoholic steatohepatitis[J]. Dig Liver Dis, 2009, 41(11): 823-828. DOI:10.1016/j.dld.2009.03.005.
[13]OLIVEIRA CP, STEFANO JT, CAVALEIRO AM, et al. Association of polymorphisms of glutamate-cystein ligase and microsomal triglyceride transfer protein genes in non-alcoholic fatty liver disease[J]. J Gastroenterol Hepatol, 2010, 25(2): 357-361. DOI: 10.1111/j.1440-1746.2009.06001.x.
[14]PENG XE, WU YL, LU QQ, et al. MTTP polymorphisms and susceptibility to non-alcoholic fatty liver disease in a Han Chinese population[J]. Liver Int, 2014, 34(1): 118-128. DOI:? 10.1111/liv.12220.
[15]ALQAHTANI SA, SCHATTENBERG JM. NAFLD in the Elderly[J]. Clin Interv Aging, 2021, 16: 1633-1649. DOI: 10.2147/CIA.S295524.
[16]ANGULO P, HUI JM, MARCHESINI G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD[J]. Hepatology, 2007, 45(4): 846-854. DOI: 10.1002/hep.21496.
[17]WILLIAMS B, MANCIA G, SPIERING W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension[J]. J Hypertens, 2018, 36(10): 1953-2041. DOI: 10.1097/HJH.0000000000001940.
[18]Chinese Diabetes Society. Guidelines for the prevention and control of type2 diabates in China(2017 Edition)[J]. Chin J Pract Intern Med, 2018, 38(4): 292-344. DOI: 10.19538/j.nk2018040108.
中華醫學會糖尿病學分會. 中國2型糖尿病防治指南(2017年版)[J]. 中國實用內科雜志, 2018, 38(4): 292-344. DOI: 10.19538/j.nk2018040108.
[19]
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies[J]. Lancet, 2004, 363(9403): 157-163. DOI: 10.1016/S0140-6736(03)15268-3.
[20]CHITTURI S, FARRELL GC, HASHIMOTO E, et al. Non-alcoholic fatty liver disease in the Asia-Pacific region: definitions and overview of proposed guidelines[J]. J Gastroenterol Hepatol, 2007, 22(6): 778-787. DOI: 10.1111/j.1440-1746.2007.05001.x.
[21]WANG CE, XU WT, GONG J, et al. Research progress in the treatment of nonalcoholic fatty liver disease[J]. Clin J Med Offic, 2022, 50(9): 897-899,903. DOI: 10.16680/j.1671-3826.2022.09.06.
王彩娥, 許文濤, 宮建, 等. 非酒精性脂肪性肝病治療研究進展[J]. 臨床軍醫雜志, 2022, 50(9): 897-899, 903. DOI: 10.16680/j.1671-3826.2022.09.06.
[22]BROUWERS MC, van GREEVENBROEK MM, CANTOR RM. Heritability of nonalcoholic fatty liver disease[J]. Gastroenterology, 2009, 137(4): 1536. DOI: 10.1053/j.gastro.2009.03.065.
[23]HUSSAIN MM, SHI J, DREIZEN P. Microsomal triglyceride transfer protein and its role in apoB-lipoprotein assembly[J]. J Lipid Res, 2003, 44(1): 22-32. DOI: 10.1194/jlr.r200014-jlr200.
[24]KIM DH, ZHANG T, LEE S, et al. FoxO6 integrates insulin signaling with MTP for regulating VLDL production in the liver[J]. Endocrinology, 2014, 155(4): 1255-1267. DOI: 10.1210/en.2013-1856.
[25]RAABE M, VNIANT MM, SULLIVAN MA, et al. Analysis of the role of microsomal triglyceride transfer protein in the liver of tissue-specific knockout mice[J]. J Clin Invest, 1999, 103(9): 1287-1298. DOI:? 10.1172/JCI6576.
[26]ZHANG Y, XIN YN, CHENG YT, et al. The association between polymorphism rs1800591 in MTTP and non-alcoholic fatty liver disease[J/CD]. Chin J Liver Dis (Electronic Version), 2015, 7(3): 77-80. DOI: 10.3969/j.issn.1674-7380.2015.03.014.
張旸, 辛永寧, 程鈺婷, 等. MTTP基因rs1800591位點多態性與非酒精性脂肪性肝病的相關性研究[J/CD]. 中國肝臟病雜志(電子版), 2015, 7(3): 77-80. DOI:?? 10.3969/j.issn.1674-7380.2015.03.014.
[27]LI L, WANG SJ, SHI K, et al. Correlation between MTP -493G>T polymorphism and non-alcoholic fatty liver disease risk: a meta-analysis[J]. Genet Mol Res, 2014, 13(4): 10150-10161. DOI: 10.4238/2014.
[28]TAN J, ZHANG J, ZHAO Z, et al. The association between SNPs rs1800591 and rs3816873 of the MTTP gene and nonalcoholic fatty liver disease: A meta-analysis[J]. Saudi J Gastroenterol, 2020, 26(4): 171-178. DOI: 10.4103/sjg.SJG_201_20.
[29]BERNARD S, TOUZET S, PERSONNE I, et al. Association between microsomal triglyceride transfer protein gene polymorphism and the biological features of liver steatosis in patients with type II diabetes[J]. Diabetologia, 2000, 43(8): 995-999. DOI: 10.1007/s001250051481.
[30]GAMBINO R, CASSADER M, PAGANO G, et al. Polymorphism in microsomal triglyceride transfer protein: a link between liver disease and atherogenic postprandial lipid profile in NASH?[J]. Hepatology, 2007, 45(5): 1097-1107. DOI: 10.1002/hep.21631.
[31]RAABE M, VNIANT MM, SULLIVAN MA, et al. Analysis of the role of microsomal triglyceride transfer protein in the liver of tissue-specific knockout mice[J]. J Clin Invest, 1999, 103(9): 1287-1298. DOI: 10.1172/JCI6576.
[32]TIETGE UJ, BAKILLAH A, MAUGEAIS C, et al. Hepatic overexpression of microsomal triglyceride transfer protein (MTP) results in increased in vivo secretion of VLDL triglycerides and apolipoprotein B[J]. J Lipid Res, 1999, 40(11): 2134-2139.
[33]CUCHEL M, RADER DJ. Microsomal transfer protein inhibition in humans[J]. Curr Opin Lipidol, 2013, 24(3): 246-250. DOI: 10.1097/MOL.0b013e32836139df.
[34]GARCA-GARCA AB, GONZLEZ C, REAL JT, et al. Influence of microsomal triglyceride transfer protein promoter polymorphism-493 GT on fasting plasma triglyceride values and interaction with treatment response to atorvastatin in subjects with heterozygous familial hypercholesterolaemia[J]. Pharmacogenet Genomics, 2005, 15(4): 211-218. DOI: 10.1097/01213011-200504000-00004.
[35]GOUDA W, ASHOUR E, SHAKER Y, et al. MTP genetic variants associated with non-alcoholic fatty liver in metabolic syndrome patients[J]. Genes Dis, 2017, 4(4): 222-228. DOI: 10.1016/j.gendis.2017.09.002.
[36]ZK A, JCHYMOV M, TVRZICK E, et al. The influence of polymorphism of -493G/T MTP gene promoter and metabolic syndrome on lipids, fatty acids and oxidative stress[J]. J Nutr Biochem, 2008, 19(9): 634-641. DOI: 10.1016/j.jnutbio.2007.09.001.
[37]KARPE F, LUNDAHL B, EHRENBORG E, et al. A common functional polymorphism in the promoter region of the microsomal triglyceride transfer protein gene influences plasma LDL levels[J]. Arterioscler Thromb Vasc Biol, 1998, 18(5): 756-761. DOI: 10.1161/01.atv.18.5.756.
[38]IQBAL J, BOUTJDIR M, RUDEL LL, et al. Intestine-specific MTP and global ACAT2 deficiency lowers acute cholesterol absorption with chylomicrons and HDLs[J]. J Lipid Res, 2014, 55(11): 2261-2275. DOI: 10.1194/jlr.M047951.
[39]YIN HJ, LI XL, XU C, et al. Clinical characteristics and influencing factors of non-alcoholic fatty liver disease in the elderly at a district in Beijing[J]. Chin J Mult Organ Dis Elderly, 2022, 21(9): 651-654. DOI:? 10.11915 /j.issn.1671-5403.2022.09.141.
尹慧君, 李曉利, 徐成, 等. 北京某地區老年人群非酒精性脂肪性肝病的臨床特征及影響因素[J]. 中華老年多器官疾病雜志, 2022, 21(9): 651-654. DOI:? 10.11915 /j.issn.1671-5403.2022.09.141.
[40]RAJAN S, HOFER P, CHRISTIANO A, et al. Microsomal triglyceride transfer protein regulates intracellular lipolysis in adipocytes independent of its lipid transfer activity[J]. Metabolism, 2022, 137: 155331. DOI: 10.1016/j.metabol.2022.155331.
[41]GARCA-GARCA AB, GONZLEZ C, REAL JT, et al. Influence of microsomal triglyceride transfer protein promoter polymorphism -493 GT on fasting plasma triglyceride values and interaction with treatment response to atorvastatin in subjects with heterozygous familial hypercholesterolaemia[J]. Pharmacogenet Genomics, 2005, 15(4): 211-218. DOI: 10.1097/01213011-200504000-00004.
[42]di FILIPPO M, MOULIN P, ROY P, et al. Homozygous MTTP and APOB mutations may lead to hepatic steatosis and fibrosis despite metabolic differences in congenital hypocholesterolemia[J]. J Hepatol, 2014, 61(4): 891-902. DOI: 10.1016/j.jhep.2014.05.023.
收稿日期:
2022-11-18;錄用日期:2023-01-06
本文編輯:林姣