腹腔鏡和開腹膽囊切除術治療門靜脈高壓癥合并膽囊結石的效果比較
趙 斌, 卿小松, 賴 釗
(自貢市第四人民醫院 肝膽外科, 四川自貢 643000)
腹腔鏡和開腹膽囊切除術治療門靜脈高壓癥合并膽囊結石的效果比較
趙 斌, 卿小松, 賴 釗
(自貢市第四人民醫院 肝膽外科, 四川自貢 643000)
目的 探討腹腔鏡膽囊切除術(LC)治療門靜脈高壓癥合并膽囊結石的安全性和可行性。方法 回顧性分析自貢市第四人民醫院2012年1月-2016年6月收治的96例行手術治療的門靜脈高壓癥合并癥狀性膽囊結石患者的臨床資料,其中50例行LC(腹腔鏡組),46例行開腹膽囊切除術(開腹組)。比較2組患者手術相關情況及術后肝功能的變化。多組間比較采用重復測量資料的方差分析,進一步兩兩比較采用LSD-t檢驗;2組間比較采用t檢驗。計數資料組間比較采用χ2檢驗。結果 2組患者均無圍手術期死亡病例,腹腔鏡組無中轉開腹病例。腹腔鏡組的手術時間、術中出血量、住院時間、住院費用和術后并發癥發生率均低于開腹組(t值分別為2.075、7.389、4.839、3.809;χ2=4.697,P值均<0.05)。2組患者血清ALT、AST、TBil和Alb水平術后1d均升高或下降,術后3、7d逐漸恢復術前水平。除腹腔鏡組的TBil之外,其余組內比較差異均有統計學意義(F值分別為201.85、597.84、185.55、373.10、5.617、4.570、10.429,P值均<0.01)。腹腔鏡組術后1 d和開腹組術后1、3 d血清ALT、AST水平均顯著高于同組術前水平(P值均<0.05),且腹腔鏡組術后1、3 d血清ALT和AST水平均明顯低于開腹組(t值分別為12.537、18.370、9.548、15.118,P值均<0.01)。開腹組術后1 d血清TBil水平高于術前(P<0.05)和腹腔鏡組術后1 d水平(t=2.547,P=0.013)。腹腔鏡術后1 d和開腹組術后1、3 d血清Alb水平均低于同組術前水平(P值均<0.05),且腹腔鏡組術后1 d血清Alb水平明顯高于開腹組(t=2.291,P=0.024)。結論 LC治療門靜脈高壓癥合并膽囊結石是安全可行的,而且較開腹手術而言,有明顯的微創優勢,對肝功能的損傷較小。
膽囊結石病; 高血壓, 門靜脈; 膽囊切除術, 腹腔鏡; 對比研究
肝硬化患者由于凝血功能和肝功能較差,且術中及術后易出現腹腔內大出血和肝衰竭等嚴重并發癥,一度是腹腔鏡膽囊切除術(LC)的絕對或相對禁忌證[1]。近年來,隨著圍手術期管理的優化、手術技術的進步和外科理念的更新,LC治療肝硬化合并膽囊結石的可行性和安全性得到了論證,并沒有增加手術相關并發癥和圍手術期死亡的發生率[2-3]。但是,關于腹腔鏡治療門靜脈高壓癥合并膽囊結石的報道仍較少,其手術療效和安全性仍存在一定的爭議。本研究比較LC和開腹膽囊切除術(OC)治療門靜脈高壓癥合并膽囊結石的效果,以指導臨床。
1 資料與方法
1.1 研究對象 選取本院2012年1月-2016年6月收治的96例行手術治療的門靜脈高壓癥合并癥狀性膽囊結石的患者。所有患者均有急、慢性膽囊炎的臨床表現,術前均行影像學檢查證實存在膽囊結石,且合并有門靜脈高壓癥的征象。根據患者及家屬的意愿選擇術式,術前均簽署手術知情同意書和手術方式選擇書。其中50例行LC(腹腔鏡組),46例行OC(開腹組)。1.2 治療方法 入院后積極予以護肝、糾正凝血功能障礙和低蛋白血癥等治療,將術前Child-Pugh分級維持在A級或B級。(1)腹腔鏡組:采用全麻-氣管插管,頭高腳低左側傾斜30°體位,三孔法操作。建立氣腹后,常規探查腹腔,解剖膽囊三角,分離和結扎膽囊動脈和膽囊頸管,順行或逆行切除膽囊。根據術中創面情況,選擇性于膽囊床處放置腹腔引流管。(2)開腹組:采用全麻-氣管插管,仰臥位,肋緣下切口,余手術步驟同腹腔鏡組。術后密切觀察患者生命體征、有無腹腔內出血和肝功能變化。
1.3 觀察指標 (1)手術相關情況:手術時間、術中出血量、引流管放置、住院時間、住院費用、術后并發癥(術后30 d內發生的并發癥)發生率。(2)肝功能指標:術前及術后1、3、7 d的ALT、AST、Alb和TBil。

2 結果
2.1 一般資料 96例患者中男68例,女28例;年齡46~72歲,平均(55.4±11.2)歲;肝功能Child-Pugh A級55例,B級41例;脾大、脾功能亢進癥75例,腹水29例,食管胃底靜脈曲張42例;乙型肝炎肝硬化76例,丙型肝炎肝硬化14例,酒精性肝硬化6例。2組患者一般資料比較差異均無統計學意義(P值均>0.05)(表1)。
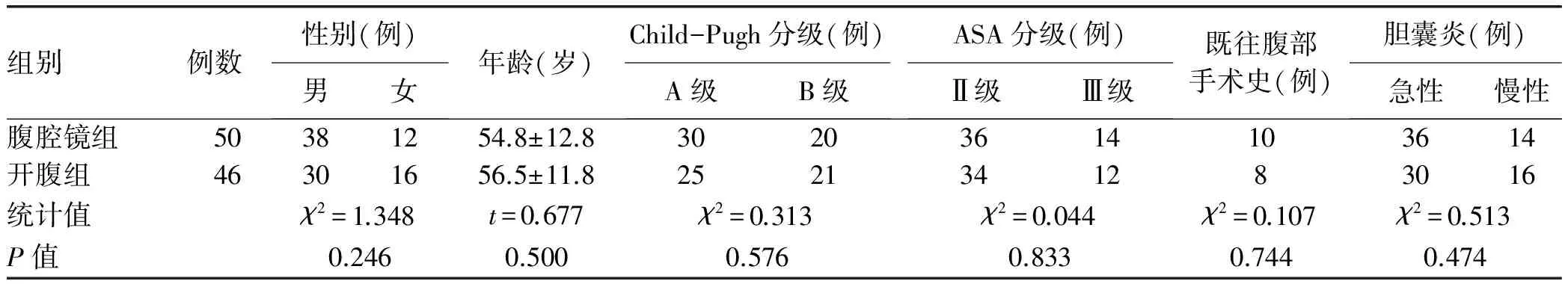
表1 2組患者的一般資料比較
注:ASA分級,美國麻醉醫師協會手術風險分級
2.2 手術相關情況 2組患者手術均順利,無圍手術期死亡病例,腹腔鏡組無中轉開腹病例。腹腔鏡組的手術時間、術中出血量、住院時間、住院費用和術后并發癥發生率均低于開腹組,且差異均有統計學意義(P值均<0.05)(表2)。
2.3 術后肝功能的變化 2組患者血清ALT、AST和TBil水平術后1 d均升高,術后3、7 d逐漸下降,除腹腔鏡組的TBil之外,其余組內比較差異均有統計學意義(P值均<0.01)。腹腔鏡組術后1 d和開腹組術后1、3 d血清ALT、AST水平與同組術前水平比較,差異均有統計學意義(P值均<0.05),且腹腔鏡組術后1、3 d血清ALT和AST水平均明顯低于開腹組(t值分別為12.537、18.370、9.548、15.118,P值均<0.01)。開腹組術后1 d血清TBil水平高于腹腔鏡組,差異有統計學意義(t=2.547,P=0.013)。2組患者血清Alb水平術后1 d均下降,術后3、7 d逐漸升高,組內比較差異有統計學意義(P值均<0.01)。腹腔鏡組術后1 d和開腹組術后1、3 d血清Alb水平較同組術前比較,差異均有統計學意義(P值均<0.05),且腹腔鏡組術后1 d血清Alb水平明顯高于開腹組(t=2.291,P=0.024)(表3)。
3 討論
膽囊結石是肝硬化患者常見的合并癥之一,其發病率較普通患者高。約30%的肝硬化患者合并膽囊結石,至少是非肝硬化患者的2倍[4]。至于肝硬化增加膽囊結石發病率的具體機制尚不清楚,可能與雌激素升高、繼發于脾亢的慢性溶血、肝臟合成及分泌的膽鹽和非結合膽紅素減少、膽囊餐后再填充功能受損[5]等因素有關。盡管目前沒有文獻統計門靜脈高壓癥合并膽囊結石的發病率,但有研究[6]表明合并腹水、門靜脈高壓癥的失代償期肝硬化患者膽囊結石的發病率是代償期肝硬化患者的2~3倍。大多數門靜脈高壓癥合并膽囊結石患者是無癥狀的,可以密切隨訪。對于癥狀性膽囊結石,反復發作不僅影響生活質量,而且可能會繼發膽總管結石使肝功能受到進一步損傷,手術切除仍是其首選的治療方式。但是由于門靜脈高壓導致十二指腸韌帶、膽囊三角區尤其膽囊床靜脈曲張,再加上凝血功能障礙,使得手術難度和風險加大,術后并發癥發生率和病死率均較高[7]。LC具有明顯的微創優勢,但是術者術中缺乏觸感,止血操作可能差于開腹手術,故其是否適用于門靜脈高壓癥合并膽囊結石患者仍存在一定的爭議。對于Child-Pugh C級的患者,手術治療后并發癥發生率和病死率較高,原則上應盡量避免手術治療[1],故本研究只納入了Child-Pugh A級或B級的患者。
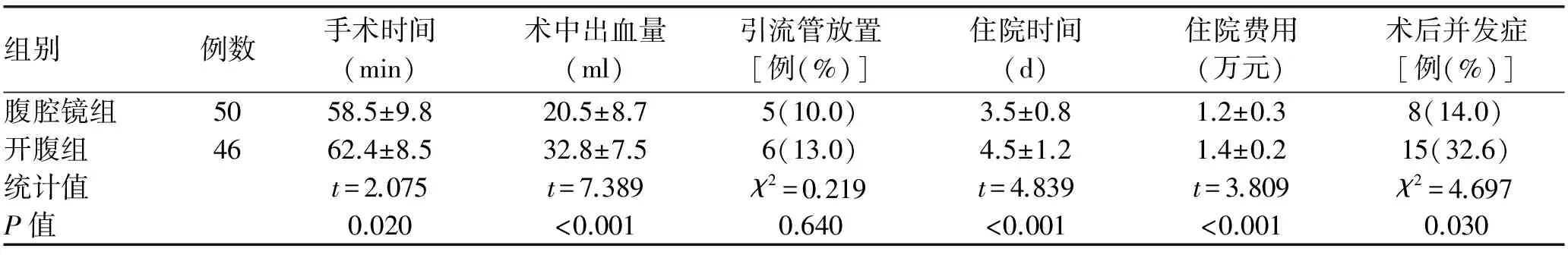
表2 2組患者手術相關情況的比較

表3 2組患者肝功能的比較
本研究比較了2組患者的手術相關情況,腹腔鏡組的手術時間、術中出血量、住院時間和住院費用均明顯低于開腹組,且腹腔鏡組無中轉開腹病例。這些數據體現了LC治療門靜脈高壓癥合并膽囊結石的可行性和安全性,且較開腹手術而言,其具有明顯的微創優勢。LC對患者的應激和免疫系統影響較小,而且其可以局部放大手術視野,更有利于手術操作的精細性,避免損傷曲張的靜脈叢[8]。近年來,3D腹腔鏡出現更進一步的增強了手術視野的清晰度[9-10]。開腹手術切口較大,破壞了腹膜的完整性,術后可能并發切口出血、腹水增多、腹部感染,甚至引發敗血癥,病死率較高,而腹腔鏡手術可以減少這些并發癥的發生。本研究中腹腔鏡組術后并發癥的發生率要低于開腹組,差異有統計學意義,但腹腔鏡組術后并發癥的發生率仍較高。這也佐證了門靜脈高壓癥合并膽囊結石患者行膽囊切除術的手術風險較大。腹腔鏡組術后并發癥主要以腹腔積液、Trocar孔出血和膽囊床滲血為主。腹腔積液與門靜脈壓力增高、低蛋白血癥等有關,術前及術后均應糾正低蛋白血癥,注意控制補液量,盡量縮短手術時間。筆者術中使用超聲刀進行分離,可有效地減少出血量[11]。術后2例膽囊床滲血的病例也均經保守治療后好轉。縫合Trocar孔時要注意縫合腹膜,以在鏡頭直視下進行操作,以減少Trocar孔出血的幾率。
對2組患者術后肝功能的變化進行比較,發現2種手術方式對肝功能均有一定的損傷,2組患者術后第1天 ALT、AST、TBil和Alb均有一定惡化,但是腹腔鏡組的惡化程度低于開腹組。而且腹腔鏡組4個指標在術后第3、7天均慢慢恢復正常,但開腹組術后第3天的ALT、AST和Alb均明顯高于或低于術前。這也說明了較開腹手術,LC對患者肝功能的損傷程度較小,也是其可以減少術后并發癥發生的原因之一。
綜上所述,LC治療門靜脈高壓癥合并膽囊結石是安全可行的,而且較開腹手術而言,均有明顯的微創優勢,對肝功能的損傷較小。但無論是LC還是OC,術后并發癥的發生率均較高,術者應注意把握手術適應證和優化圍手術期處理。
[1] McGILLICUDDY JW, VILLAR JJ, ROHAN VS, et al. Is cirrhosis a contraindication to laparoscopic cholecystectomy?[J]. Am Surg, 2015, 81(1): 52-55.
[2] LAURENCE JM, TRAN PD, RICHARDSON AJ, et al. Laparoscopic or open cholecystectomy in cirrhosis: a systematic review of outcomes and meta-analysis of randomized trials[J]. HPB (Oxford), 2012, 14(3): 153-161.
[3] de GOEDE B, KLITSIE PJ, HAGEN SM, et al. Meta-analysis of laparoscopic versus open cholecystectomy for patients with liver cirrhosis and symptomatic cholecystolithiasis[J]. Br J Surg, 2013, 100(2): 209-216.
[4] GUI L, LIU Y, LUO M. Surgical management of cholecystolithiasis combination with cirrhotic portal hypertension[J]. J Hepatopancreatobiliary Surg, 2016, 28(2): 162-165. (in Chinese) 桂亮, 劉曄, 羅蒙. 膽囊結石伴肝硬化門靜脈高壓癥的外科處理進展[J]. 肝膽胰外科雜志, 2016, 28(2): 162-165.
[5] ZHANG LL. Pathological changes and pathogenesis of gallbladder stones associated with liver cirrhosis[J]. Chin J Gen Surg, 2016, 25(2): 276-280. (in Chinese) 張亮亮. 肝硬化并膽囊結石的病理改變與發病機制[J]. 中國普通外科雜志, 2016, 25(2): 276-280.
[6] STEINBERG HV, BECKETT WW, CHEZMAR JL, et al. Incidence of cholelithiasis among patients with cirrhosis and portal hypertension[J]. Gastrointest Radiol, 1988, 13(4): 347-350.
[7] BAI MD, WANG J, XU H, et al. A prospective study on cholecystectomy for symptomatic benign gallbladder disease in cirrhotic patients[J]. Chin J Gen Surg, 2012, 27(4): 306-309.(in Chinese) 白明東, 王建, 徐海, 等. 癥狀性膽囊良性病變合并肝硬化的手術治療:一項前瞻性隨機研究[J]. 中華普通外科雜志, 2012, 27(4): 306-309.
[8] KONG XY, LI MJ, ZHENG Z, et al. Clinical efficacy of laparoscopic cholecystectomy for the treatment of cholecystolithiasis combined with liver cirrhosis and portal hypertension[J]. Chin J Dig Surg, 2014, 13(9): 734-735. (in Chinese) 孔曉宇, 李明杰, 鄭直, 等. 腹腔鏡膽囊切除術治療膽囊結石合并肝硬化門靜脈高壓癥的臨床療效[J]. 中華消化外科雜志, 2014, 13(9): 734-735.
[9] BILGEN K, USTUN M, KARAKAHYA M, et al. Comparison of 3D imaging and 2D imaging for performance time of laparoscopic cholecystectomy[J]. Surg Laparosc Endosc Percutan Tech, 2013, 23(2): 180-183.
[10] ZHENG MH. Review on the development of minimally invasive surgery[J]. Chin J Dig Surg, 2015, 14(1): 17-18. (in Chinese) 鄭民華. 微創外科發展回眸[J]. 中華消化外科雜志, 2015, 14(1): 17-18.
[11] HE XD, YANG Y, CUI Q, et al. Effects of ultracision-harmonic scalpel and electro scalpel used in laparoscopic cholecystectomy on C-reactive protein[J]. Clin J Med Offic, 2015, 43(3): 240-242. (in Chinese) 何效東, 楊毅, 崔泉, 等. 腹腔鏡膽囊切除術中超聲刀和高頻電刀對患者血漿CRP水平的影響[J]. 臨床軍醫雜志,2015, 43(3): 240-242.
引證本文:ZHAO B, QING XS, LAI Z. Clinical effect of laparoscopic versus open cholecystectomy in treatment of patients with portal hypertension complicated by gallstones[J]. J Clin Hepatol, 2017, 33(5): 888-891. (in Chinese) 趙斌, 卿小松, 賴釗. 腹腔鏡和開腹膽囊切除術治療門靜脈高壓癥合并膽囊結石的效果比較[J]. 臨床肝膽病雜志, 2017, 33(5): 888-891.
(本文編輯:王 瑩)
Clinical effect of laparoscopic versus open cholecystectomy in treatment of patients with portal hypertension complicated by gallstones
ZHAOBin,QINGXiaosong,LAIZhao.
(DepartmentofHepatobiliarySurgery,TheFourthPeople′sHospitalofZigong,Zigong,Sichuan643000,China)
Objective To investigate the safety and feasibility of laparoscopic cholecystectomy (LC) in the treatment of portal hypertension complicated by gallstones. Methods A retrospective analysis was performed for the clinical data of 96 patients with portal hypertension complicated by gallstones who underwent surgical treatment in The Fourth People′s Hospital of Zigong from January 2012 to June 2016. These patients were divided into laparoscopic group with 50 patients who underwent LC and open group with 46 patients who underwent open cholecystectomy. The surgical conditions and changes in liver function after surgery were compared between the two groups. An analysis of variance with repeated measures was used for comparison of continuous data between multiple groups, and the least significant differencet-test was used for comparison between two groups; thet-test was used for comparison between two groups. The chi-square test was used for comparison of categorical data between groups. Results No deaths occurred during the perioperative period and no patient was converted to open surgery in the laparoscopic group. Compared with the open group, the laparoscopic group had significantly lower time of operation, intraoperative blood loss, length of hospital stay, hospital costs, and incidence rate of postoperative complications (t=2.075, 7.389, 4.839, and 3.809,χ2=4.697, allP<0.05). Both groups had increased or reduced serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TBil), and albumin (Alb) at 1 day after surgery, which gradually returned to preoperative levels at 3 or 7 day after surgery. The laparoscopic group had significant changes in the serum levels of ALT, AST, and Alb (F=201.85, 185.55, and 4.570, allP<0.01), while the open group had significant changes in the serum levels of ALT, AST, TBil, and Alb (F=597.84, 373.10, 5.617, and 10.429, allP<0.01). There were significant increases in the serum levels of ALT and AST 1 day after surgery in the laparoscopic group and at 1 and 3 days after surgery in the open group (allP<0.05), and at 1 and 3 days after surgery, the laparoscopic group had significantly lower serum levels of ALT and AST than the open group (t=12.537, 18.370, 9.548 and 15.118, bothP<0.01). At 1 day after surgery, the open group had a significant increase in the serum level of TBil (P<0.05) and a higher serum level of TBil than the laparoscopic group (t=2.547,P=0.013). There were significant reductions in the serum level of Alb at 1 day after surgery in the laparoscopic group and at 1 and 3 days after surgery in the open groups (allP<0.05), and at 1 day after surgery, the laparoscopic group had a significantly higher serum level of Alb than the open group (t=2.291,P=0.024). Conclusion LC is safe and feasible in the treatment of portal hypertension complicated by gallstones, and compared with open cholecystectomy, it has the advantages of a minimally invasive surgery and causes less liver damage.
cholecystolithiasis; hypertension, portal; cholecystectomy,laparoscopic; comparative study
10.3969/j.issn.1001-5256.2017.05.019
2016-11-18;
2016-12-08。
趙斌(1967-),男,副主任醫師,主要從事肝膽外科疾病的研究。
R657.34; R657.42
A
1001-5256(2017)05-0888-04