高脂血癥性與膽源性急性胰腺炎患者血脂、血淀粉酶、尿淀粉酶水平的比較
董永春
成都軍區機關醫院消化科,四川 成都 610011
高脂血癥性與膽源性急性胰腺炎患者血脂、血淀粉酶、尿淀粉酶水平的比較
董永春
成都軍區機關醫院消化科,四川 成都 610011
目的 比較高脂血癥性急性胰腺炎(hyperlipidemic acute pancreatitis, HLAP)與膽源性急性胰腺炎(biliary acute pancreatitis, BAP)患者的血脂、血淀粉酶(amylase, AMY)和尿淀粉酶(urine amylase, UAMY)含量水平。方法 選取2014年8月-2016年8月在成都軍區機關醫院就診的急性胰腺炎(acute pancreatitis, AP)患者218例,其中HLAP患者117例,BAP患者101例,分析兩組患者血脂、AMY、UAMY、血葡萄糖(Glu)、乳酸脫氫酶(LDH)、血紅細胞壓積(HCT)、C反應蛋白(CRP)、治療及預后的情況。結果 HLAP組的甘油三酯(TG)、總膽固醇(TC)、高密度脂蛋白(HDL-C)、低密度脂蛋白(LDH-C)、平均載脂蛋白A(Apo-A)和平均載脂蛋白B(Apo-B)含量水平均高于BAP組,兩組之間比較,差異有統計學意義(P<0.05)。HLAP組的AMY、UAMY和LDH含量水平低于BAP組,HLAP組的Glu、HCT和CRP含量水平高于BAP組,兩組之間比較,差異有顯著統計學意義(P<0.01)。HLAP組的復發、手術治療和病死例數高于BAP組,兩組之間比較,差異有統計學意義(P<0.05)。結論 HLAP患者的糖脂質含量水平高于BAP患者,AMY和UAMY含量水平低于BAP患者。
高脂血癥性急性胰腺炎;膽源性急性胰腺炎;血淀粉酶;尿淀粉酶
急性胰腺炎(acute pancreatitis, AP)臨床上屬于常見病,發生該疾病的原因有酒精、高脂血癥、飲食、內分泌、腹部創傷、遺傳等,在我國比較多見的發病原因是膽道疾病[1]。發生膽源性急性胰腺炎(biliary acute pancreatitis, BAP)概率最高,超過1/2的AP是因為膽道疾病如膽結石、膽道蛔蟲等引起的,發生AP的時候發展較快且急,有時候病情非常危險,病死率為6%~12%[2]。經常發作AP的患者大多數并發高脂血癥,特別是升高非常明顯的甘油三脂(TG),當血清濃度>11.3 mmol/L時發生AP的概率非常高,多年的研究證明高脂血癥是發生AP的主要原因之一,稱為高脂血癥性急性胰腺炎(hyperlipidemic acute pancreatitis, HLAP)[3-4]。然而,脂質、血淀粉酶(amylase, AMY)和尿淀粉酶(urine amylase, UAMY)在HLAP與BAP患者的含量水平并不清楚。因此,本文主要對HLAP與BAP患者的糖脂質、AMY和UAMY含量水平進行比較,為臨床治療提供參考。
1 資料與方法
1.1 一般資料 選取2014年8月-2016年8月在成都軍區機關醫院就診的AP患者218例,其中HLAP患者117例,男76例,女41例,年齡(40.91±9.54)歲;BAP患者101例,男45例,女56例,年齡(46.17±14.38)歲;男女比例、年齡在兩組間比較,差異無統計學意義(P>0.05),具有可比性。
1.2 納入及排除標準 納入標準:參照2014版急性胰腺炎診治指南進行診斷,HLAP診斷標準:具有AP的臨床和影像學表現,入院時血TG>11.3 mmol/L或AP并靜脈乳糜狀血患者;BAP診斷標準:符合AP的臨床診斷指標,根據B超、CT、MRCP或ERCP等影像學檢查提示膽管、膽囊結石等疾病。排除標準:發病48 h內入院后未進行血脂檢測,伴有結石、蛔蟲等膽系疾病的HLAP患者。
1.3 研究方法 采集患者早晨空腹血液,提取血清進行檢測。所有患者入院后均按照我國急性胰腺炎診治指南進行規范化治療,非手術治療:包括禁食、胃腸減壓、解痙、止痛、抑酸和胰酶抑制、液體復蘇、保護器官功能、營養支持、抗炎等治療;手術治療:外科治療主要針對胰腺局部并發癥繼發感染或產生壓迫癥狀,如消化道梗阻、膽道梗阻、胰瘺等。
1.4 研究指標 分析兩組患者血脂、AMY、UAMY、血葡萄糖(Glu)、乳酸脫氫酶(LDH)、血紅細胞壓積(HCT)、C反應蛋白(CRP)、治療及預后的情況。
1.5 質量控制 所有患者樣品均重復檢測3次,取平均值。

2 結果
2.1 兩組患者的血脂水平比較 結果顯示,HLAP組中的TG、TC、Apo-B含量顯著高于BAP組,差異有統計學意義(P<0.01)。HLAP組中的HDL-C、LDH-C、Apo-A含量高于BAP組,兩組之間比較,差異有統計學意義(P<0.05,見表1)。


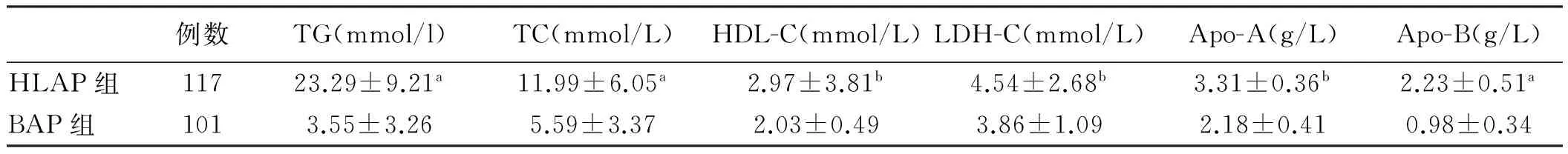
例數TG(mmol/l)TC(mmol/L)HDL-C(mmol/L)LDH-C(mmol/L)Apo-A(g/L)Apo-B(g/L)HLAP組11723.29±9.21a11.99±6.05a2.97±3.81b4.54±2.68b3.31±0.36b2.23±0.51aBAP組1013.55±3.265.59±3.372.03±0.493.86±1.092.18±0.410.98±0.34
注:與BAP組比較,aP<0.01,bP<0.05。
2.2 兩組患者的生化指標比較 結果顯示,HLAP組中的AMY、UAMY、LDH含量顯著低于BAP組,差異有統計學意義(P<0.01);HLAP組中的Glu、HCT、CRP含量顯著高于BAP組,兩組之間比較,差異有顯著統計學意義(P<0.01,見表2)。



例數AMY(U/L)UAMY(U/L)Glu(mmol/L)LDH(U/L)HCT(%)CRP(mg/L)HLAP組117221.56±199.36a1416.24±1384.38a12.48±7.98a767.23±324.52a74.28±5.99a119.98±55.35aBAP組1011496.14±1259.423963.47±3559.277.72±2.841291.96±687.8552.79±6.3271.39±57.98
注:與BAP組比較,aP<0.01。
2.3 兩組患者的治療及預后分析 兩組患者入院后均給予非手術治療,經非手術治療無效或病情急劇進展、胰腺局部并發癥繼發感染或產生壓迫癥狀時,及時給予外科手術干預治療。通過對兩組患者的治療及預后比較分析,結果顯示,HLAP組的復發病例數高于BAP組,HLAP組的手術治療例數高于BAP組,HLAP組的病死例數高于BAP組,兩組之間比較,差異有統計學意義(P<0.05,見表3)。
表3 兩組患者的治療及預后比較[例數(%)]
Tab 3 Comparison of treatment and prognosis between two groups [n(%)]
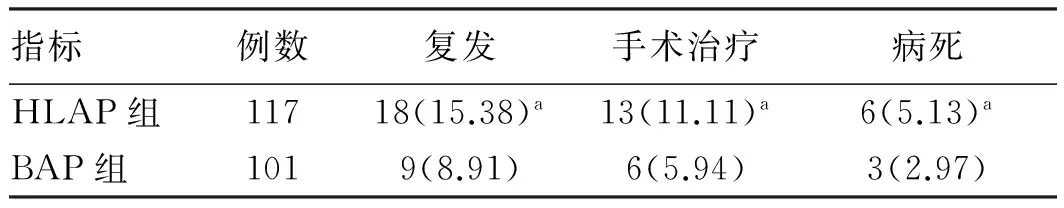
指標例數復發手術治療病死HLAP組11718(15.38)a13(11.11)a6(5.13)aBAP組1019(8.91)6(5.94)3(2.97)
注:與BAP組比較,aP<0.05。
3 討論
隨著對HLAP患者的研究,我國學者提出關于此疾病的規范治療標準,擬定提出了關于AP的治療標準,還對AP的分類進行修改,詳細概述了局部及全身性的AP并發癥,及評估疾病嚴重程度的指標,包括對治療診斷等方面的標準,第一次確定血脂對AP的影響(TG血液含量>11.3 mmol/L發生AP概率增加,降低血脂到<5.65 mmol/L可以降低風險)及逐年上升的發病趨勢[5-7]。AP患者中并發高脂血癥的占8.9%,目前認為影響的原因可以歸為3種:(1)直接產生的損傷,通常情況下存在胰腺內或四周的TG會被胰脂肪酶水解成游離的脂肪酸,這時會有白蛋白結合這些游離的脂肪酸,但是當游離脂肪酸量超過能夠結合的白蛋白量時過多的游離脂肪酸就會損傷胰腺泡細胞還有血管內皮細胞;(2)血液循環障礙,TG含量過高會抑制纖溶酶原、AMY、UAMY及Ⅶ因子活性,并且血清中血脂過高容易出現血栓堵在微血管,導致胰腺中的血液循環異常,組織得不到充足的血液供應出現壞死;(3)胰蛋白酶原被激活,當患者發生AP時,游離脂肪酸增多會刺激機體產生更多的蛋白酶原,這樣會加重對胰腺泡細胞的損傷[8-9]。對于HLAP出現的臨床特征還在進一步的研究,多數學者認為HLAP患者會出現明顯升高的TG水平,并且血液出現脂濁樣,沒有明顯升高AMY或UAMY,不斷地反復發作,并發脂肪肝、糖尿病等[10]。G??men等[11]研究認為HLAP會導致更多的并發癥及加重病情。Xu等[12]研究認為TG血癥不會直接影響AP的嚴重程度及引發并發癥。
一旦身體中有組織被損傷或炎癥反應時,單核細胞和免疫細胞會被刺激活化釋放出能夠讓肝臟上皮細胞釋放急性應激炎癥蛋白的因子,這種應急炎癥反應蛋白叫作CRP,屬于組織損傷炎癥反應的標志物[13]。很多臨床試驗證明,整個AP過程中CRP起關鍵作用,在血液中的含量直接關系到AP的病情還有發生并發癥的概率[14]。經過不斷地分析AP患者發病原因數據,現在可以將診斷AP的病情程度量化為CRP>150 mg/L這一閾值進行判斷[15-17]。內科治療HLAP當下主要為保守治療,除了常規的治療之外還考慮到血脂對病情的影響所以配合降血脂藥物進行治療[18]。Kruszyna等[19]研究認為治療過程中做到凈化血液,靜脈注射胰島素、低分子量肝素等是比較關鍵的治療措施,其中最核心的就是降低血液中TG的含量。
本研究結果顯示HLAP組的TG、TC、HDL-C、LDH-C、Apo-A和Apo-B含量水平高于BAP組,兩組之間比較,差異有統計學意義。HLAP組的AMY、UAMY和LDH含量水平低于BAP組,HLAP組的Glu、HCT和CRP含量水平高于BAP組,兩組之間比較,差異有顯著統計學意義。HLAP組的復發、手術治療和病死例數高于BAP組,兩組之間比較,差異有統計學意義。這表明HLAP患者中,血清中TG水平增加的更多,它能顯著干擾AMY活性的檢測,同時該抑制因子還可以通過腎臟進入尿液,抑制UAMY活性從而使其檢測值下降。此外,AMY和UAMY不升高,伴有糖尿病、脂肪肝等伴隨疾病,容易合并局部或全身并發癥,從而增加產生復發、手術治療和病死的概率。
綜上所述,HLAP患者的糖脂質含量水平高于BAP患者,AMY和UAMY含量水平低于BAP患者。
[1]Kusnierz K, Nowakowska-Dulawa E, Pilch-Kowalczyk J, et al. Biliary cast syndrome in a non-transplant patient with acute pancreatitis [J]. Dig Liver Dis, 2012, 44(6): 534-535.
[2]Dubravcsik Z, Hritz I, Fejes R, et al. Early ERCP and biliary sphincterotomy with or without small-caliber pancreatic stent insertion in patients with acute biliary pancreatitis: better overall outcome with adequate pancreatic drainage [J]. Scand J Gastroenterol, 2012, 47(6): 729-736.
[3]Saraswat VA, Sharma BC, Agarwal DK, et al. Biliary microlithiasis in patients with idiopathic acute pancreatitis and unexplained biliary pain: response to therapy [J]. J Gastroenterol Hepatol, 2014, 23(1): 1910-1918.
[4]Kruszyna T, Zajac A, Karcz D. Sphincter of Oddi manometry in patients with acute biliary pancreatitis: evidence for sphincter of Oddi dysfunction in acute biliary pancreatitis [J]. Scand J Gastroenterol, 2004, 39(7): 696-697.
[5]Billi P, Barakat B, D’Imperio N, et al. Relapses of biliary acute pancreatitis in patients with previous attack of biliary pancreatitis and gallbladder in situ [J]. Dig Liver Dis, 2003, 35(9): 653-655.
[6]de Madaria E. Pancreas and biliary tract. Which is the right moment for cholecystectomy in a patient with previous acute pancreatitis of biliary origin complicated by intraabdominal collections [J]. Gastroenterol Hepatol, 2008, 31(7): 464-465.
[7]張鐵英, 馬彬. 高脂血癥急性胰腺炎患者C反應蛋白水平及影響因素研究[J]. 寧夏醫學雜志, 2016, 38(5): 428-430. Zhang TY, Ma B. The study of CRP and related risk factor in acute pancreatitis patients with hyperlipidemia [J]. Ningxia Med J, 2016, 38(5): 428-430.
[8]Noel RA, Braun DK, Patterson RE, et al. Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study [J]. Diabetes Care, 2009, 32(5): 834-838.
[9]Nebiker CA, Frey DM, Hamel CT, et al. Early versus delayed cholecystectomy in patients with biliary acute pancreatitis [J]. Surgery, 2009, 145(3): 260-264.
[10]Martínez JF. Pancreas and biliary tree. In patients with acute pancreatitis, what monitoring measures and treatment are essential in the first 72 h after onset? [J]. Gastroenterol Hepatol, 2008, 31(9): 616-617.
[11]G??men E, Klc YA, YoldaO, et al. Comparison and validation of scoring systems in a cohort of patients treated for biliary acute pancreatitis [J]. Pancreas, 2007, 34(1): 66-69.
[12]Xu HM, Qiu YF, Wang WM. Diagnoses and treatment of 125 patients with biliary acute pancreatitis [J]. Zhong Xi Yi Jie He Xue Bao, 2006, 4(5): 537-538.
[13]Saraswat VA, Sharma BC, Agarwal DK, et al. Biliary microlithiasis in patients with idiopathic acute pancreatitis and unexplained biliary pain: response to therapy [J]. J Gastroenterol Hepatol, 2004, 19(10): 1206-1211.
[14]陳微微. 高脂血癥性急性胰腺炎患者的臨床特征(28例)[J]. 醫療裝備, 2016, 29(15): 13-14. Chen WW. Clinical characteristics of 28 cases with hyperlipidemic acute pancreatitis [J]. Medical Equipment, 2016, 29(15): 13-14.
[15]Dubravcsik Z, Hritz I, Fejes R, et al. Early ERCP and biliary sphincterotomy with or without small-caliber pancreatic stent insertion in patients with acute biliary pancreatitis: better overall outcome with adequate pancreatic drainage [J]. Scand J Gastroenterol, 2012, 47(6): 729-736.
[16]Pezzilli R, Billi P, Barakat B, et al. Ultrasonographic evaluation of the common bile duct in biliary acute pancreatitis patients: comparison with endoscopic retrograde cholangiopancreatography [J]. J Ultrasound Med, 1999, 18(6): 391-394.
[17]Mistiri S, Hadjsalah H, Achour H. Letter: acute pancreatitis in patients with biliary microlithiasis [J]. Nouv Presse Med, 1976, 5(14): 930.
[18]Guo L, Zheng T, Hu G, et al. Continuous renal replacement therapy in successful treatment of a patient with hyperlipidemic acute pancreatitis [J]. Ther Apher Dial, 2015, 19(5): 518-521.
[19]Kruszyna T, Zajac A, Karcz D. Sphincter of oddi manometry in patients with acute biliary pancreatitis: evidence for sphincter of oddi dysfunction in acute biliary pancreatitis [J]. Scand J Gastroenterol, 2004, 39(7): 696-697.
(責任編輯:馬 軍)
Comparison of glycolipid, amylase and urine amylase levels in patients with hyperlipidemia and biliary acute pancreatitis
DONG Yongchun
Department of Gastroenterology, the Institution Hospital of Chengdu Military Command, Chengdu 610011, China
Objective To compare the levels of glycolipid, amylase (AMY) and urine amylase (UAMY) in hyperlipidemic acute pancreatitis (HLAP) and biliary acute pancreatitis (BAP) patients. Methods Two hundred and eighteen cases of acute pancreatitis (AP) patients were selected in the Institution Hospital of Chengdu Military Command from Aug. 2014 to Aug. 2016, and divided into HLAP group (n=117) and BAP group (n=101). The blood lipid, serum amylase (AMY), urine amylase (UAMY), blood glucose (Glu), lactate dehydrogenase (LDH), blood hematocrit (HCT), C reactive protein (CRP) of patients with treatment and prognosis between two groups were analyzed. Results
The levels of TG, TC, HDL-C, LDH-C, Apo-A and Apo-B in the HLAP group were higher than those in BAP group, and there was statistical difference between two groups (P<0.05). The levels of AMY, UAMY and LDH in the HLAP group were lower than those in BAP group, the levels of Glu, HCT and CRP in the HLAP group were higher than those in BAP group, and there was significant difference between two groups (P<0.01). Recurrence, surgical treatment and death cases of HLAP group were higher than those in BAP group, there was statistical difference between two groups (P<0.05). Conclusion The level of serum lipid in HLAP patients is higher than the patients with BAP, the levels of AMY and UAMY in HLAP patients are lower than the patients with BAP.
Hyperlipidemic acute pancreatitis; Biliary acute pancreatitis; Serum amylase; Urine amylase
10.3969/j.issn.1006-5709.2017.07.012
R576
A
1006-5709(2017)07-0761-04
2017-06-05