椎板成形在內鏡下椎板間入路治療椎間盤突出中的應用
黃燦陽 王振強 黃杰聰 曾志遠
[摘要] 目的 研究椎板成形在局部麻醉下脊柱內鏡椎板間入路治療腰椎間盤突出中的應用。 方法 收集我院2016年1月~2018年12月行椎板間入路治療腰椎間盤突出癥患者63例,研究椎板間入路時椎板成形的應用,根據術中是否行椎板成形分為成形組和非成形組,對比了解兩組椎板成形與突出節段、突出位置、突出游離情況及原始椎板間隙大小等的關系。 結果 全部病例均成功在局部浸潤復合右美托咪定基礎麻醉下完成椎間盤突出髓核摘除手術。術后患者的VAS評分及術后ODI評分均較手術前明顯好轉,差異有統計學意義(P<0.01)。成形組術前椎板間隙高度平均(7.93±1.64)mm小于非成形組的(10.91±1.72)mm,差異有統計學意義(P<0.01);成形組突出位置肩上18例(81.82%)、腋下4例(18.18%),非成形組肩上11例(26.83%)、腋下30例(73.17%),成形組肩上型比例高于非成形組,差異有統計學意義(P<0.01);成形組突出節段L4~5 10例(45.45%)、L5~S1 12例(54.55%),非成形組L4~5 2例(4.88%)、L5~S1 39例(95.12%),成形組L4~5節段比率明顯高于非成形組,差異有統計學意義(P<0.01)。但是成形組手術時間平均(108.07±5.61) min明顯長于非成形組[(62.12±3.74) min],差異有統計學意義(P<0.01)。 結論 椎板成形在局麻內鏡椎板間入路治療腰椎間盤突出中有時候必不可少,尤其L4~5節段、術前椎板間隙較小及肩上型突出時,能有效擴大內鏡通道、減少鞘管對神經根牽拉等,鏡下的椎板成形在將來脊柱內鏡手術中將大有作為。
[關鍵詞] 腰椎間盤突出;內鏡;椎板間入路;椎板成形
[中圖分類號] R687.3 ? ? ? ? ?[文獻標識碼] B ? ? ? ? ?[文章編號] 1673-9701(2019)32-0059-04
Application of laminoplasty by endoscopic interlaminar approach for the treatment of intervertebral disc herniation
HUANG Canyang WANG Zhenqiang HUANG Jiecong ZENG Zhiyuan
Department of Orthopaedics, Quanzhou First Hospital Affiliated to Fujian Medical University, Quanzhou ? 362000,China
[Abstract] Objective To study the application of laminoplasty by endoscopic interlaminar approach for the treatment of intervertebral disc herniation. Methods 63 cases of lumbar disc herniation treated by interlaminar approach from January 2016 to December 2018 in our hospital were collected. The application of laminoplasty by endoscopic interlaminar approach was studied. According to whether or not laminoplasty was performed during operation, they were divided into laminoplasty group and non-laminoplasty group. The relationship between the laminoplasty and protruding segment, the protruding position, the protruding free condition, and the size of the original lamina gap were compared. Results All cases successfully completed the removal of herniated nucleus pulposus of lumbar disc herniation under anesthesia with local infiltration combined with dexmedetomidine. The VAS score and postoperative ODI score of the patients after operation were significantly better than those before surgery, and the difference was statistically significant(P<0.01). The average height of the lamina before operation was(7.93±1.64) mm in the laminoplasty group, less than(10.91±1.72)mm in the non-laminoplasty group, and the difference was statistically significant(P<0.01). There were 18 cases(81.82%) of protruding position above the shoulder and 4 cases(4.18%) of protruding position below the shoulder in the laminoplasty group. There were 11 cases(26.83%) of protruding position above the shoulder and 30 cases (73.17%) of protruding position below the shoulder in the laminoplasty group. The proportion of above-shoulder herniation in the laminoplasty group was higher than that in the non-laminoplasty group, and the difference was statistically significant(P<0.01). There were 10 cases(45.45%) of L4-5 protruding and 12 cases(54.55%) of L5-S1 protruding in the laminoplasty group. There were 2 cases(4.88%) of L4-5 protruding and 39 cases(95.12%) of L5-S1 protruding in the non-laminoplasty group. The ratio of L4-5 protruding in the laminoplasty group was higher than that in the non-laminoplasty group, and the difference was statistically significant(P<0.01). However, the average operation time of the laminoplasty group was(108.07±5.61)min, and that of the non-forming group was(62.12±3.74)min. The difference was statistically significant(P<0.01). Conclusion Laminoplasty is sometimes necessary in the treatment of lumbar disc herniation with local anesthesia and interlaminar approach, especially in the L4-5 segment and when the preoperative lamina is small and protruding position is above the shoulder. It can effectively enlarge the endoscopic channel and reduce the pulling of sheath to the nerve root. Laminoplasty under the microscope will be useful in future endoscopic surgery.
[Key words] Lumbar disc herniation; Endoscopy; interlaminar approach; Laminoplasty
腰椎間盤突出癥是脊柱骨科最為常見的疾病。除了保守治療,內鏡治療逐漸成為手術治療的熱門選擇,因為其微創、高效、恢復快,受到脊柱外科醫生及患者青睞。內鏡治療中入路選擇很多但總體上可分為經椎間孔入路及椎板間入路兩種方式[1-3]。在這兩種方式中均可能需要對椎間孔及椎板間隙進行骨性成形以擴大入路通道。對于椎間孔通道的骨性成形有較多報道,但對于椎板成形在椎板間入路中的報道則較少[4]。本文旨在收集2016年1月~2018年12月我院行局部麻醉下椎板間入路治療腰椎間盤突出癥患者63例,研究椎板間入路時椎板成形的應用,了解椎板成形與突出節段、突出位置、突出游離情況及原始椎板間隙大小等關系。現報道如下。
1 資料與方法
1.1 一般資料
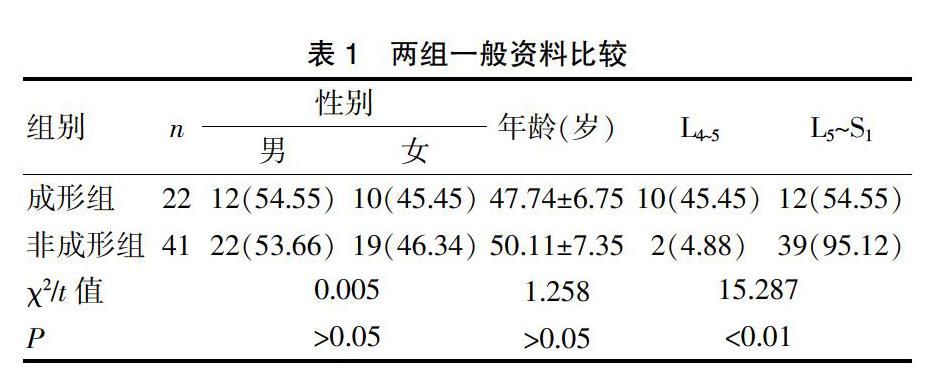
選取2016年1月~2018年12月在我院行局麻下椎板間入路脊柱內鏡治療的腰椎間盤突出癥患者63例,根據術中是否行椎板成形分為成形組(22例)和非成形組(41例)。成形組:男12例,女10例;年齡23~70歲,平均(47.73±6.75)歲;病變位置L4~5 10例,L5~S1 12例。非成形組:男22例,女19例;年齡28~76歲,平均(50.11±7.35)歲;病變位置L4~5 2例,L5~S1 39例。患者臨床癥狀、體征及影像資料診斷為腰椎間盤突出,經保守治療6周無緩解。兩組患者一般資料比較,差異無統計學意義(P>0.05),具有可比性。見表1。
表1 ? 兩組一般資料比較
1.2 方法
1.2.1 手術方法 ?所有患者俯臥于專用腰椎后弓墊上,減少腰椎前凸,增加腰椎板間隙面積;腹部懸空減少腹壓所致術中出血。手術器械采用德國SPINENDOS脊柱內窺鏡手術系統(外鞘套管直徑8 mm),該系統包括內窺鏡監視系統和髓核摘除的手術器械。術前C臂定位責任節段手術側椎板間隙。常規用3%碘酒及75%酒精消毒、鋪巾。旁開后正中線約在小關節突處插入定位針,深達骨表面。局部5%利多卡因10 mL稀釋1倍局部浸潤麻醉,尤其注意椎板間隙外側緣關節突關節內側與黃韌帶交界處的浸潤麻醉,復合靜脈右美托咪定麻醉下手術。在距棘突旁0.5 cm處做一約0.8 cm的縱行切口,依次切開皮膚、皮下、深筋膜。采用鉛筆頭狀擴張管鈍性擴張,深至黃韌帶外側近關節突關節內側緣表面,逐層擴張并置入外工作通道,再次透視確定手術椎間隙。取出擴張管,置入短內窺鏡(外鞘直徑8 mm),清理黃韌帶及小關節突內側緣骨表面的脂肪肌肉等軟組織,顯露小關節內側緣交界處黃韌帶(封三圖1A)。等離子燒灼、藍鉗咬開逐層破開關節突內側緣黃韌帶,可見硬膜外脂肪。術中根據椎板間隙大小、突出位置及工作套管牽開神經根時患者的耐受程度選擇是否行椎板成形及成形大小,術中通過磨鉆及椎板咬骨鉗行椎板成形,有時候需成形椎板下緣甚至下位椎體上關節突內側部(封三圖1B),松解神經根。神經剝離子探查突出髓核組織,剝離子牽開保護神經根并旋轉放入外工作套,摘除游離及松動的間盤髓核組織,直至硬膜囊及神經根充分減壓,雙極射頻電極消融絮狀髓核并行纖維環成形。
1.2.2 影像采集方法 ?CT三維重建:取患者平臥位,雙手自然放置軀干兩邊,采用GE64排lightVCT,電壓120 kV、電流300 mA,層厚5 mm,拆薄0.625,GE adw4.6工作站,采用VR、MPR重建系列,掃描椎板減壓及上下共3個椎體。MRI檢查:取患者平臥位,雙手自然放置軀干兩邊,采用GE3.0T,矢狀位T2、T1、T2壓脂序列,橫斷位T2序列。矢狀位掃描方位平行于脊柱,范圍包含雙側椎弓根,橫斷位T2掃描平行于椎間盤走形。T2參數:TR3000 ms,TE80 ms,激勵次數為2;T1參數:TR800 ms,TE20 ms,激勵次數為2。矢狀位層厚4 mm,層間隔1 mm,fov240×240 mm,相位編碼方向A/P;橫斷位層厚4 mm,層間隔0.5 mm,fov180×180 mm,相位編碼方向A/P。掃描包括手術椎間盤間隙的整個腰椎。
1.3 觀察指標
術前椎板間隙高度:術前通過CT三維測量椎板間隙高度,以矢狀位下板間距離最大值為術前椎板間隙高度值(封三圖2);突出位置:術前通過MRI(封三圖3)及CT三維影像判斷行走神經根與突出物之間的關系將突出位置分為肩上、腋下兩型,主要通過磁共振水平位影像判斷突出髓核與神經根關系;術前腰腿痛視覺模擬評分VAS評分;術前Oswestry功能障礙指數ODI評分。
術后復查三維CT測量椎板成形情況(封三圖2);復查MRI(封三圖4)察看椎間盤殘留情況;術后3個月VAS評分;術后3個月ODI評分。
1.4 統計學方法
采用SPSS25.0統計學軟件處理數據,計量資料以均數±標準差(x±s)表示,兩組間比較采用成組t檢驗或多變量方差分析;計數資料采用χ2檢驗,P<0.05為差異有統計學意義。
2 結果
所有患者皆順利完成手術,未見神經根損傷、硬脊膜撕裂、椎管內血腫等并發癥,復查MRI皆未見明顯突出髓核殘留。
2.1 兩組手術前后VAS評分、ODI評分、手術時間比較
兩組手術前后VAS評分比較,差異無統計學意義(P>0.05);兩組手術后均較手術前明顯好轉(P<0.01)。兩組手術前后ODI評分比較,差異無統計學意義(P>0.05);兩組手術后均較手術前明顯好轉(P<0.01)。成形組手術時間(108.07±5.61)min,明顯大于非成形組(62.12±3.74)min,(P<0.01)。見表2。
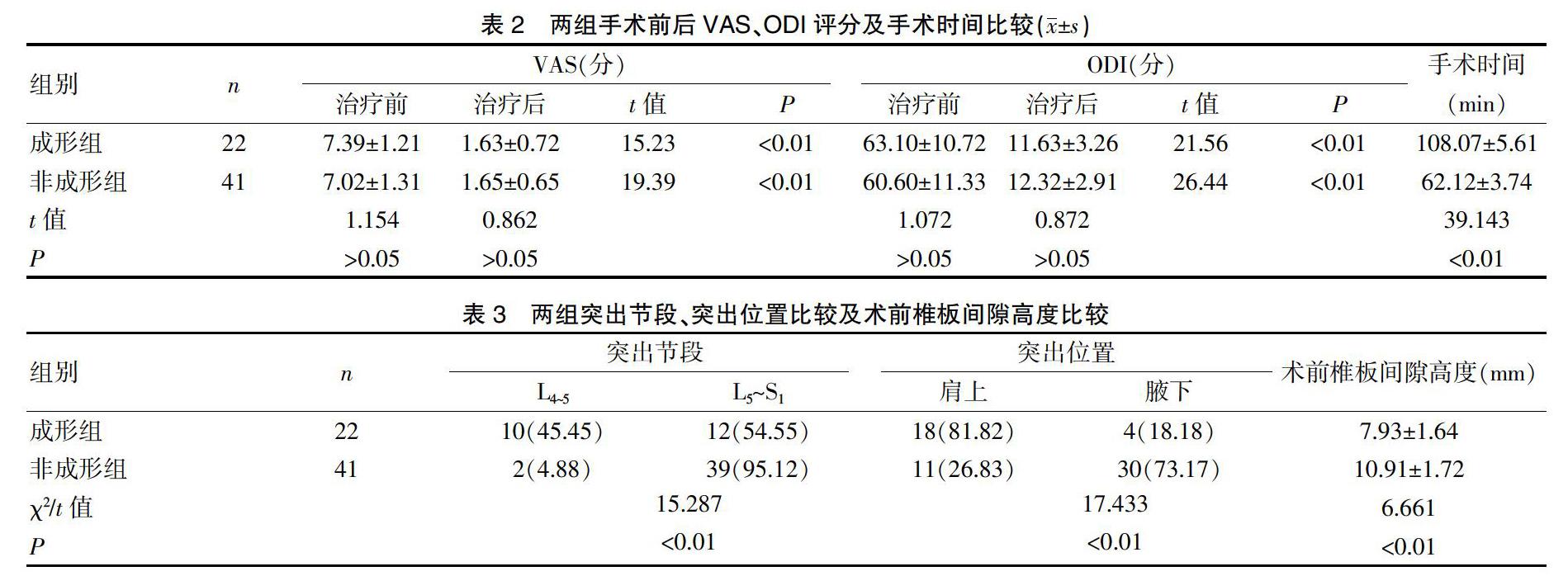
2.2 兩組突出節段、突出位置、術前椎板間隙高度比較
從突出節段上看L4~5節段間隙成形機會較大(P<0.01);從突出位置上看肩上型突出椎板成形機會較大(P<0.01)。術前椎板間隙高度比較,成形組(7.93±1.64)mm、非成形組(10.91±1.72)mm。成形組術前椎板間隙高度明顯小于非成形組,差異有統計學意義(P<0.01)。見表3。
3 討論
椎間盤突出的脊柱內鏡治療主要分為椎間孔入路和椎板間入路兩種[5]。椎間孔入路具有對神經牽拉較少、良好的局麻耐受性等優點,是腰椎間盤突出內鏡治療的理想通道。由于下腰段的解剖特點如高髂脊、橫突粗大、椎間孔變小等,經椎間孔入路內鏡并不容易到達突出椎間盤。相反下腰段的椎板間隙越往下越大,有利脊柱內鏡的操作[6],這時椎板間入路更具優勢。但椎板間入路術中需通過鞘管牽拉神經根增加了神經損傷可能,特別是全身麻醉情況下。
局麻下的脊柱內鏡手術可以更好保證手術安全性。脊柱內鏡手術中麻醉的選擇主要是考慮手術安全性與手術舒適性的平衡[7-8]。全麻手術患者具有最好的舒適性,但在沒有神經監護下術中神經損傷機會亦增加,帶來更多安全性擔憂。目前為了手術安全性經椎間孔入路皆采用局部麻醉下手術。而經椎板間入路因為和傳統開放手術類似采用全麻下手術。全麻下椎板間入路內鏡手術雖然帶來最好的手術舒適性及耐受性,但亦有馬尾損傷等安全問題報告[9]。所以為了安全性本研究嘗試在局麻下行椎板間入路內鏡手術。我們可能需要椎板成形來保證手術的耐受性。
椎板的擴大成形是局部麻醉椎板間入路腰椎髓核摘除手術成功實施的有力保證。正如在椎間孔入路手術中椎間孔擴大成形是成功的重要環節。椎板成形在開放椎間盤突出手術中已經應用廣泛,也是手術中主要的操作步驟[10]。同樣在椎板間入路內鏡手術時我們也可以行椎板成形。
而在局部麻醉下內鏡手術中椎板成形有著特殊幾個目的:①擴大操作通道有利內鏡的進入,一般來說椎板間隙高度小于8 mm時無法滿足后路內鏡鞘管置入的基本要求,因此必須成形椎板擴大椎板間隙;②減少神經牽拉,后路椎板間隙入路局麻手術中如果神經牽拉厲害往往患者無法耐受并且術后神經損傷亦增加。在肩上型突出尤其是小關節突內聚的患者為了減少鞘管轉動牽拉對神經根干擾,在椎板間入路手術時需要行椎板成形將外側椎板甚至下位椎體的上關節突內側緣成形,有利手術操作無需牽拉神經根而直面突出的髓核[11-12];③擴大骨性側隱窩間隙,椎板成形擴大后側隱窩骨性間隙能有效的減少癥狀性椎間盤突出復發[13];④高游離靶點通道的需要,對于高度游離的椎間盤突出椎板間隙后入路是一種相對無盲區的選擇,除了極外側突出[14-16]。但是這時需要對內鏡套管進行大成角放置,甚至需要在椎板上特殊制道,需要對椎板進行成形來滿足手術要求。
然而局麻下椎板間入路的椎間盤髓核摘除手術何時需要行椎板成形?通過本研究發現是否需要行椎板成形與患者術前椎板間隙高度、手術椎間盤的節段及突出位置密切相關。需要成形的手術組術前椎板間隙高度較低,為了容納操作器械及操作空間需要一定的椎板間隙。L4~5節段更需要行椎板成形,因為L4~5本來椎板間隙高度就小,所以更有機會需要成形椎板擴大空間。肩上型突出更需要成形,應該是肩上型突出的椎間盤更多的覆蓋在椎板下,而腋下型突出更多覆蓋于黃韌帶下的緣故。
椎板成形契合了目前脊柱內鏡高速發展、內鏡的手術適應證擴大的需要。越來越多的開放手術都是內鏡手術指征,如鏡下椎管狹窄椎管擴大減壓、鏡下融合技術等。適應證的擴大均是建立在鏡下椎板擴大成形,甚至擴大到小關節突關節成形的基礎上,所以椎板成形在后路椎板間隙入路的脊柱內鏡手術中大有可為。
[參考文獻]
[1] Wang B.,Guo HL,Liu W,et al. Full-endoscopic interlaminar approach for the surgical treatment of lumbar disc herniation:The causes and prophylaxis of conversion to open[J]. Arch Orthop Trauma Surg,2012,132(11):1531-1538.
[2] Hoogland T,Schubert M,Miklitz B,et al. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain:A prospective randomized study in 280 consecutive cases[J]. Spine,2006, 31(24):890-897.
[3] Ruetten S,Komp M,Merk H,et al. Use of newly developed instruments and endoscopes:Full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach[J]. Journal of Neurosurgery Spine,2007,6(6):521-530.
[4] Xinyu L,Yanping Z,Jianmin L,et al. Hemilaminoplasty for the treatment of lumbar disc herniation[J]. International Orthopaedics,2009,33(5):1323-1327.
[5] Jha RT,Syed HR,Catalino M,et al. Contralateral approach for minimally invasive treatment of upper lumbar intervertebral disc herniation:Technical note and case series[J]. World Neurosurg,2017,100:583-589.
[6] Tonosu J,Oshima Y,Shiboi R,et al. Consideration of proper operative route for interlaminar approach for percutaneous endoscopic lumbar discectomy[J]. Journal of Spine Surgery,2016,2(4):281-288.
[7] Yeung AT,Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation[J]. Spine,2002,27(7):722-731.
[8] 王冰,呂國華,劉偉東. 完全內窺鏡下經椎板間入路手術治療腰椎間盤突出癥術中轉為開放手術的原因分析[J]. 中國脊柱脊髓雜志,2011,21(3):185-188.
[9] Wang, H.,Zhou Y,Li C,et al. Risk factors for failure of single-level percutaneous endoscopic lumbar discectomy[J].J Neurosurg Spine,2015,23(3):320-325.
[10] 李亢. 小切口椎板開窗術與顯微內鏡下髓核摘除術治療腰椎間盤突出癥的療效比較[J]. 醫學綜述,2013,19(12):2290-2292.
[11] 劉元彬,張智,鄭佳狀,等. 經椎板間入路椎間孔鏡治療巨大游離型腰椎間盤突出癥[J]. 中國微創外科雜志,2018,18(7):616-618.
[12] 孔翔飛,吳小濤,齊新生,等. 經椎板間隙入路椎間盤鏡手術治療合并小關節內聚的腰椎間盤突出癥[J]. 中國微創外科雜志,2001,1(6):352-353.
[13] Li Z,Yang H,Liu M,et al. Clinical characteristics and risk factors of recurrent lumbar disk herniation:A retrospective analysis of three hundred twenty-one cases[J]. Spine,2018,43(21):1463-1469.
[14] Choi G,Lee SH,Raiturker PP,et al. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope[J]. Neurosurgery,2006,58(1 Suppl):59-68.
[15] Hirano Y,Mizuno J,Takeda M,et al. Percutaneous endoscopic lumbar discectomy-early clinical experience[J]. Neurologia Medico-Chirurgica,2012,52(9):625-630.
[16] Yasushi I,Yasushi O,Hirokazu I,et al. Percutaneous endoscopic lumbar discectomy via adjacent interlaminar space for highly down-migrated lumbar disc herniation:A technical report[J]. J Spine Surg,2018,4(2):483-489.
(收稿日期:2019-06-03)