健骨方預防椎體成形術后再發骨折的療效觀察
張偉 李偉 田峰 張志強 朱先龍


【摘要】 目的:觀察北京市懷柔區中醫醫院院內制劑健骨方對骨質疏松性椎體壓縮骨折椎體成形術后再發骨折的預防效果。方法:選取2015年1月-2016年1月本院收治的單一椎體壓縮骨折患者116例,隨機將患者分為觀察組和對照組,每組58例。對照組予經皮椎體后凸成形術治療,觀察組予經皮椎體后凸成形術治療后結合健骨方加減治療。對兩組患者進行為期2年的隨訪,分別于術后1周、1年、2年對患者進行骨密度(BMD)檢測,通過Oswestry功能障礙指數問卷表(ODI)評估功能障礙,WHO疼痛緩解程度標準評估治療效果,對疼痛復發加重的患者,應用MRI檢查確診是否再發骨折。結果:最終納入統計的患者111例,其中觀察組56例、對照組55例。觀察組患者術后1周、1年、2年的治療總有效率雖均高于對照組,但差異均無統計學意義(P>0.05)。術后1、2年,對照組腰椎、髖部骨密度值均低于觀察組,差異均有統計學意義(P<0.05)。術后2年,觀察組再發骨折例數少于對照組,差異有統計學意義(P<0.05)。術后1年,觀察組的日常生活自理能力、提物、疼痛評分均優于對照組,差異均有統計學意義(P<0.05);術后2年,觀察組的日常生活自理能力、提物、睡眠、社會活動、旅行、疼痛評分均優于對照組,差異均有統計學意義(P<0.05)。結論:骨質疏松性椎體壓縮骨折椎體成形術手術效果肯定,北京市懷柔區中醫醫院骨科院內制劑健骨方具有改善骨質疏松,降低椎體再發骨折的作用,可明顯改善患者術后的遠期功能。
【關鍵詞】 椎體壓縮骨折 椎體成形術 健骨方
The Effect of Jiangu Formula on Prevention of Recurrent Fracture after Vertebroplasty/ZHANG Wei, LI Wei, TIAN Feng, ZHANG Zhiqiang, ZHU Xianlong. //Medical Innovation of China, 2020, 17(02): 005-009
[Abstract] Objective: To observe the preventive effect of Jiangu Formula in the Huairou District Hospital of Traditional Chinese Medicine on the recurrent fracture after vertebroplasty for osteoporotic vertebral compression fracture. Method: From January 2015 to January 2016, 116 patients with a single vertebal compression fracture were selected, they were randomly divided into observation group and control group, 58 cases in each group. The control group was treated with percutaneous kyphoplasty, and the observation group was treated with percutaneous kyphoplasty combined with Jiangu Formula. The patients in the two groups were followed up for 2 years. The BMD of the patients were measured at 1 week, 1 year and 2 years after the operation. The dysfunction was assessed by the Oswestry Disability Index questionnaire (ODI), and the treatment effect was assessed by the WHO pain relief standard. For the patients with pain recurrence and aggravation, MRI was used to check whether there was recurrent fracture. Result: 111 patients were included in the final statistics, include 56 patients in the observation group and 55 patients in the control group. Although the total effective rate of the observation group at 1 week, 1 year and 2 years after surgery were higher than those of the control group, but the differences were not statistically significant (P>0.05). 1 year and 2 years after operation, the BMD of lumbar vertebrae and hip in the control group were lower than those in the observation group, the differences were statistically significant (P<0.05). 1 year after the operation, the daily self-care ability, extract and pain of the observation group were all better than those of the control group, with statistically significant differences (P<0.05); 2 years after the operation, daily life self-care ability, extract, sleep, social activities, travel and pain in the observation group were better than those of the control group, with statistically significant differences (P<0.05). Conclusion: The effect of vertebroplasty for osteoporotic vertebral compression fracture is positive, the preparation of Jiangu Formula in the orthopedic department of Huairou District Hospital of Traditional Chinese Medicine in Beijing has the effect of improving osteoporosis and reducing the recurrence fracture of vertebral body, which can significantly improve the long-term function of patients after operation.
[Key words] Vertebral compression fracture Vertebroplasty Jiangu Formula
First-authors address: Hospital of Traditional Chinese Medicine, Huairou District, Beijing 101400, China
doi:10.3969/j.issn.1674-4985.2020.02.002
隨著我國平均壽命增加,目前老年人普遍存在骨質疏松的情況,骨質疏松使椎體脆性增加,胸腰段椎體是力的主要承受部位,故易發生椎體壓縮性骨折[1-3]。其臨床主要癥狀為腰背部疼痛,嚴重影響中老年人的日常生活質量。目前經皮球囊擴張后凸成形術(percutaneous kyphoplasty,PKP)和經皮椎體成形術(percutaneous vertebroplasty,PVP)是治療骨質疏松性椎體壓縮骨折的主要方式,創傷小、可迅速止痛,改善功能障礙,有效提高老年患者生活質量[4-7]。再發骨折是術后常見并發癥,中醫藥制劑對再發骨折的預防成為中醫系統研究熱點,本院骨科對2015年1月-2016年1月收治的116例椎體成形術后患者進行中藥干預并隨訪研究,以期觀察健骨方對單純骨質疏松性椎體壓縮骨折成形術后再發骨折的預防療效,現將研究結果報道如下。
1 資料與方法
1.1 一般資料 抽選2015年1月-2016年1月本院收治的單一椎體壓縮骨折患者116例,納入標準:符合原發性骨質疏松癥診斷標準;明確診斷單一椎體壓縮性骨折(MRI提示新鮮壓縮骨折);無明顯手術禁忌證。排除標準:有明確外傷病史;伴有較嚴重基礎疾病者。其中男10例,女106例,年齡55~89歲,平均(69.4±7.3)歲,病程3~16 d,平均(6.6±2.2)d。隨機將患者分為觀察組和對照組,各58例。觀察組:2例患者無法完成長期服用湯藥,56例入組;對照組:2例患者失訪,1例患者死亡,55例入組;最終納入統計111例。此次研究已得到本院倫理委員會批準,患者均簽署治療及隨訪知情同意書。
1.2 方法 (1)對照組予經皮椎體后凸成形術治療。患者取俯臥位,C型臂定位患椎,局部麻醉后經椎弓根穿刺,導管針至椎體中前1/3處,調和骨水泥后在C型臂透視下緩慢注入椎體。術畢觀察雙下肢感覺活動,術后24 h腰圍保護下地活動。(2)觀察組予經皮椎體后凸成形術治療后結合健骨方加減治療。兩組患者術后均予健康宣教、協助指導鍛煉腰背肌肉,術后第2天下地行走復查X線片,術后第3天出院;出院后均于門診予骨化三醇、碳酸鈣等鈣劑藥物服用,觀察組患者額外服用健骨方,該方由北京市懷柔區中醫醫院骨科院內制劑,主要組成如下:補骨脂12 g、骨碎補12 g、淫羊藿9 g、懷牛膝15 g、蛇床子6 g、桑葚15 g、黃芪30 g、杜仲15 g等。辨證加減,陰虛者加用烏梅、酒黃精、地骨皮等;血瘀者加用桃仁、紅花等。隔天服1劑,早晚分服,間隔3個月復查肝腎功,半年后停服。兩組患者均隨訪24個月。
1.3 觀察指標與評價標準 (1)比較兩組治療效果,以WHO疼痛緩解程度為評價標準。完全緩解(CR):治療后完全無痛;部分緩解(PR):疼痛較治療前明顯減輕,基本不影響睡眠,能正常生活;輕度緩解(MR):疼痛較治療前有所減輕,但仍明顯,睡眠受影響;無效(NR):治療前后疼痛程度無變化。總有效率=(CR例數+PR例數)/總例數×100%。(2)通過雙能X線骨密度儀檢測,比較兩組術后1周、1年、2年的腰部、雙髖部骨密度數值(BMD)。(3)比較兩組Oswestry功能障礙指數評分。Oswestry功能障礙指數量表評價內容包括日常生活自理能力、提物、行走、坐、站立、睡眠、社會活動、旅行、疼痛程度等情況,每項內容評分為0~5分,分數越高功能越差。(4)對疼痛復發加重的患者,應用MRI檢查確診是否再發骨折。
1.4 統計學處理 采用SPSS 15.0軟件對所得數據進行統計分析,計量資料用(x±s)表示,比較采用t檢驗;計數資料以率(%)表示,比較采用字2檢驗。P<0.05為差異有統計學意義。
2 結果
2.1 兩組一般資料比較 兩組患者的一般資料比較,差異均無統計學意義(P>0.05),具有可比性,見表1。
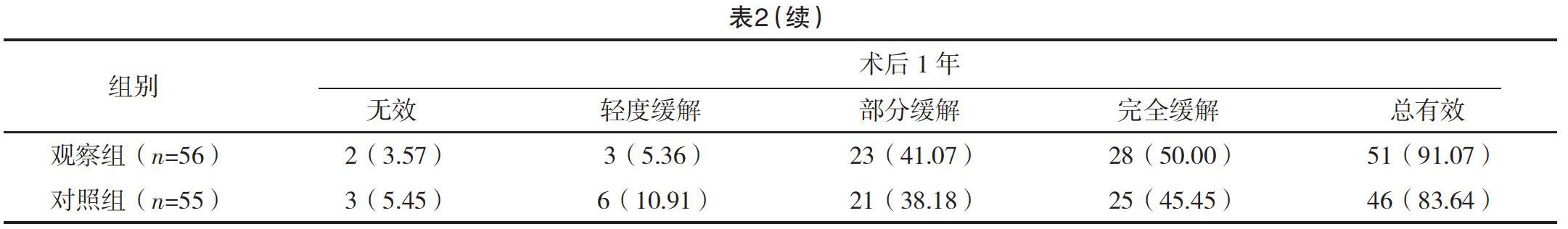
2.2 兩組術后疼痛緩解效果比較 觀察組患者術后
1周、1年、2年的治療總有效率雖均高于對照組,但差異均無統計學意義(字2=0.000、1.392、1.582,P=0.985、0.238、0.209),見表2。
2.3 兩組術后腰椎、髖部骨密度比較 兩組術后1周腰椎、髖部骨密度值比較,差異均無統計學意義(P>0.05);術后1、2年,對照組腰椎、髖部骨密度值均低于觀察組,差異均有統計學意義(P<0.05)。見表3。
2.4 兩組術后再發骨折情況比較 術后1年,兩組再發骨折情況比較,差異無統計學意義(P>0.05);術后2年,觀察組再發骨折例數少于對照組,差異有統計學意義(P<0.05)。見表4。
2.5 兩組術后Oswestry功能障礙指數評分比較 術后1周,兩組患者在Oswestry功能障礙指數中9個方面比較,差異均無統計學意義(P>0.05);術后1年,觀察組的日常生活自理能力、提物、疼痛評分均優于對照組,差異均有統計學意義(P<0.05);術后2年,觀察組的日常生活自理能力、提物、睡眠、社會活動、旅行、疼痛評分均優于對照組,差異均有統計學意義(P<0.05)。見表5。
3 討論
PKP和PVP是治療骨質疏松性胸腰椎體壓縮性骨折的主要方式之一,療效已經得到文獻[8-11]研究證實,但隨著患者年齡增加,骨質疏松加重,使患者再次出現腰背部疼痛甚至骨折,進而影響術后患者的遠期效果,所以系統全程的抗骨質疏松治療才是治療疾病的根本,符合中醫理論“標本兼治”。
經脈受損、氣機失調、血不循經溢于脈外、離經之血瘀滯于肌膚腠理為產生疼痛的主要原因[12]。經過椎體成形術后,主要病機由血瘀氣滯轉變為腎虛、脾虛有關;中醫學認為“腎為先天之本,主生長發育”“腎藏精,主骨生髓”,如腎精虧損則不能滋養全身之骨,則骨枯髓減,導致骨痿。結合中醫基礎理論及現代藥理研究,筆者提出了治療椎體壓縮骨折術后骨質疏松癥的主要原則為補腎壯骨、健脾益氣、活血通絡,據此原則組方,研制出防治骨質疏松癥的健骨方。該方以補骨脂補腎助陽壯骨為君藥;輔之骨碎補、淫羊藿加強其補腎壯陽之功為臣藥;同時配以黃芪補中益氣;杜仲、桑葚補益肝腎,此乃“善補陽者,必于陰中求陽”和“壯水之主,以制陽光”之意。現代藥物實驗研究表明,較高濃度補骨脂對分離破骨細胞性骨吸收有抑制作用,它抑制了骨吸收陷窩的增加和擴大[13]。補骨脂中的有效成分異補骨脂素能顯著促進骨髓間充質干細胞的成骨性分化,從而起到抗骨質疏松的作用[14]。淫羊藿可通過保護性腺、抑制骨吸收和促進骨形成等途徑,使機體骨代謝處于骨形成大于骨吸收的正平衡狀態,抑制骨量丟失,防止骨質疏松的發生[15]。
本研究結果顯示,術后1、2年,對照組腰椎、髖部骨密度值均低于觀察組,差異均有統計學意義(P<0.05);且術后2年,對照組發生再骨折的例數明顯多于觀察組(P<0.05),這說明健骨方在治療過程中可以維持平穩骨密度,從而降低椎體再骨折的風險。兩組患者在癥狀改善及治療總有效率方面,差異均無統計學意義(P>0.05),充分肯定了PKP和PVP的手術效果。術后1年,觀察組的日常生活自理能力、提物、疼痛評分均優于對照組,差異均有統計學意義(P<0.05);術后2年,觀察組的日常生活自理能力、提物、睡眠、社會活動、旅行、疼痛評分均優于對照組,差異均有統計學意義(P<0.05);充分說明了中藥補腎健骨治療對骨質疏松性胸腰椎體壓縮性骨折的具有較好的遠期療效。
綜上所述,椎體成形術是目前臨床治療骨質疏松性椎體壓縮骨折的主要方法,健骨方能提高骨密度,降低椎體再骨折的風險,明顯改善患者術后的功能和癥狀。
參考文獻
[1] Bae J S,Park J H,Kim K J,et al.In Reply to the letter to the editor regarding “analysis of risk factors for secondary new vertebral compression fracture following percutaneous vertebroplasty in patients with osteoporosis”[J].World Neurosurg,2017,99:387-394.
[2] Wang Y,Zhong H,Zhou Z,et al.Letter to the editor regarding “analysis of risk factors for secondary new vertebral compression fracture following percutaneous vertebroplasty in patients with osteoporosis”[J].World Neurosurg,2017,103:924-925.
[3] Lee D G,Park C K,Park C J,et al.Analysis of Risk Factors Causing New Symptomatic Vertebral Compression Fractures After Percutaneous Vertebroplasty for Painful Osteoporotic Vertebral Compression Fractures[J].Journal of Spinal Disorders & Techniques,2015,28(10):E578.
[4] Yan L,He B,Guo H,et al.The prospective self-controlled study of unilateral transverse process-pedicle and bilateral puncture techniques in percutaneous kyphoplasty[J].Osteoporos Int,2016,27(5):1849-1855.
[5] Gu Y T,Zhu D H,Liu H F,et al.Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty for preventing secondary fracture after vertebroplasty[J].J Orthop Surg Res,2015,10:31.
[6] Firanescu C E,De Vries J,Lodder P,et al.Percutaneous Vertebroplasty is no Risk Factor for New Vertebral Fractures and Protects Against Further Height Loss (VERTOS IV)[J].CardioVascular and Interventional Radiology,2019,42(7):991-1000.
[7] Xie L L,Chen X D,Yang C Y,et al.Efficacy and complications of 125I seeds combined with percutaneous vertebroplasty for metastatic spinal tumors: a literature review[J].Asian Journal of Surgery,2019,36(8):1020-1024.
[8] Yan L,He B,Guo H,et al.The prospective self-controlled study of unilateral transverse process-pedicle and bilateral puncture techniques in percutaneous kyphoplasty[J].Osteoporos Int,2016,27(5):1849-1855.
[9] Gu Y T,Zhu D H,Liu H F,et al.Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty for preventing secondary fracture after vertebroplasty[J].J Orthop Surg Res,2015,10:31.
[10] Shiva S J J,Roah M,Stefanos F,et al.Imaging Improves Efficacy of Vertebroplasty-A Systematic Review and Meta-Analysis[J].The Canadian Journal of Neurological Sciences.Le Journal Canadien Des Sciences Neurologiques,2019,46(5):1-33.
[11] Ge Z,Ma R,Chen Z,et al.Uniextrapedicular kyphoplasty for the treatment of thoracic osteoporotic vertebral fractures[J].Orthopedics,2015,36(8):e1020-1024.
[12]孫月釗,郭寧國,強曉軍,等.骨質疏松性骨折術后再發骨折的危險因素分析[J].深圳中西醫結合雜志,2019,29(7):79-81.
[13]王丹丹,王琛,郭奧林.椎體成形術后再發骨折的臨床研究進展[J].世界最新醫學信息文摘,2018,18(A2):130,133.
[14]丁小力,王燕,閆海珠,等.椎體成形術后鄰椎新發骨折特征與相關因素分析[J].寧夏醫學雜志,2018,40(12):1193-1195.
[15]梅治,李青,趙成毅,等.經皮椎體成形術后非手術椎體再發骨折的危險因素分析[J].中國醫刊,2018,53(4):397-400.
(收稿日期:2019-06-26) (本文編輯:張爽)
①北京市懷柔區中醫醫院 北京 101400
通信作者:張偉