圍手術期腸內外聯合營養支持對老年結直腸癌患者預后、胃腸道菌群及免疫功能的影響分析
戴劍 杜金林 金晰函
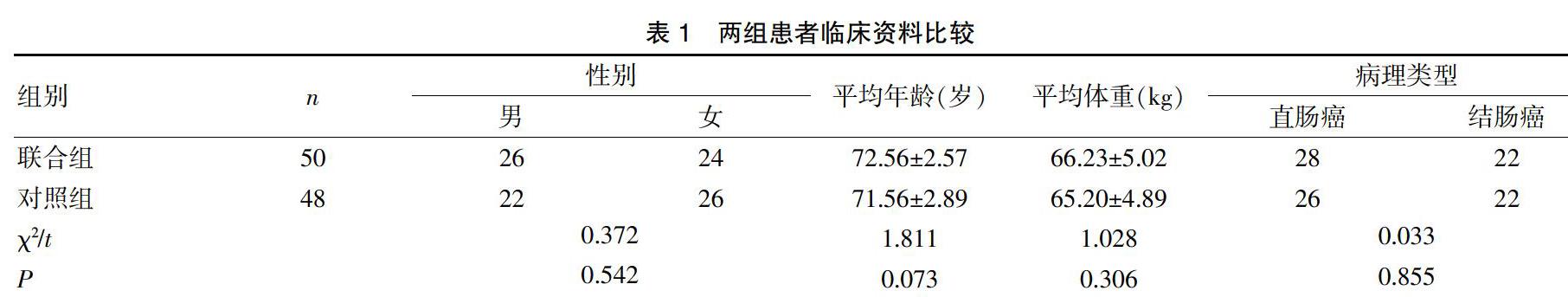

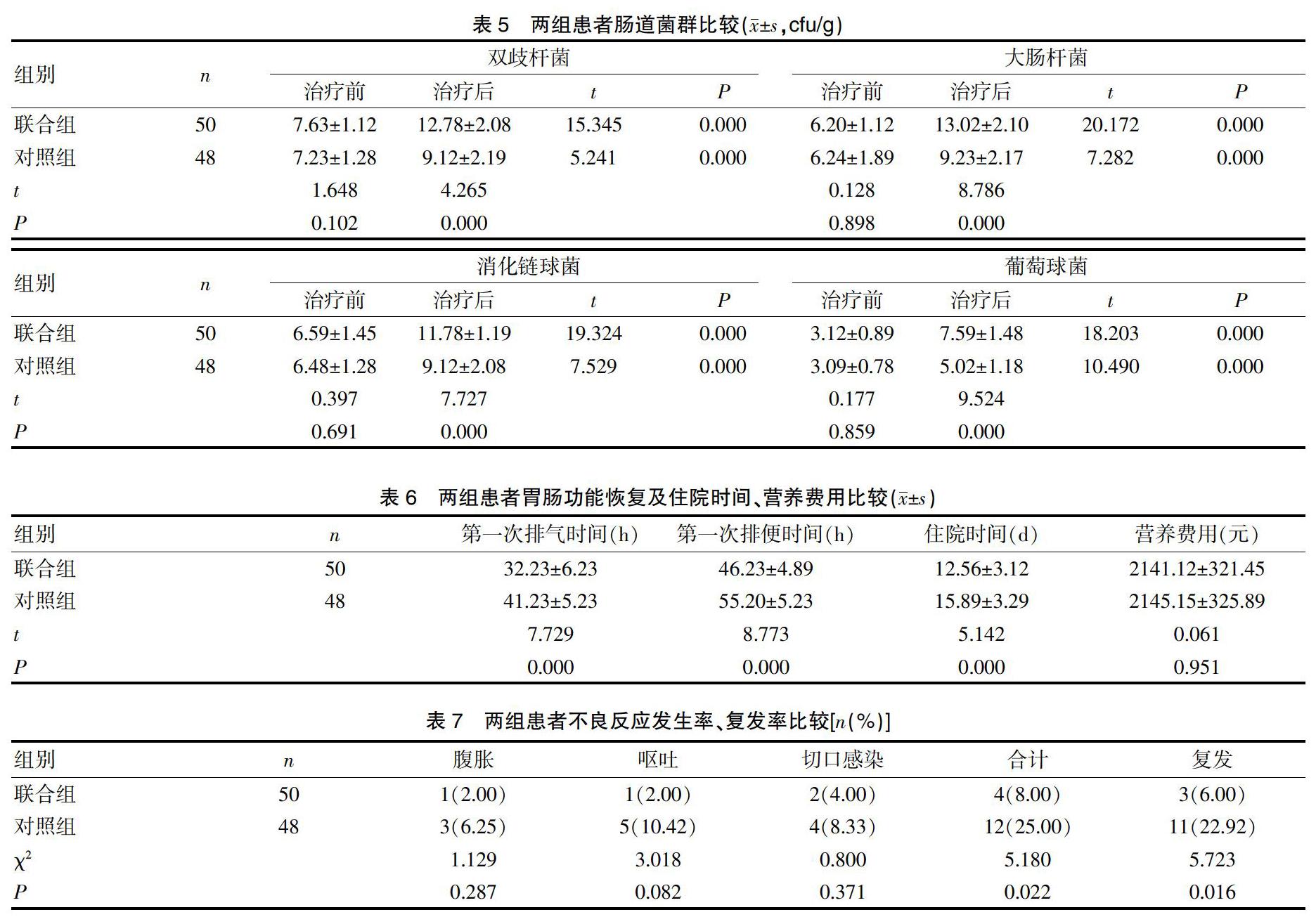
[摘要] 目的 探討圍術期腸內外聯合營養支持對老年結直腸癌患者預后、胃腸道菌群以及免疫功能的影響。 方法 選取2016年9月~2017年10月我院就診的老年結直腸癌患者98例,根據治療方法分為聯合組(n=50)和對照組(n=48)。對照組給予腸外營養干預,聯合組給予腸內營養聯合腸外營養干預。比較治療前后總蛋白、清蛋白、血紅蛋白、C反應蛋白(CRP)、白細胞介素-6(IL-6)、腫瘤壞死因子α(TNF-α)、免疫球蛋白A(IgA)、免疫球蛋白G(IgG)、免疫球蛋白M(IgM)、腸道菌群變化,記錄患者胃腸功能、住院時間、營養費用,比較不良反應、復發率發生情況。 結果 治療后,兩組患者總蛋白、清蛋白、血紅蛋白均有提高,聯合組高于對照組(P<0.05);治療后,兩組患者炎性因子CRP、IL-6、TNF-α表達均有提高,聯合組表達水平低于對照組(P<0.05);治療后,患者免疫功能表達水平均有提高,聯合組高于對照組(P<0.05)。治療后,聯合組患者雙歧桿菌、大腸桿菌、消化鏈球菌、葡萄球菌高于對照組(P<0.05)。治療后,聯合組第一次排便時間、排氣時間均早于對照組;住院時間短于對照組(P<0.05)。聯合組不良反應發生率8.00%、復發率6.00%均低于對照組25.00%、22.92%(P<0.05)。 結論 給予老年結直腸癌患者圍術期腸內外營養支持,可改善免疫功能,降低炎癥反應,糾正胃腸道菌群失調,降低營養費用、不良反應發生率、復發率,改善預后。
[關鍵詞] 圍術期;腸內外營養;結直腸癌;胃腸道菌群;免疫功能
[中圖分類號] R735.34? ? ? ? ? [文獻標識碼] A? ? ? ? ? [文章編號] 1673-9701(2020)14-0018-05
[Abstract] Objective To investigate the effect of perioperative enteral and parenteral nutrition support on the prognosis, gastrointestinal flora and immune function of elderly patients with colorectal cancer. Methods A total of 98 elderly patients with colorectal cancer who were treated in our hospital from September 2016 to October 2017 were enrolled. According to the treatment, they were divided into the combined group(n=50) and the control group(n=48). The control group was given parenteral nutrition intervention, and the combined group was given enteral nutrition combined with parenteral nutrition intervention. The changes of total protein, albumin, hemoglobin, C-reactive protein(CRP), interleukin-6(IL-6), tumor necrosis factor alpha(TNF-α), immunoglobulin A(IgA), immunoglobulin Protein G(IgG), immunoglobulin M(IgM) and intestinal flora before and after treatment were compared. The gastrointestinal function, hospitalization time and nutritional costs were recorded. The adverse reactions and recurrence rates were compared. Results After treatment, the total protein, albumin and hemoglobin were increased in the two groups. The above indexes of the combined group were higher than those of the control group(P<0.05). The expression of inflammatory factors CRP, IL-6 and TNF-α in both groups were improved after treatment. The expression levels of the combined group were lower than those of the control group(P<0.05). After treatment, the expression level of immune function was increased in both groups, and the expression level of combined group was higher than that in the control group(P<0.05). After treatment, Bifidobacterium, Escherichia coli, Streptococcus mutans and Staphylococcus were higher in the combined group than those in the control group(P<0.05). After treatment, the first defecation time and exhaust time of the combined group were earlier than those of the control group, and the hospitalization time in the combined group was shorter than that in the control group(P<0.05). The incidence of adverse reactions and the recurrence rate was 8.00% and 6.00% in the combined group, which was lower than that of the control group(25.00% and 22.92%)(P<0.05). Conclusion Perioperative enteral and parenteral nutrition support in elderly patients with colorectal cancer can improve immune function, reduce inflammatory response, correct gastrointestinal flora imbalance. And it can reduce nutritional costs, adverse reaction rate and recurrence rate, and improve prognosis.
2.5兩組患者胃腸功能恢復及住院時間、營養費用比較
治療后,聯合組患者第一次排便時間、第一次排氣時間均早于對照組(P<0.05);聯合組患者住院時間短于對照組(P<0.05);兩組患者營養費用對比差異無統計學意義(P>0.05),見表6。
2.6 兩組患者不良反應發生率、復發率比較
治療期間,兩組患者均有出現腹脹、嘔吐、切口感染等不良反應,聯合組發生率8.00%明顯低于對照組發生率25.00%(P<0.05);對患者進行1年隨訪,聯合組復發率6.00%低于對照組22.92%(P<0.05),見表7。
3討論
結直腸癌是消化道惡性腫瘤之一,隨著經濟不斷發展,人們飲食習慣的改變,結直腸癌的發病率逐年呈上升趨勢[7]。結直腸癌不僅會影響胃腸道消化功能,導致機體蛋白下降,同時也會造成患者營養不良,若長期治療無效,可損傷患者免疫功能,導致患者病情進一步加重。因此必須給予患者有效營養干預,改善患者機體免疫功能、營養不良狀態[8-9]。
營養狀態是機體產生抵抗能力、組織生長修復能力以及維持機體正常生理的一種物質基礎,因此給予結直腸癌患者圍術期營養支持尤為重要[10]。臨床營養支持主要包括腸內營養、腸外營養2種方法,但是長期腸外營養支持會損傷腸黏膜,造成腸內細菌移位,導致患者術后不良反應增加[11]。腸內營養是臨床上比較常用的營養支持,與腸外營養聯合,可優勢互補,不僅能夠提高機體免疫能力,同時也可降低不良反應發生率,縮短患者住院時間,促進患者病情康復[12-13]。本研究顯示,給予患者腸內外營養聯合治療后,患者血清總蛋白、清蛋白、血紅蛋白改善效果均優于采用單一腸外營養支持患者。分析原因在于:腸內營養更加符合人體正常生理代謝功能需求,符合小腸的吸收特點,可盡早被吸收利用。TNF-α為機體處于應激反應時的炎性介質,與機體炎性水平呈正相關;CRP屬于急性時相反應蛋白,為炎性反應的敏感指標;IL-6在機體免疫應答中占有重要地位,當機體組織受到創傷時,TNF-α、IL-6、CRP表達水平均異常上升,加重患者病情[14-15]。本結果顯示,給予患者結直腸癌患者圍術期腸內外營養支持,患者TNF-α、IL-6、CRP等表達水平雖有上升,但明顯低于單一腸外營養支持患者,表明圍術期給予結直腸癌患者腸內外營養干預,能夠改善機體炎性反應。
研究顯示[16-17],結直腸癌患者術前均有不同程度免疫功能低下,加之手術、飲食受限的影響,導致患者機體免疫功能進一步下降,如何緩解免疫功能抑制現象、穩定機體內外環境是圍術期面臨的難題。本研究結果表明,給予患者腸內外營養支持后,患者IgA、IgG、IgM等免疫功能指標表達水平均有提高,且明顯高于腸外營養支持患者,證實腸內營養與腸外營養聯合支持更能有效改善機體免疫功能,促進患者病情好轉。本研究證實,給予患者腸內外營養支持,患者排氣時間、排便時間均早于單一腸外營養支持患者,且患者住院時間短。原因在于:腸內外營養支持能夠有效穩定腸道內外環境,促進腸道蠕動、分泌、吸收,獲取營養,促進病情好轉。研究顯示[18-20],結直腸癌的發生、發展與飲食習慣導致的腸道內環境改變密切相關,而腸道菌群是構成腸道內環境的重要因素,結直腸癌患者術前腸道菌群在種類、數量、比例等方面均會發生巨大變化,如雙歧桿菌顯著減少等。本次結果顯示,給予患者腸內外營養支持,患者雙歧桿菌、大腸桿菌、消化鏈球菌、葡萄球菌均有改善,且效果優于采用單一腸外營養支持患者,表明腸內外營養支持可有效調節結直腸癌患者腸道內菌群失衡。此外,本結果證實,腸內外營養聯合支持,患者不良反應發生率8.00%低于單一腸外營養支持患者,復發率6.00%低于腸外營養支持患者,表明腸內外營養聯合支持可降低患者術后不良反應,降低疾病復發率,改善患者預后。
綜上所述,給予老年結直腸癌患者圍術期腸內外營養支持,可改善患者營養狀況,提高免疫功能,降低炎癥反應,有效糾正胃腸道菌群失調,縮短患者住院時間,降低營養費用、不良反應發生率、復發率,改善患者預后。
[參考文獻]
[1] 何琪. 術后早期經口腸內營養對結直腸癌患者術后免疫和腸黏膜屏障的影響[J]. 中國中西醫結合消化雜志,2016(4):292-294.
[2] Wang H,Zuo L,Zhao J,et al. Impact of Preoperative Exclusive Enteral Nutrition on Postoperative Complications and Recurrence After Bowel Resection in Patients with Active Crohns Disease[J]. World Journal of Surgery,2016,40(8):1-8.
[3] Iliopoulos I,Burke R,Hannan R,et al. Preoperative intubation and lack of enteral nutrition are associated with prolonged stay after arterial switch operation[J]. Pediatric Cardiology,2016,37(6):1-7.
[4] Perinel J,Mariette C,Dousset B,et al. Early enteral versus total parenteral nutrition in patients undergoing Pancreaticoduodenectomy:A randomized multicenter controlled trial (Nutri-DPC)[J]. Annals of Surgery,2016,264(5):731-735.
[5] 李積廣,余剛. 圍手術期FTS聯合營養風險篩查對結直腸癌患者手術效果的影響[J]. 貴州醫科大學學報,2017, 13(2):198-201.
[6] Jankowski M,Lasjankowska M,Sousak M,et al. Contemporary enteral and parenteral nutrition before surgery for gastrointestinal cancers:a literature review[J]. World Journal of Surgical Oncology,2018,16(1):94-98.
[7] 王飛. 丙泊酚聯合順式阿曲庫銨對老年結直腸癌患者圍手術期外周血T淋巴細胞亞群的影響[J]. 實用癌癥雜志,2017,32(3):408-410.
[8] Heerasing N,Thompson B,Hendy P,et al. Exclusive enteral nutrition provides an effective bridge to safer interval elective surgery for adults with Crohn's disease[J]. Alimentary Pharmacology & Therapeutics,2017,45(5):660-669.
[9] 孫廣榮,鄒萍,董瑞強,等. 圍手術期營養支持對結直腸癌患者腫瘤細胞cyclin D1表達及復發轉移的影響[J]. 實用癌癥雜志,2017,32(8):1328-1330.
[10] Hara T,Kubo A,Kogure E,et al. Impact of the difference in surgical site on the physique in gastrointestinal tract cancer patients[J]. Journal of Physical Therapy Science,2016,28(1):67-69.
[11] 張永萍. 直腸癌患者圍手術期的營養支持對術后免疫功能及并發癥發生情況的影響[J]. 結直腸肛門外科,2017, 18(1):35-38.
[12] Tan S J,Yu C,Yu Z,et al. High-fat enteral nutrition controls intestinal inflammation and improves intestinal motility after peritoneal air exposure[J]. Journal of Surgical Research,2016,201(2):408-410.
[13] 郭添羽,黃昌浩,袁偉杰,等. 術前營養風險篩查對胃癌和結腸癌患者圍手術期營養支持的臨床意義[J]. 中國現代醫學雜志,2016,26(5):119-123.
[14] Hertlein L,G?觟ss C,Fürst S,et al. Perioperative orale/enterale Immunonutrition nach Ern?覿hrungsscreening mithilfe des Nutritional Risk Screenings bei Patientinnen mit Ovarialkarzinom[J]. Geburtshilfe Und Frauenheilkunde,2016, 76(10):56-59.
[15] 蘇學艷,薛蘇娟,李曉紅,等. 添加益生菌的腸內營養對老年骨折術后患者腸道菌群變化及預后的影響[J]. 河北醫藥,2017,39(12):1776-1779.
[16] Zhang Y,Gu F,Wang F,et al. Effects of early enteral nutrition on the gastrointestinal motility and intestinal mucosal barrier of patients with burn-induced invasive fungal infection[J]. Pakistan Journal of Medical Sciences,2016,32(3):599-603.
[17] 郭永鋒,羅孔亮,韓冰,等. 胰十二指腸切除術后腸內外聯合營養與完全胃腸外營養的臨床療效比較[J]. 中國普外基礎與臨床雜志,2017,19(3):317-321.
[18] Carr AC,Rosengrave PC,Bayer S,et al. Hypovitaminosis C and vitamin C deficiency in critically ill patients despite recommended enteral and parenteral intakes[J]. Critical Care,2017,21(1):300-306.
[19] 雷婷,汪泳,于剛,等. 微生態制劑聯合早期腸內營養對重型顱腦損傷患者臨床結局指標影響的Meta分析[J].醫藥導報,2016,35(12):1364-1368.
[20] Yu HM,Tang CW,Feng WM,et al. Early Enteral Nutrition Versus Parenteral Nutrition After Resection of Esophageal Cancer:a Retrospective Analysis[J]. Indian Journal of Surgery,2017,79(1):13-18.
(收稿日期:2019-05-27)

