氧代謝指標評估膿毒癥早期急性腎損傷的臨床意義
袁滿涓 霍保善
[摘要]目的 探討氧代謝指標中心靜脈-動脈二氧化碳分壓差與動脈-中心靜脈氧含量差比值(Pv-aCO2/Ca-vO2)對膿毒癥早期急性腎損傷(AKI)的臨床意義。方法 采用前瞻性隊列研究方法,選取2019年8月~2020年1月佛山市第二人民醫院重癥醫學科收治的膿毒癥行機械通氣患者48例,根據復蘇24 h后是否發生AKI分為AKI組(n=31)和非AKI組(n=17)。分別收集患者復蘇0、12、24 h后的毛細血管再填充時間(CRT)、乳酸(Lac)、Pv-aCO2、Ca-vO2。應用二元Logistic回歸模型分析AKI的影響因素,受試者工作特征(ROC)曲線評價指標的敏感度與特異性。結果 入院時AKI組的急性生理學及慢性健康狀況評分、序貫器官衰竭評分高于非AKI組,差異有統計學意義(P<0.05),復蘇24 h后,AKI組Lac水平高于非AKI組,差異有統計學意義(P<0.05);復蘇12、24 h后,AKI組CRT長于非AKI組,差異有統計學意義(P<0.05);復蘇0、12、24 h后,AKI組Pv-aCO2/Ca-vO2高于非AKI組,差異有統計學意義(P<0.05)。應用二元Logistic回歸分析顯示,復蘇24 h后Pv-aCO2/Ca-vO2值(β=2.579,OR=13.181,95%CI=1.048~165.708,P=0.046)是膿毒癥患者早期AKI發生的獨立危險因素。ROC曲線顯示,復蘇24 h后的Pv-aCO2/Ca-vO2值預測AKI進展的曲線下面積最高,其臨界值為1.625,敏感度為83.9%,特異性為76.5%。結論 氧代謝評估對膿毒癥患者復蘇時早期AKI評估具有重要的臨床意義,其中Pv-aCO2/Ca-vO2對AKI病情進展具有較好的預測價值。
[關鍵詞]膿毒性休克;急性腎損傷;微循環與氧代謝評估;毛細血管再填充時間
[中圖分類號] R44? ? ? ? ? [文獻標識碼] A? ? ? ? ? [文章編號] 1674-4721(2020)8(b)-0010-05
[Abstract] Objective To explore the clinical significance of the ratio of the central venous-arterial carbon dioxide partial pressure difference and the arterial-central venous oxygen content difference (Pv-aCO2/Ca-vO2) to early acute renal injury (AKI) in sepsis. Methods This study was a prospective and observative cohort study. A total of 48 patients with sepsis and mechanical ventilation in the intensive care unit of Foshan Second People Hospital were enrolled into this study and their general clinical data grading scores were collected from August, 2019 to January, 2020. According to whether AKI occurred 24 h after resuscitation, they were divided into AKI group (n=31) and non-AKI group (n=17). The capillary refill time (CRT), lactate (Lac), Pv-aCO2 and Ca-vO2 were collected at 0, 12 and 24 h after resuscitation. The potential influencing factors of AKI were analyzed by binary Logistic regression model, and then the risk factors were decided. Receiver operating characteristic curve (ROC) was used to analyze the predictive value of each indexs for AKI diagnostic value at the early stage of sepsis. Results The initial score of acute physiology and chronic health and the initial score of sequential organ failure in AKI group were higher than those in the non-AKI group, the differences were statistic significant(P<0.05). At 24 h after resuscitation, the Lac level in the AKI group was higher than that of the non-AKI group, and the difference was statistically significance(P<0.05); At 12 and 24 h after resuscitation, the CRT of AKI group were longer than those of the non-AKI group, the differences were statistically significant(P<0.05); At 0, 12 and 24 h after resuscitation, the Pv-aCO2/Ca-vO2 of the AKI group were higher than those of non-AKI group, the differences were also statistically significant(P<0.05). The results of binary Logistic regression analysis showed that the value of Pv-aCO2/Ca-vO2 (β=2.579, OR=13.181, 95%CI=1.048-165.708, P=0.046) was an independent risk factor of AKI in early sepsis. ROC curve showed that 24 h after resuscitation, the cutoff value of Pv-aCO2/Ca-vO2 was 1.625, the sensitivity was 83.9% while the specificity was 76.5%. Conclusion Oxygen metabolism assessment has important clinical significance for early AKI assessment during resuscitation. Among them, Pv-aCO2/Ca-vO2 has a good predictive value for the progression of AKI.
[Key words] Septic shock; Acute kidney injury; Microcirculation and oxygen metabolism evaluation; Capillary refill time
目前我國每年至少有290萬例成年急性腎損傷(AKI)患者需住院治療,其中約70萬例病死,并且在臨床上有嚴重的漏診、誤診和治療不當的情況發生,整體診療水平亟待提高[1]。AKI在膿毒癥住院患者中具有較高的發生率和病死率,分別為26.9%和11.0%,加強對膿毒癥患者AKI的防治對改善患者預后具有重要意義[2]。目前研究認為微循環灌注異常與氧代謝障礙是影響膿毒性休克腎損傷的兩個重要因素,因此對膿毒癥患者早期微循環和氧代謝的評估是治療膿毒性AKI的關鍵[3]。氧輸送參數之一的中心靜脈-動脈二氧化碳分壓差與動脈-中心靜脈氧含量差比值(Pv-aCO2/Ca-vO2)是評價無氧代謝的指標,其理論依據是組織消耗的氧減少,所生成的二氧化碳也相應減少,但同時組織無氧代謝時會繼發生成二氧化碳,從而出現二氧化碳減少程度小于氧減少程度的情況即表現為Pv-aCO2/Ca-vO2升高[4]。由于該指標可以較好地評估微循環灌注以及細胞無氧代謝情況,目前已經運用到膿毒癥休克患者復蘇后的病情和預后的評估中[5]。本項目旨在探討Pv-aCO2/Ca-vO2對膿毒癥早期患者AKI發生的診斷價值。
1資料與方法
1.1一般資料
選取2019年8月~2020年1月佛山市第二人民醫院重癥醫學科收治的48例膿毒癥患者。納入標準:①符合2016年美國重癥醫學會頒布的膿毒癥和膿毒性休克管理的國際指南中的相關診斷標準[6];②年齡>18歲且<90歲;③需行有創機械輔助通氣。排除標準:①存在通氣氧合嚴重異常者,即吸氧濃度(FiO2)>80%,二氧化碳分壓>60 mmHg,呼氣末氣道正壓>10 cmH2O;②慢性腎功能不全;③患者家屬拒絕簽署知情同意書;④患者入院24 h內死亡或自動出院。本研究符合醫學倫理學標準,經佛山市第二人民醫院倫理委員會批準,所有檢測和治療均獲得患者家屬的知情同意。
1.2方法
收集所有患者的一般臨床資料、急性生理學及慢性健康狀況評分(APACHEⅡ)、序貫器官衰竭評分(SOFA)。其中APACHEⅡ廣泛用于危重癥疾病病情分類跟預后預測,分值越高表示病情越重,預后越差。APACHEⅡ包括急性生理評分、年齡評分及慢性健康評分三部分,最后得分為三者之和。理論最高分71分,分值越高病情越嚴重[7]。SOFA主要內容是評估臟器功能,目的是描述多器官衰竭發生發展并評價發生率,0~48分,分數越高提示預后越差[8]。所有患者均按照膿毒癥診治指南[6]給予相應基礎治療,包括盡早合理應用抗感染藥物、機械通氣、積極優化血流動力學治療、鎮靜鎮痛、營養支持等。由于復蘇需要,治療前均留置頸內或鎖骨下靜脈導管,并經股動脈放置動脈導管,進行有創監測血壓。監測內容包括0 h及復蘇12 h,24 h的CRT、Lac、Pv-aCO2、Ca-vO2。根據腎臟病預后組織在2012年提出AKI診斷標準[9],將復蘇24 h后的患者分為AKI組和非AKI組。
1.3統計學方法
采用SPSS25.0統計學軟件進行數據分析。計量資料符合正態分布的用均數±標準差(x±s)表示,非正態分布的計量資料改用中位數(四分位數)[M(Q25,Q75)]表示,符合正態方差齊時采用獨立樣本t檢驗,不符合正態或方差不齊的計量資料用Mann-Whitney U檢驗;計數資料采用χ2檢驗。應用二元Logistic回歸模型分析AKI的影響因素;應用受試者工作特征(ROC)曲線確定診斷臨界值。P<0.05為差異有統計學意義。
2結果
2.1兩組一般資料的比較
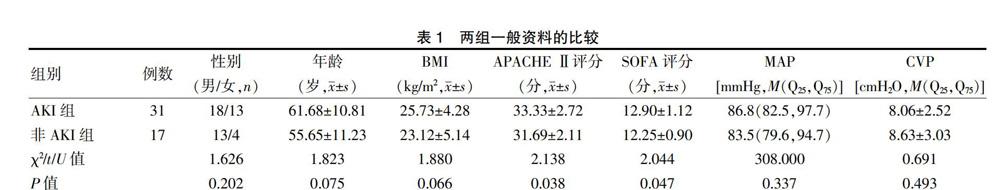
兩組性別、年齡、體重指數(BMI)、動脈壓(MAP)、中心靜脈壓(CVP)比較,差異均無統計學意義(P>0.05)。AKI組的APACHEⅡ、SOFA評分高于非AKI組,差異有統計學意義(P<0.05)(表1)。
2.2 AKI組和非AKI組各時間段微循環指標的比較
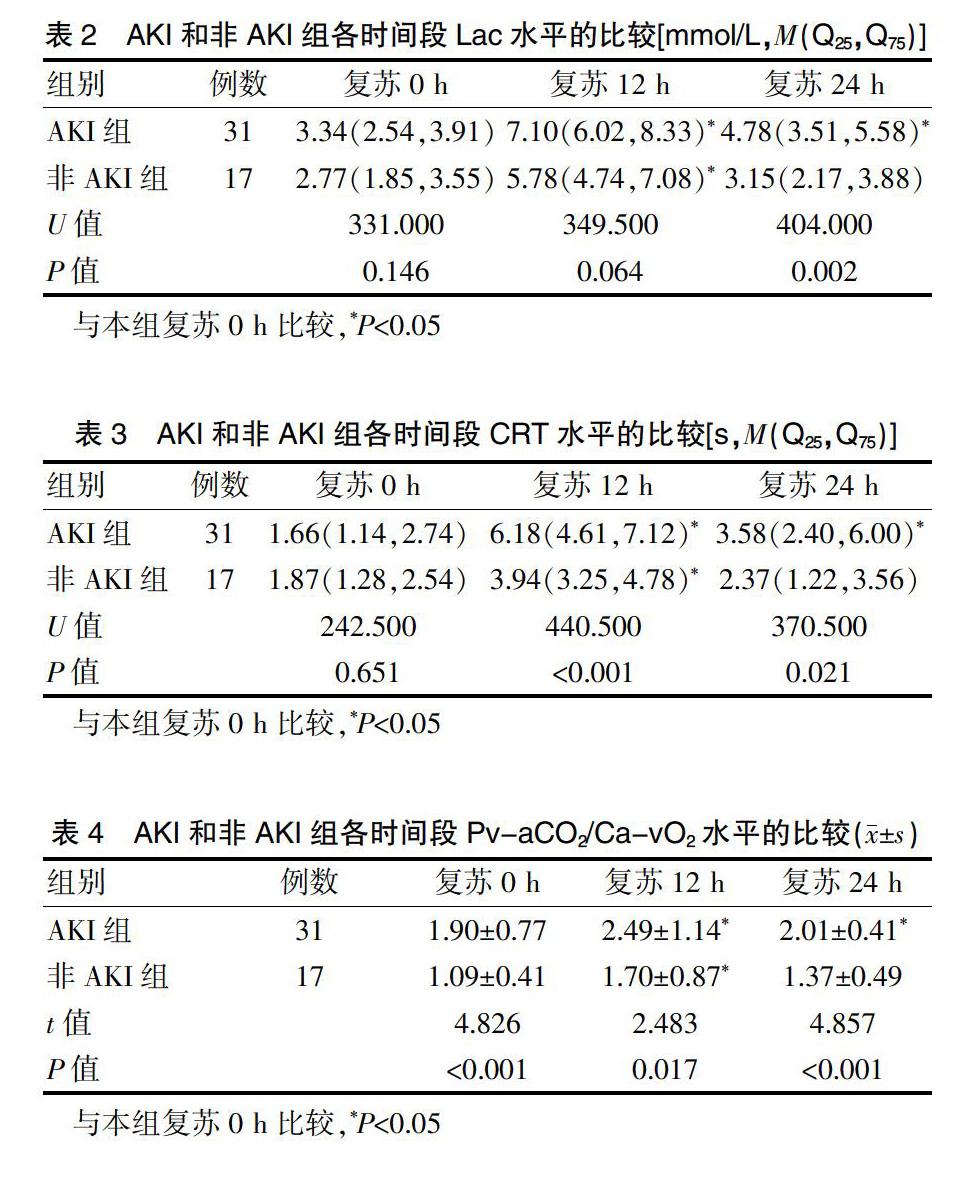
復蘇24 h后,AKI組Lac水平高于非AKI組,差異有統計學意義(P<0.05)。復蘇12、24 h,AKI組CRT長于非AKI組,差異有統計學意義(P<0.05)。復蘇0、12、24 h,AKI組Pv-aCO2/Ca-vO2均高于非AKI組,差異有統計學意義(P<0.05)。組內比較,與復蘇0 h比較,AKI組12、24 h兩個時間段的Lac、CRT、Pv-aCO2/Ca-vO2微循環指標均升高,差異有統計學意義(P<0.05)。與復蘇0 h比較,非AKI組復蘇12 h的Lac、CRT、Pv-aCO2/Ca-vO2微循環指標均升高,差異有統計學意義(P<0.05);非AKI組復蘇24 h后的Lac、CRT、Pv-aCO2/Ca-vO2微循環指標與復蘇0 h比較,差異無統計學意義(P>0.05)(表2~4)。
2.3膿毒癥患者早期AKI發生的二元Logistic回歸分析
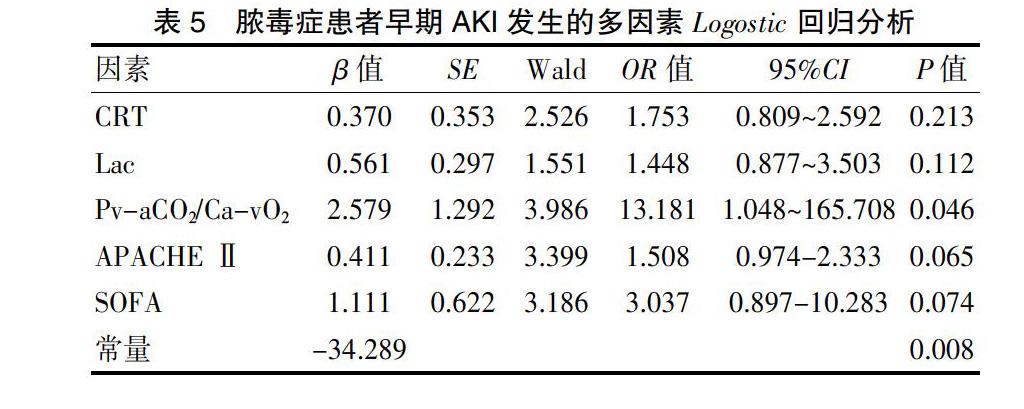
以AKI和非AKI為因變量,以CRT、CRT、Lac、Pv-aCO2/Ca-vO2、APACHE Ⅱ、SOFA作為自變量進行二元Logistic回歸分析,結果顯示Pv-aCO2/Ca-vO2是膿毒癥早期AKI發生的獨立危險因素(P<0.05)(表5)。
2.4氧代謝標預測AKI的敏感度、特異性
復蘇24 h后,CRT、Lac水平、Pv-aCO2/Ca-vO2對AKI的預測價值:根據約登指數,Pv-aCO2/Ca-vO2預測復蘇后24 h內AKI進展的臨界值為1.625,敏感度為83.9%,特異性為76.5%(表6、圖1)。
3討論
AKI是膿毒癥患者最常見的并發癥,是膿毒癥患者死亡風險增加的危險因素。腎血流不足導致的腎小球與腎小管細胞壞死曾被認為是AKI的主要發生機制。近期研究證實,休克患者大循環復蘇后,盡管腎血流恢復正常甚至增加,AKI仍會發生[10]。膿毒性休克患者完成早期目標導向治療并不能降低AKI的發生[11]。腎組織微循環異常與線粒體功能障礙是現在研究證實的AKI發生、發展的重要機制,也是目前膿毒性休克治療進一步改善預后的難點[12]。休克早期復蘇后中心靜脈血氧飽和度正常并不能保證組織灌注和細胞氧代謝的恢復,復蘇深入到微循環和細胞氧代謝已成為共識[13-14]。在治療過程種,也發現膿毒癥早期患者Lac、CRT等微循指標異常。因此微循環與氧代謝評估成為膿毒性AKI評估的關鍵。
有學者發現,Pv-aCO2/Ca-vO2可預測快速增加氧輸送后氧消耗的反應,Pv-aCO2/Ca-vO2異常升高提示存在無氧代謝,氧輸送-氧消耗呈依賴關系,增加氧輸送可以相應增加氧消耗[5,15]。作為反映組織缺氧的一項敏感指標,與Lac具有良好的相關性,且能較為準確地預測休克患者液體復蘇后氧代謝的變化。Monnet等[5]研究提示,Pv-aCO2/Ca-vO2從理論上作為組織缺氧指標比血漿Lac濃度反應更早、更快、更純粹。膿毒癥性AKI通常發生在入住ICU后24 h內[16-17],在膿毒癥休克患者中,約68%的AKI發生在膿毒癥診斷后的6 h內[18]。國內現見1例研究,使用氧代謝指標來評估膿毒性休克患者的AKI發生情況[1]。然而入住ICU膿毒癥患者不完全出現大循環衰竭,微循環障礙反而多見。早期未發生休克前,預測到AKI的可能性及嚴重程度更具臨床意義。本研究中也觀察到,入院時AKI組的APACHEⅡ、SOFA評分高于非AKI組,差異有統計學意義(P<0.05)。復蘇24 h后,AKI組Lac水平高于非AKI組,差異有統計學意義(P<0.05);復蘇12、24 h,AKI組CRT長于非AKI組,差異有統計學意義(P<0.05);復蘇0、12、24 h,AKI組Pv-aCO2/Ca-vO2均高于非AKI組,差異有統計學意義(P<0.05);組內比較,與復蘇0 h比較,AKI組12、24 h兩個時間段的Lac、CRT、Pv-aCO2/Ca-vO2微循環指標均升高,差異有統計學意義(P<0.05)。與復蘇0 h比較,非AKI組復蘇12 h的Lac、CRT、Pv-aCO2/Ca-vO2微循環指標均升高,差異有統計學意義(P<0.05);與復蘇0 h比較,非AKI組復蘇24 h后的Lac、CRT、Pv-aCO2/Ca-vO2微循環指標變化不大,差異無統計學意義(P>0.05)。說明AKI組與非AKI組復蘇后12 h與治療前相比效果明顯,經過復蘇治療24 h后,非AKI組指標改善更明顯。說明復蘇改善了兩組患者的病情,非AKI組患者可能因為基礎情況良好,微循環指標理想,復蘇后效果更為理想。相對于其他膿毒癥患者,并發了AKI的患者病情評分明顯高于非AKI患者,同時他們的微循環指標也明顯降低,說明AKI的發生嚴重降低了患者生理健康指標,并且加重了他們的多臟器負擔。同時通過多因素Logostic回歸分析顯示,Pv-aCO2/Ca-vO2是膿毒癥早期AKI的獨立危險因素;根據約登指數,Pv-aCO2/Ca-vO2預測復蘇后24 h內AKI進展的臨界值為1.625,敏感度為83.9%,特異性為76.5%。可以較好分辨出AKI高風險患者,早期及時予以針對性的治療。
綜上,AKI在膿毒癥早期具有較高的發病率,微循環和氧代謝評估對膿毒癥早期AKI評估具有重要的臨床意義,其中Pv-aCO2/Ca-vO2對AKI病情進展具有較好的預測價值。
[參考文獻]
[1]Li Y,Guolan X,Li W,et al.Acute kidney injury in China:a cross-sectional survey[J].Lancet (London,England),2015, 386(10002):1465-1471.
[2]Kaddourah A,Basu RK,Bagshaw SM,et al.Epidemiology of acute kidney injury in critically ill children and young adults[J].N Engl J Med,2017,376(1):11-20.
[3]Seely KA,Holthoff JH,Burns ST,et al.Hemodynamic changes in the kidney in a pediatric rat model of sepsis-induced acute kidney injury[J].Am J Physiol Renal Physiol,2011,301(1):F209-217.
[4]Mesquida J,Saludes P,Gruartmoner G,et al.Central venous-to-arterial carbon dioxide difference combined with arterial-to-venous oxygen content difference is associated with lactate evolution in the hemodynamic resuscitation process in early septic shock[J].Crit Care,2015,19(1):126.
[5]Monnet X,Julien F,Ait-Hamou N,et al.Lactate and venoarterial carbon dioxide difference/arterial-venous oxygen difference ratio,but not central venous oxygen saturation,predict increase in oxygen consumption in fluid responders[J].Crit Care Med,2013,41(6):1412-1420.
[6]Rhodes A,Evans LE,Alhazzani W,et al.Surviving sepsis campaign:international guidelines for management of sepsis and septic shock[J].Crit Care Med,2017,45(3):486-552.
[7]LeGall JR,Loirat P,Alpérovitch A.APACHE II-a severity of disease classification system[J].Crit Care Med,1986,14(8):754-755.
[8]Le Gall JR,Lemeshow S,Saulnier F.A new Simplified Acute Physiology Score(SAPS Ⅱ) based on a European/North American multicenter study[J].JAMA,1993,270(24):2957-2963.
[9]Disease K,Improving Global Outcomes KDIGO.Acute Kidney Injury Work Group:KDIGO clinical practice guideline for acute kidney injury[J].Kidney International Supplement,2012,2(1):1-138.
[10]Gomez H,Ince C,De Backer D,et al.A unified theory of sepsis-induced acute kidney injury:inflammation,microcirculatory dysfunction,bioenergetics,and the tubular cell adaptation to injury[J].Shock,2014,41(1):3-11.
[11]Wasim A,Memon Javed I,Rifat R,et al.Outcome of patients with acute kidney injury in severe sepsis and septic shock treated with early goal-directed therapy in an intensive care unit[J].Saudi J Kidney Dis Transpl,2014,25(3):544-551.
[12]Zuk A,Bonventre JV.Acute kidney injury[J].Annu Rev Med,2016,67:293-307.
[13]ARISE Investigators,ANZICS Clinical Trials Group,Peake SL,et al.Goal-directed resuscitation for patients with early septic shock[J].N Engl J Med,2014,371(16):1496-506.
[14]ProCESS Investigators,Yealy DM,Kellum JA,et al.A randomized trial of protocol-based care for early septic shock[J].N Engl J Med,2014,370(18):1683-1693.
[15]Mallat J,Lemyze M,Meddour M,et al.Ratios of central venous-to-arterial carbon dioxide content or tension to arteriovenous oxygen content are better markers of global anaerobic metabolism than lactate in septic shock patients[J].Ann Intensive Care,2016,6(1):10.
[16]Lima RS,Marques CN,Silva Júnior GB,et al.Comparison between early and delayed acute kidney injury secondary to infectious disease in the intensive care unit[J].Int Urol Nephrol,2008,40(3):731-739.
[17]Bagshaw SM,Lapinsky S,Dial S,et al.Acute kidney injury in septic shock:clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy[J].Intensive Care Med,2009,35(5):871-881.
[18]Sood Manish M,Anne SL,Julie H,et al.Early reversible acute kidney injury is associated with improved survival in septic shock[J].J Crit Care,2014,29(5):711-717.
(收稿日期:2020-04-07)

