腹腔鏡直腸癌根治術(shù)中保留左結(jié)腸動(dòng)脈的前瞻性隨機(jī)對(duì)照研究
胡軍 羅俊峰 周文斌 李包根 呂玉良

【摘要】 目的:探討腹腔鏡直腸癌根治術(shù)中保留左結(jié)腸動(dòng)脈(LCA)的安全性和可行性。方法:采用前瞻性隨機(jī)對(duì)照試驗(yàn),依據(jù)隨機(jī)數(shù)字表法,將2018年6月-2020年3月于本院行直腸癌手術(shù)患者分為試驗(yàn)組和對(duì)照組,每組30例。試驗(yàn)組行保留LCA的直腸癌根治術(shù),對(duì)照組行距離IMA根部1 cm的高危結(jié)扎。比較兩組手術(shù)時(shí)間、術(shù)中出血量、遠(yuǎn)端和近端腸管切除長(zhǎng)度、脾曲游離例數(shù)、預(yù)防性造口例數(shù)、住院時(shí)間、吻合口漏、淋巴結(jié)清掃總數(shù)、253組淋巴結(jié)等指標(biāo)。結(jié)果:所有患者手術(shù)順利,且圍術(shù)期無(wú)死亡。兩組術(shù)中出血量、手術(shù)時(shí)間、遠(yuǎn)端腸管切除長(zhǎng)度、清除的淋巴結(jié)總數(shù)目、清除的253組淋巴結(jié)數(shù)目及253組淋巴結(jié)癌轉(zhuǎn)移陽(yáng)性率比較,差異均無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05)。試驗(yàn)組游離脾曲例數(shù)、預(yù)防性造口例數(shù)、近端腸管切除長(zhǎng)度均低于對(duì)照組,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05)。兩組均未出現(xiàn)吻合口出血及切口感染。試驗(yàn)組無(wú)吻合口漏,對(duì)照組4例吻合口漏,兩組比較,差異有統(tǒng)計(jì)學(xué)意義(P<0.05)。試驗(yàn)組術(shù)后首次排氣時(shí)間、術(shù)后住院時(shí)間均短于對(duì)照組,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05)。結(jié)論:腹腔鏡下直腸癌根治術(shù)中保留LCA在淋巴結(jié)清掃根治方面與不保留LCA臨床效果相當(dāng),并且有利于促進(jìn)術(shù)后腸道功能恢復(fù),降低吻合口漏,安全可行。
【關(guān)鍵詞】 直腸腫瘤 左結(jié)腸動(dòng)脈 腹腔鏡 淋巴結(jié) 吻合口漏
Prospective Randomized Controlled Study of Preserving Left Colonic Artery in Laparoscopic Radical Resection of Rectal Cancer/HU Jun, LUO Junfeng, ZHOU Wenbin, LI Baogen, LYU Yuliang. //Medical Innovation of China, 2021, 18(30) :-116
[Abstract] Objective: To investigate the safety and feasibility of preserving the left colon artery (LCA) during laparoscopic radical resection of rectal cancer. Method: In this prospective randomized controlled trial, patients who underwent rectal cancer surgery in our hospital from June 2018 to March 2020 were divided into experimental group and control group according to random number table method, 30 patients in each group. The experimental group was treated with lCA-preserving radical resection of rectal cancer, while the control group was treated with high-risk ligation 1 cm away from IMA root. The operative time, intraoperative blood loss, distal and proximal bowel resection length, free cases of splenic flexion, preventive stomy cases, length of hospital stay, anastomotic leakage, total number of lymph node dissection and 253 groups of lymph nodes were compared between the two groups. Result: All patients were successfully operated and no perioperative death occurred. There were no significant differences in intraoperative blood loss, operation time, distal bowel resection length, total number of lymph nodes removed, number of lymph nodes removed in 253 groups and positive rate of lymph node metastasis in 253 groups between the two groups (P>0.05). The number of free splenic flexion, the number of preventive colostomy and the length of proximal bowel resection in experimental group were lower than those in control group, the differences were statistically significant (P<0.05). There was no anastomotic bleeding or incision infection in the two groups. There was no anastomotic leakage in the experimental group and 4 cases anastomotic leakage in the control group, the difference between the two groups was statistically significant (P<0.05). The first postoperative exhaust time and postoperative hospitalization time of the experimental group were shorter than those of the control group, the differences were statistically significant (P<0.05). Conclusion: The clinical effect of preserving LCA in laparoscopic radical resection of rectal cancer is similar to that of not preserving LCA in lymph node dissection and radical resection, and it is safe and feasible to promote postoperative intestinal function recovery and reduce anastomotic leakage.
[Key words] Rectal neoplasms Left colic artery Laparoscopy Lymph gland Anastomotic leakage
First-author’s address: Yichun People’s Hospital, Yichun 336000, China
doi:10.3969/j.issn.1674-4985.2021.30.027
直腸癌是我國(guó)常見(jiàn)的惡性腫瘤之一,其死亡主要原因是局部復(fù)發(fā)和遠(yuǎn)處轉(zhuǎn)移[1]。進(jìn)展期直腸癌首選的手術(shù)方式為腹腔鏡下直腸癌根治術(shù),術(shù)中對(duì)腸系膜下動(dòng)脈(inferior mesenteric artery,IMA)的處理分別為保留左結(jié)腸動(dòng)脈(left colic artery,LCA)的低位結(jié)扎和在IMA根部高位結(jié)扎兩種方式[2]。理論上保留LCA會(huì)使殘留腸管血運(yùn)更加豐富,降低吻合口漏的發(fā)生率[3]。但目前對(duì)于保留LCA能否同時(shí)清掃253組淋巴結(jié)、減少吻合口漏等仍存在爭(zhēng)議。文獻(xiàn)[4-5]多為回顧性研究,缺少隨機(jī)對(duì)照研究,本研究旨在通過(guò)設(shè)計(jì)隨機(jī)對(duì)照試驗(yàn),探討腹腔鏡直腸癌根治術(shù)中保留LCA的可行性與安全性,現(xiàn)報(bào)道如下。
1 資料與方法
1.1 一般資料 采用前瞻性隨機(jī)對(duì)照試驗(yàn),依據(jù)隨機(jī)數(shù)字表法,將2018年6月-2020年3月于本院行直腸癌手術(shù)患者分為試驗(yàn)組和對(duì)照組,每組30例。納入標(biāo)準(zhǔn):(1)腸鏡和病理學(xué)證實(shí)為直腸惡性腫瘤;(2)影像學(xué)檢查無(wú)遠(yuǎn)處轉(zhuǎn)移;(3)未行新輔助治療;(4)年齡20~70歲。排除標(biāo)準(zhǔn):(1)嚴(yán)重肝腎心肺功能障礙,不宜行手術(shù)治療;(2)急癥手術(shù);(3)術(shù)前多學(xué)科討論評(píng)估出現(xiàn)遠(yuǎn)處轉(zhuǎn)移,不宜手術(shù)治療;(4)術(shù)前已決定行Miles手術(shù)。本研究通過(guò)本院倫理委員會(huì)審批,患者及家屬術(shù)前均簽署知情同意書(shū)。
1.2 方法
1.2.1 手術(shù)方法 術(shù)前口服和爽(聚乙二醇電解質(zhì)散)2盒行機(jī)械性腸道準(zhǔn)備,禁水4 h。氣管插管全身麻醉,兩腿分開(kāi)頭低腳高位,臍上1 cm建立觀察孔,常規(guī)行5孔法。切開(kāi)乙狀結(jié)腸系膜根部,進(jìn)入Toldts間隙并充分拓展,避免損傷左側(cè)輸尿管、生殖血管和神經(jīng)。試驗(yàn)組:術(shù)中保留LCA的低位結(jié)扎。清除253組淋巴結(jié),解剖IMA及屬支,保留LCA,切斷直腸上動(dòng)脈和乙狀結(jié)腸動(dòng)脈,保護(hù)好腹下神經(jīng)叢,相同水平離斷腸系膜下靜脈。對(duì)照組:距離IMA根部1 cm的高危結(jié)扎。距離IMA根部1 cm結(jié)扎、切斷血管。兩組其余步驟遵循全直腸系膜切除術(shù)(TME)原則進(jìn)行操作。腫瘤與上切緣的距離在10 cm以上,下切緣與腫瘤下緣之間的距離不少于2 cm,術(shù)中冰凍檢查確保切緣陰性。3-0可吸收線(xiàn)縫合吻合口,放置骶前引流管和肛管。如術(shù)中發(fā)現(xiàn)吻合口血運(yùn)障礙,則行末端回腸雙腔造口。
1.2.2 術(shù)后處理 手術(shù)當(dāng)日禁食,術(shù)后第1天進(jìn)流食,如患者無(wú)不適,逐漸增加進(jìn)食量,術(shù)后第4天起半流質(zhì)飲食,如無(wú)嚴(yán)重并發(fā)癥,術(shù)后7~10 d出院。
1.3 觀察指標(biāo) 比較兩組術(shù)中出血量、手術(shù)時(shí)間、腫瘤遠(yuǎn)端及近端腸管切除長(zhǎng)度、游離脾曲情況、預(yù)防性腸造口例數(shù)、清除的淋巴結(jié)總數(shù)和253組淋巴結(jié)數(shù)目及253組淋巴結(jié)癌轉(zhuǎn)移陽(yáng)性率、術(shù)后首次排氣時(shí)間和住院時(shí)間、并發(fā)癥發(fā)生情況,包括吻合口漏等。
1.4 統(tǒng)計(jì)學(xué)處理 采用SPSS 18.0軟件分析處理數(shù)據(jù),計(jì)量資料以(x±s)表示,比較采用獨(dú)立樣本t檢驗(yàn),計(jì)數(shù)資料以例(%)表示,采用字2檢驗(yàn),以P<0.05為差異有統(tǒng)計(jì)學(xué)意義。
2 結(jié)果
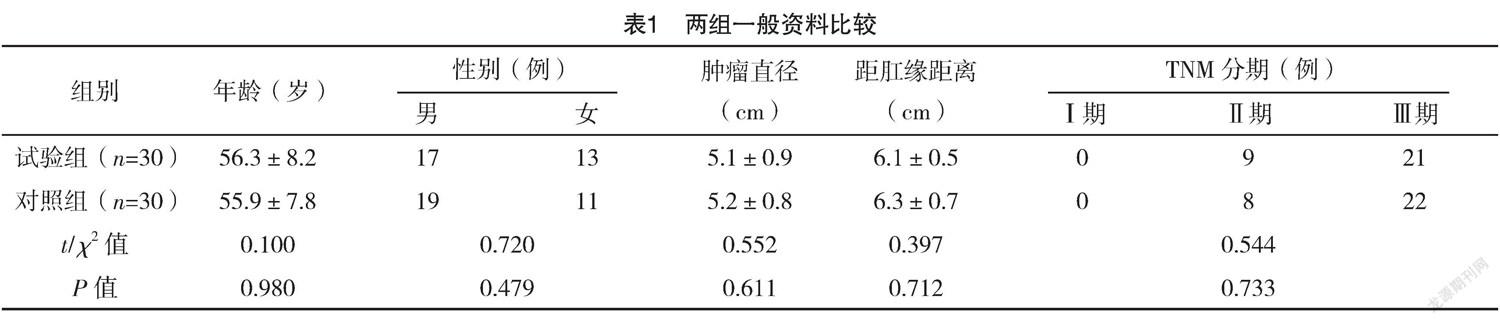
2.1 兩組一般資料比較 兩組年齡、性別、腫瘤直徑、距肛緣距離及TNM分期比較,差異均無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05),具有可比性,見(jiàn)表1。
2.2 兩組手術(shù)指標(biāo)比較 兩組手術(shù)順利完成,兩組均無(wú)中轉(zhuǎn)開(kāi)腹,圍術(shù)期無(wú)死亡。兩組術(shù)中出血量、手術(shù)時(shí)間、遠(yuǎn)端腸管切除長(zhǎng)度比較,差異均無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05);試驗(yàn)組游離脾曲例數(shù)、預(yù)防性造口例數(shù)、近端腸管切除長(zhǎng)度均低于對(duì)照組,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05)。見(jiàn)表2。
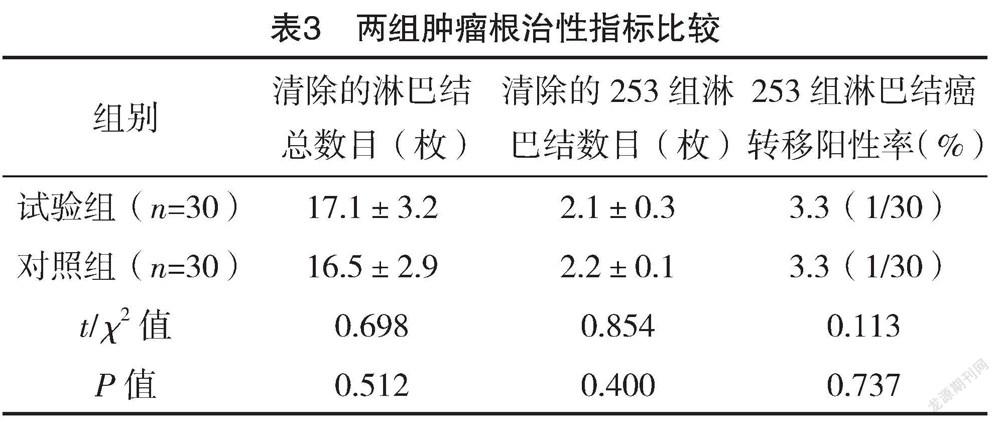
2.3 兩組腫瘤根治性指標(biāo)比較 兩組清除的淋巴結(jié)總數(shù)目、清除的253組淋巴結(jié)數(shù)目以及253組淋巴結(jié)癌轉(zhuǎn)移陽(yáng)性率比較,差異均無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05),見(jiàn)表3。
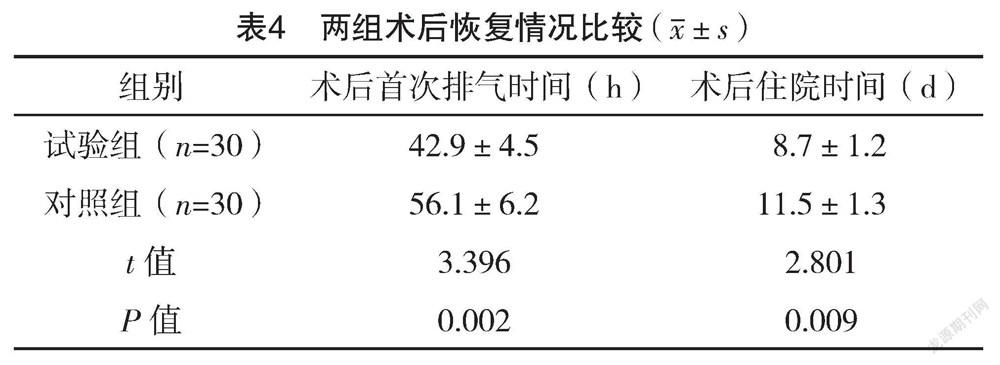
2.4 兩組術(shù)后恢復(fù)情況及并發(fā)癥發(fā)生情況比較 試驗(yàn)組術(shù)后首次排氣時(shí)間、術(shù)后住院時(shí)間均短于對(duì)照組,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05),見(jiàn)表4。兩組均未出現(xiàn)吻合口出血及切口感染,試驗(yàn)組無(wú)吻合口漏,對(duì)照組4例吻合口漏,3例為B級(jí)漏,1例為A級(jí)漏,經(jīng)保守治療后好轉(zhuǎn),兩組比較,差異有統(tǒng)計(jì)學(xué)意義(字2=4.286,P=0.038)。
3 討論
腹腔鏡直腸癌根治術(shù)具有手術(shù)視野清晰、損傷小、術(shù)后恢復(fù)快等優(yōu)點(diǎn),為淋巴結(jié)的清掃創(chuàng)造了更好的條件[6],目前已成為首選手術(shù)方式,然而關(guān)于腹腔鏡直腸癌根治術(shù)中是否保留LCA、保留LCA的臨床意義和療效等仍存在爭(zhēng)議,主要在于是否能夠徹底清掃淋巴結(jié)以及吻合口血供上。
淋巴結(jié)轉(zhuǎn)移是直腸癌最為常見(jiàn)且對(duì)預(yù)后具有重要影響的轉(zhuǎn)移途徑之一[7]。日本大腸癌規(guī)約將IMA根部淋巴結(jié)命名為第253組淋巴結(jié),頭側(cè)緣為IMA起始部,外側(cè)緣為腸系膜下靜脈內(nèi)側(cè),LCA為下側(cè)緣,內(nèi)側(cè)緣為IMA右側(cè),其轉(zhuǎn)移的發(fā)生率為0.3%~8.6%[8-9]。文獻(xiàn)[10-11]認(rèn)為清掃第253組淋巴結(jié)可以獲得更長(zhǎng)的生存期限,降低復(fù)發(fā)、轉(zhuǎn)移的風(fēng)險(xiǎn)。無(wú)253組淋巴結(jié)轉(zhuǎn)移的患者5年存活率為71.5%,然而存在253組淋巴結(jié)轉(zhuǎn)移5年存活率僅為37.5%,差異有統(tǒng)計(jì)學(xué)意義(P<0.05)[12]。因此,目前253組淋巴結(jié)需常規(guī)清掃。Kobayashi等[13]認(rèn)為高位結(jié)扎IMA步驟簡(jiǎn)單,容易掌握,對(duì)253組淋巴結(jié)的清掃比較徹底,保留LCA則增加了手術(shù)難度和手術(shù)時(shí)間。然而日本學(xué)者Sekimoto等[14]通過(guò)回顧分析比較,發(fā)現(xiàn)保留與不保留LCA在手術(shù)時(shí)間、淋巴結(jié)清掃總數(shù)、253組淋巴結(jié)清掃數(shù)量及其陽(yáng)性率方面比較,差異均無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05)。本研究結(jié)果顯示,兩組清除的淋巴結(jié)總數(shù)目、清除的253組淋巴結(jié)數(shù)目、術(shù)中出血量、手術(shù)時(shí)間比較,差異均無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05)。提示保留LCA與高位結(jié)扎IMA相比,清掃的淋巴結(jié)數(shù)量和腫瘤根治的標(biāo)準(zhǔn)相似,并未增加手術(shù)時(shí)間和出血量。本研究體會(huì)為:(1)細(xì)致解剖IMA及其分支;(2)進(jìn)入正確的Toldts間隙,避免損傷周?chē)K器,尤其注意保護(hù)髂腹下神經(jīng)和輸尿管等;(3)LCA與腸系膜下靜脈常常有一段伴行,因此在游離腸系膜下靜脈主干時(shí)注意避免損傷LCA。
腹腔鏡直腸癌根治性手術(shù)后吻合口漏是嚴(yán)重并發(fā)癥,可導(dǎo)致患者死亡,值得重視,文獻(xiàn)[15]報(bào)道發(fā)生率1%~20%,其危險(xiǎn)因素有患者糖尿病、年齡、性別、腫瘤距肛門(mén)距離、出血量、手術(shù)時(shí)間、新輔助放化療等,而吻合口血供和張力是最重要的因素[16-17]。Seike等[18]研究證明,高位結(jié)扎IMA可能顯著減少殘留結(jié)腸的血供。IMA高位離斷后,吻合口血液供應(yīng)來(lái)自邊緣血管弓,左結(jié)腸動(dòng)脈的升支與結(jié)腸中動(dòng)脈的左支在脾曲附近形成吻合支,此吻合支通常較細(xì)小,據(jù)統(tǒng)計(jì)有近5%的人缺如,對(duì)這類(lèi)患者保留LCA更加有意義[19-21]。本研究中試驗(yàn)組未出現(xiàn)吻合口漏,對(duì)照組有4例出現(xiàn)吻合口漏,兩組比較,差異有統(tǒng)計(jì)學(xué)意義(P<0.05);試驗(yàn)組術(shù)后首次排氣時(shí)間、術(shù)后住院時(shí)間均短于對(duì)照組,差異均有統(tǒng)計(jì)學(xué)意義(P<0.05)。表明術(shù)后腸道首次排氣時(shí)間更早,恢復(fù)更快,并發(fā)癥發(fā)生率更低,提示保留了LCA后可以確保腸管血供,避免游離脾曲,降低了吻合張力,減少吻合口漏發(fā)生。試驗(yàn)組操作過(guò)程雖略復(fù)雜,但不需要游離脾曲,并且不需要過(guò)多的切除腸管,因此總的手術(shù)時(shí)間并未延長(zhǎng)。本研究發(fā)現(xiàn)部分患者切斷IMA根部后,近端腸管明顯缺血,甚至變黑壞死,此時(shí)往往需切除更多的腸管,導(dǎo)致吻合口張力過(guò)大,需要進(jìn)一步游離結(jié)腸脾曲或改行預(yù)防性造口,這從另一角度說(shuō)明保留LCA可以改善腸管的血供,保留更多的正常腸管。對(duì)照組切除了更多的腸管,但并沒(méi)有增加淋巴結(jié)總數(shù),沒(méi)有增加陽(yáng)性率,因此患者在腫瘤根治方面并沒(méi)有明顯獲益。文獻(xiàn)[20]提示部分保留LCA的患者,因血供更好,可能導(dǎo)致吻合口出血,而本研究中所有患者無(wú)吻合口出血,本研究采用常規(guī)方法行吻合口縫合,減少術(shù)后出血風(fēng)險(xiǎn)。
綜上所述,與傳統(tǒng)高位結(jié)扎術(shù)式相比,腹腔鏡直腸癌根治術(shù)中保留LCA在手術(shù)安全性、淋巴結(jié)清掃等方面差異無(wú)統(tǒng)計(jì)學(xué)意義,可以促進(jìn)術(shù)后康復(fù),減少吻合口漏發(fā)生率,安全可行。
參考文獻(xiàn)
[1]姚宏偉,劉蔭華.基于循證醫(yī)學(xué)證據(jù)的腹腔鏡直腸癌手術(shù)療效評(píng)價(jià)[J].中華外科雜志,2017,55(1):28-31.
[2] LI X X,LI Q G.Significance of left colonic artery preservation in laparoscopic rectal cancer surgery[J].Chinese Journal of Gastrointestinal Surgery,2018,21(3):272-275.
[3]韓儒墨,姚寶福,馮國(guó)勛.保留左結(jié)腸動(dòng)脈的腹腔鏡直腸癌D3根治術(shù)對(duì)中晚期直腸癌患者的臨床效果分析[J/OL].中華普外科手術(shù)學(xué)雜志(電子版),2021,15(1):27-30.
[4]姜慧員,劉海義,江波,等.保留左結(jié)腸動(dòng)脈在腹腔鏡直腸癌前切除術(shù)中的臨床應(yīng)用和療效觀察[J/OL].中華結(jié)直腸疾病電子雜志,2021,10(1):70-75.
[5] LUO Y,YU M H,HUANG Y Z,et al.Lymphadenectomy Around Inferior Mesenteric Artery in Low-Tie vs High-Tie Laparoscopic Anterior Resection: Short- and Long-Term Outcome of a Cohort of 614 Rectal Cancers[J].Cancer Management and Research,2021,13:3963-3971.
[6]沈海玉,劉正,陳佳楠,等.血管三維重建技術(shù)在腹腔鏡保留左結(jié)腸動(dòng)脈的直腸癌低位前切除術(shù)的臨床應(yīng)用研究[J/OL].中華結(jié)直腸疾病電子雜志,2021,10(2):137-143.
[7] Watanabe T,Muro K,Ajioka Y,et al.Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer[J].Int J Clin Oncol,2018,23(1):1-34.
[8]李偉,國(guó)瑀辰,所劍.腹腔鏡下保留左結(jié)腸動(dòng)脈的直腸癌D3根治術(shù)的爭(zhēng)議與體會(huì)[J].中國(guó)普外基礎(chǔ)與臨床,2019,7(7):135-139.
[9] Girard E,Trilling B,Rabattu P Y,et al.Level of inferior mesenteric artery ligation in low rectal cancer surgery: high tie preferred over low tie[J].Tech Coloproctol,2019,23(3):267-271.
[10] RAO X,ZHANG J,LIU T,et al.Prognostic value of inferior mesenteric artery lymph node metastasis in cancer of the descending colon, sigmoid colon and rectum[J].Clolrectal Dis,2018,20(6):135-142.
[11] Ubukata M,Itabashi M,Kameoka S.Japanese D3 lymph node dissection in low rectal cancer with inferior mesenteric lymph node metastses[J].World J Surg,2014,38(10):2724-2729.
[12] Benson A B,Venook A P,Bekaii-Saab T,et al.Rectal Cancer,Version 2.2015[J].J Natl Compr Canc Netw,2015,13(6):719-728.
[13] Kobayashi M,Okamoto K,Namikawa T,et al.Laparoscopic lymph node dissection around the inferior mesenteric artery for cancer in the lower sigmoid colon and rectum: is D3 lymph node dissection with preservation of the left colic artery feasible?[J].Surg Endosc,2006,20(4):563-569.
[14] Sekimoto M,Takemasa I,Mizushima T,et al.Laparoscopic lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery[J].Surg Endosc,2011,25(3):861-866.
[15] Sakr A,Emile S H,Abdallah E,et al.Predictive Factors for Small Intestinal and Colonic Anastomotic Leak: a Multivariate Analysis[J].Indian J Surg,2017,79(6):555-562.
[16]徐誼,趙曉牧,孫武青,等.直腸癌低位前切除術(shù)后吻合口瘺發(fā)生相關(guān)因素分析[J].首都醫(yī)科大學(xué)學(xué)報(bào),2017,38(5):727-732.
[17] Fukada M,Matsuhashi N,Takahashi T,et al.Risk and early predictive factors of anastomotic leakage in laparoscopic low anterior resection for rectal cancer[J].World J Surg Oncol,2019,17(1):178.
[18] Seike K,Koda K,Saito N,et al.Laser doppler assessment of the influence of division at the root of the inferior mesenteric artery on anastomotic blood flow in rectosigmoid cancer surgery[J].Int J Colorectal Dis,2007,22(6):689-697.
[19]駱洋,陳建軍,秦駿,等.腹腔鏡直腸癌根治術(shù)中腸系膜下動(dòng)脈低位結(jié)扎對(duì)第3站淋巴結(jié)清掃的影響及第3站淋巴結(jié)轉(zhuǎn)移危險(xiǎn)因素分析[J].中華消化外科雜志,2018,17(2):154-160.
[20]臧潞,馬君俊,鄭民華.直腸癌根治術(shù)中保留左結(jié)腸動(dòng)脈對(duì)吻合口瘺及手術(shù)時(shí)間的影響[J].中華胃腸外科雜志,2016,19(4):386-387.
[21]孫躍明,唐俊偉.腹腔鏡直腸癌根治術(shù)保留左結(jié)腸動(dòng)脈關(guān)鍵技術(shù)與意義[J/OL].中華普外科手術(shù)學(xué)雜志(電子版),2019,13(1):13-15.
(收稿日期:2021-09-18)(本文編輯:姬思雨)

