Recurrence of sigmoid colon cancer–derived anal metastasis: A case report and review of literature
INTRODUCTION
The incidence of colorectal cancer is 38.7 per 100000 and 50%-60% of patients develop distant metastases with the liver being the most common site of involvement[1]. The most common seeding metastatic site of colorectal cancer is the anastomosis[2]. In contrast, metastasis at the anus is rare, with only 30 cases published in PubMed thus far. Due to the limited number of cases and insufficient information for anal metastasis of colorectal cancer, the diagnosis of such patients is difficult. In addition, there is currently no standard treatment and postoperative management strategy for anus metastasis of colorectal cancer. In most cases, patients receive surgical treatment and some are also treated with radiotherapy or chemotherapy. Patients who receive surgical treatment typically exhibit a good prognosis with a low recurrence rate. We reviewed and analyzed the relevant literature to provide more information to help clinicians better recognize and treat similar cases in the future.
CASE PRESENTATION
Chief complaints
In May 2020, an 80-year-old man presented with symptoms including anal swelling and pain.
History of present illness
Patient’s symptoms started a month ago with recurrent episodes of anal swelling and pain, as well as blood in the stool and diarrhea.
The patient went to hospital for colonoscopy due to repeated blood in stool in January 2010. A mass in sigmoid was found and pathology showed moderately differentiated adenocarcinoma. Subsequently, he underwent an open radical resection of the sigmoid colon in January 2010. Postoperative pathological examination showed moderately differentiated adenocarcinoma, pT3N1M0, with invasion to the serosal layer; the margin was free and 1 of 29 Lymph nodes was positive. In December 2010, he complained of anal swelling and pain and subsequently underwent anal fistula resection. Postoperative pathology revealed moderately differentiated adenocarcinoma and the margin was free. In December 2010, the patient began 6 cycles of chemotherapy with the FOLFIRI regimen and one course of local anal radiotherapy (45 Gy in 25 fractions). In September 2019, he was admitted to the Department of Hematology for four rounds of Azacytidine chemotherapy for myelodysplastic syndrome (MDS).
為了提高空氣動力學課程的教學質量,并鍛煉學生的動手能力,克服大型伯努利原理驗證實驗裝置體積大、耗能多,實測數據誤差大等缺點,組織學生研制了一種小型的基于音頻的伯努利方程驗證實驗裝置。
History of past illness
在時域測量過程中,采用一定的時域窗口進行采樣,通常采用阿倫方差來表征時域的頻率穩定度。阿倫方差的定義式為:
為了不露馬腳,鄧強等人也著實費了一番心思。2012年3月2日,城投公司與市建公司簽訂合同,將肇慶市安居華苑項目發包給市建公司。同年3月23日,市建公司又將項目內部承包給公司員工梁某金。而在此之前,梁某金已和林某強簽訂合作協議及委托書,將項目委托給林某強個人承包施工。
Personal and family history
This case highlights that there is a risk of recurrence of anal metastasis of colorectal cancer even after 10 years of follow-up. We also reviewed the literature and discuss potential mechanisms for anal metastasis of colorectal cancer, thus providing some suggestions for treatment of these cases.
Physical examination
Our physical examination found an approximate 3 cm × 3 cm perianal ring-shaped mass with obvious tenderness.
Laboratory examinations
Compared with the previously reported cases, our cases show some unique characteristics and findings. The patient received radiotherapy and chemotherapy after resection of local anal metastatic lesions in 2010, but recurrence of local anal tumor still occurred 10 years later. However, this patient needed chemotherapy for MDS with ring sideroblasts and with multilineage dysplasia (RS-MLD), so only a perianal mass biopsy was performed to confirm the diagnosis. Although APR surgery was planned after the chemotherapy, the patient still required management for RS-MLD and died 5 mo later.
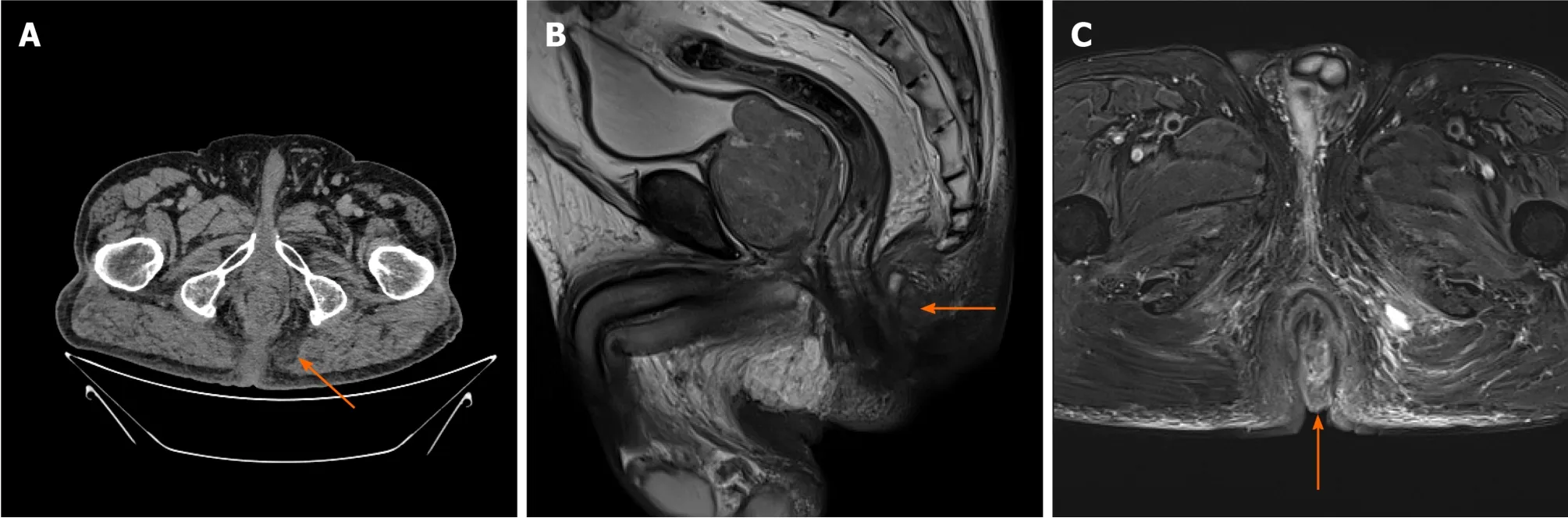
Imaging examinations
Colonoscopy did not detect any mass or abnormality. Computed tomography found low-density shadows on the posterior edge of the anal canal. Magnetic resonance imaging further confirmed that the 22.8 mm × 24.2 mm lesion went through the external sphincter. The internal fistula was located at 6 o’clock on the posterior edge of the anal canal; the external fistula was at the left side of the buttocks; and the subcutaneous soft tissue signal of the buttocks was increased (Figure 1). Biopsy test of the anal mass was performed by resecting the most obvious swollen part at the lithotomy position. Postoperative pathology of this soft and poorly structured tissue showed moderately differentiated adenocarcinoma with large amounts of necrotic tissue that was positive for cytokeratin 20 (CK20) and negative for cytokeratin 7 (CK7)(Figure 2).
FINAL DIAGNOSIS
Based on pathology as well as the patient’s history, the final diagnosis was metastatic anal cancer derived from sigmoid colon cancer.
TREATMENT
OUTCOME AND FOLLOW-UP
We planned to perform abdominoperineal resection (APR) after chemotherapy for MDS in another hospital. However, the patient died due to MDS in November 2020.
DISCUSSION
The most common distant metastasis site of colorectal cancer is the liver[3]. Regarding implantation metastases, the most common ones are observed at anastomoses and biopsy sites, and some studies have reported metastases at fistulas and hemorrhoids[2,4-9]. Metastasis of sigmoid colon cancer to the anus is very rare[10], and so far, the underlying mechanism remains unknown. One possible explanation for these metastases is that improper operation during surgery may cause tumor cells to fall off and relocate, but in general, tumor cells do not easily implant to intact mucosa.However, the intestinal mucosa could possibly be damaged when surgical instruments or fingers are used to expand the anus during surgery. In this case, damaged intestinal mucosa might become an adhesion target for tumor cells, which would then colonize and begin to proliferate[5,6,8,11]. This phenomenon has been observed in mouse models. For example, Hubens[12] observed that mice with damaged intestinal mucosal develop gut tumors after colorectal cancer cells perfuse into the colon, while no mice with intact intestinal mucosa showed tumor growth. Another possible explanation is that tumor cells were already implanted into the existing fistula before resection of the primary tumor. Occasionally, clinical symptoms appear when the tumor grows to a sufficient size[13]. In addition, one study reported the same DNA aneuploid cell line in sigmoid colon tumors and perianal tumors[14]. These findings supported a potential metastasis mechanism of tumor cells migrating from the colon to anus. More cases and studies are warranted to better elucidate the underlying mechanisms.
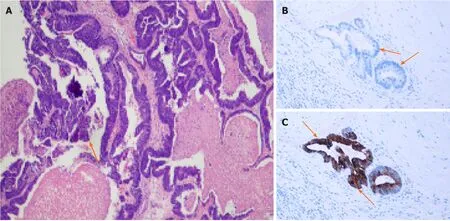
Diagnostic criteria have not been established in metastatic anal cancer. First,colorectal cancer cases with first symptoms as anal fistula and perianal abscess should be excluded[4]. Additionally, diagnosis of metastatic anal cancer should include primary tumors in the colon with five exclusion criteria for primary anal fistula cancer:(1) More than 10 years of history of anal fistula; (2) Induration and severe pain at the anal fistula; (3) Mucus secretion; (4) Internal opening in the anus and anal recess; and(5) No tumor on the cranial side of the anal fistula[15]. More importantly, immunohistochemical staining of CK7 and CK20 biomarkers is usually used to confirm the presence of a metastatic tumor. Anal tissue shows strong positive expression only for CK7, while colorectal tumor tissue shows positive CK20 expression[16,17]. Immunohistochemical analyses of the tumor in the current case were CK20 positive and CK7 negative, consistent with our diagnosis as metastatic anal cancer.
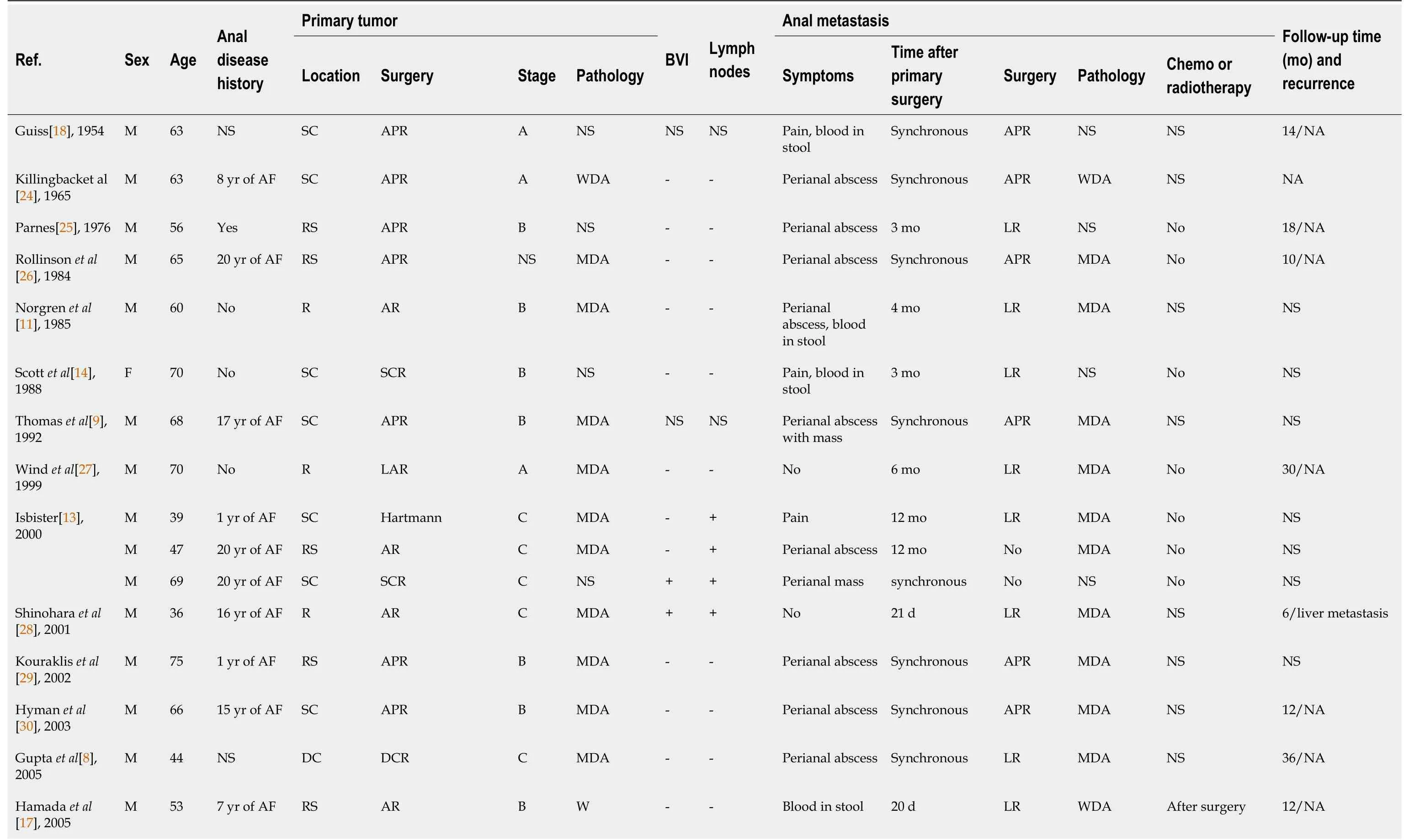
We further reviewed previous publications of these cases. Guiss[18] published the first case report of sigmoid colon cancer implanted anal fistula in 1954. We retrieved 25 papers from PubMed describing a total of 30 cases of colorectal cancer metastasis to the anus (Table 1). Among the 30 patients, there was only one female, and the mean patient age was 60.2 yr. Seventeen patients (56.7%) had a history of anal disease. Most patients complained of anal abscess and induration as first symptoms. All primary tumors were located in or below the descending colon; 13 tumors (43.3%) were located in the colon, 12 tumors (40%) were at the junction of the rectum and sigmoid colon,and the remaining 5 tumors (16.7%) were in the rectum. This location information may support the idea that seeding metastasis, instead of hematogenous or lymphatic was more likely the cause of anal metastasis formation. All 30 patients underwent radicalprimary tumor resection; 16 cases (53.3%) had synchronous metastases and the rest 14 cases (46.7%) had metachronous metastases at approximately 8.5 mo post-surgery.Due to the limited number of cases, there is currently no standard treatment method for colorectal cancer–derived anus metastasis. Surgery is still the most common treatment method. Among the 30 cases, 13 patients (43.3%) received APR surgery, 15 patients (50%) underwent additional local lesion resection after radical colorectal surgery, and 3 patients (10%) did not undergo surgery because of extensive tumor metastasis or disapproval of the surgical plan. Overall, postoperative pathology was mostly moderately or well-differentiated adenocarcinoma. Notably, only 11 patients received radiotherapy and chemotherapy during the perioperative period. However,the prognosis of most patients was good. The average follow-up time for patients was 29.9 mo. Only one patient died 10 mo after surgery from extensive peritoneal metastasis[19].
Blood count shows lymphocyte count 1.03 × 10/L, red blood cell count 3.52 × 10/L,hemoglobin 114 g/L and albumin 33.2 g/L. Blood tests for cancer-associated markers revealed the carcinoembryonic antigen (CEA) of 5.95 ng/mL and carbohydrate antigen 199 (CA199) of 20.59 U/mL. Fecal occult blood test was positive.
The main surgical treatment options are APR and local resection. Although APR is more effective in reducing the risk of residual tumor cells, the life quality of patients is relatively poor. Therefore, we suggest that local resection should be considered first to ensure that patients have a better quality of life after surgery when the anus tumor does not aggressively grow. In addition, Ikeda[5] indicated that tumors should be treated first when the patient exhibits other anal diseases. Otherwise, it is possible that the tumor cells may easily implant on the anal wound and cause anal recurrence.Regarding perioperative radiotherapy and chemotherapy, a retrospective study of metastatic anal cancer patients from 1950 to 2011 found that the combination of preoperative or postoperative radiotherapy, chemotherapy and radical surgical resection provided patients with better survival compared with patients receiving surgeries only[20]. At present, there is no standard postoperative follow-up management guideline, so we should extend the postoperative follow-up time for such patients to detect the disease and provide treatment in a timely manner.
The current patient reported no anal disease before the first radical surgery.Although without immune-histological result, histological features of this anal mass were moderately differentiated gland cancer, similar to primary tumor in sigmoid colon. Considering the anatomical structure of the colon and anus and combined with the patient’s medical history, we therefore believe that the lesion was derived from sigmoid colon tumor cells. Since any shed tumor cells would not be implanted on the intact intestinal mucosa, as discussed above, we assume that this may be from stapler use that damaged the anal mucosa during the operation. The patient showed a relapse at the anus, and the colonoscopy showed no tumor in the colon. Moreover, immunohistological results showed the tumor was derived from colon, so it was possible that a small amount of tumor cells had remained in the anus. Moreover, chemotherapy for MDS for 4 mo potentially impaired the patient’s immune system, causing any remaining tumor cells to proliferate.
In the fault mode 2, two generators and auxiliary electricity device all fails at 0.8 s. After 0.1 s delay, the battery supplies for the DC motor connected to the DC(28 V) port on the right.
隨著社會經濟不斷發展和對人才的較高要求,就業指導課也要隨之變化、隨之發展,不斷增加新的內容。獨立學院應根據學生個性特征和社會經濟發展的需要,有目的、有計劃、有步驟地對學生未來的職業定位及在校期間的職業準備、職業能力培養等施加影響[4]。
Norgren[11] and Tranchart[21] also reported cases of recurrence of local scars in the anus caused by the use of staplers and retractors during operation.Therefore, surgeons should be aware of the importance of protecting the mucosa during surgical procedures, for example during staple use and retraction. Another study reported the presence of tumor cells in washing solution after rectal washing during surgery. Therefore, sterile water or 5% povidone-iodine and other cytotoxic solutions may be useful to wash the surgical area to reduce the numbers of any remaining tumor cells and prevent local recurrence[22,23]. A close follow-up around the anus after surgery is also recommended.
美國容量市場和備用服務市場均運行多年,在供需平衡的情況下,容量市場的價格等于發電成本減去在能量市場和輔助服務市場中已補償的成本。目前多數國家的容量市場與美國的設計理念一致,即系統裝機容量將平衡在基準峰荷機組成本剛好回收的點上。
CONCLUSION
Metastasis of colorectal cancer to the anus is very rare. The clinical symptoms are similar to benign anal diseases like perianal abscesses and anal fistula, which makes the diagnosis of metastasis of colorectal cancer to the anus more difficult. Currently,pathological examination and staining of CK7 and CK20 markers can contribute to diagnosis of anal metastases. In addition, surgeons should pay attention to protecting the normal mucosa during operation to reduce the possibility of implant metastasis caused by iatrogenic injury. During surgery, surgical area irrigation with cytotoxic solution is also recommended to reduce the number of remaining tumor cells. For patients with anal metastasis, the follow-up time after surgery should be extended.Accumulating more clinical data is necessary to establish treatment and postoperative management standards for colorectal cancer–derived anal metastasis.
 World Journal of Clinical Cases2022年3期
World Journal of Clinical Cases2022年3期
- World Journal of Clinical Cases的其它文章
- Mycoplasma hominis meningitis after operative neurosurgery: A case report and review of literature
- New method to remove tibial intramedullary nail through original suprapatellar incision: A case report
- Metastasis to the thyroid gland from primary breast cancer presenting as diffuse goiter: A case report and review of literature
- Gastric submucosal lesion caused by an embedded fish bone: A case report
- Epibulbar osseous choristoma: Two case reports
- Bullectomy used to treat a patient with pulmonary vesicles related to COVID-19: A case report
