胸腰交界椎旁巨大啞鈴形腫瘤的手術策略
涂兵 陳鈞麟 練沛榮 夏虹 易紅蕾
【摘要】目的明確胸腰交界椎旁巨大啞鈴形腫瘤定義,建立其臨床分型,并根據術前臨床分型選擇胸腰交界椎旁巨大啞鈴形腫瘤手術治療策略。方法回顧性分析2018年1月—2023年1月南部戰區總醫院收治的11例胸腰交界椎旁巨大啞鈴形腫瘤患者。根據腫瘤與胸腰椎相對解剖位置的關系,將橫向最遠端距脊柱后正中線距離≥6 cm的腫瘤定義為胸腰交界椎旁巨大啞鈴形腫瘤,并制定新的臨床分型,即椎旁型(腫瘤未超過椎體前緣)和椎前型(腫瘤超過椎體前緣)。對椎旁型采用后路腫瘤切除術,對椎前型行后路聯合前路腫瘤切除術。術后1周、3個月、6個月、12個月及每年行X線、CT及MRI檢查,評價腫瘤切除情況、是否復發及脊柱穩定性、內固定情況;定期隨訪并評估術后疼痛改善情況。結果椎旁型8例,5例行后路腫瘤切除術+內固定術,3例行后路腫瘤切除術。椎前型3例,2例行后路+前路腫瘤切除術,1例行后路+前路腫瘤切除術+內固定術。術前與術后JOA及VAS評分差異有統計學意義(分別為P=0.03;P<0.001)。術后組織病理學確診為神經鞘瘤9例,神經纖維瘤2例。11例均獲隨訪。隨訪時間 6個月~2年。所有患者術后復查均未見腫瘤復發,神經癥狀均明顯改善,胸腰背部無酸痛感,內固定無松動、斷裂。結論腫瘤橫向最遠端距脊柱后正中線距離≥6 cm為胸腰交界椎旁巨大啞鈴形腫瘤,可分為椎旁型和椎前型。椎旁型采用單純后路腫瘤切除術即可實現滿意切除;椎前型宜采用后路聯合前路腫瘤切除術方能實現滿意切除。
【關鍵詞】胸腰交界椎旁巨大啞鈴形腫瘤;臨床分型;手術策略
【中圖分類號】R739.41;R651【文獻標志碼】A【文章編號】16727770(2024)02015105
Surgical treatment strategy of giant dumbbell paraspinal tumors at thoracolumbar junction TU Bing, CHEN Junlin, LIAN Peirong, et al. Department of Orthopedics, General Hospital of the Southern Theater Command of the PLA of China, Guangzhou 510010, China
Corresponding author: YI Honglei
Abstract: ObjectiveTo clarify the definition of giant paraspinal dumbbell tumor at thoracolumbar junction and establish the clinical classification. The surgical treatment strategy of giant paraspinal dumbbell tumor at thoracolumbar junction was selected according to the preoperative clinical classification. Methods11 patients with giant paraspinal dumbbell tumors at the thoracolumbar junction admitted to General Hospital of the Southern Theater Command of China from January 2018 to January 2023 were analyzed retrospectively. According to the relationship between the tumor and the relative anatomical position of the thoracolumbar vertebrae, the distance between the transverse farthest end of the tumor and the posterior midline of the spine ≥6 cm was defined as a huge dumbbell tumor at the thoracolumbar junction, and a new clinical classification was established, paraspinal type (tumor not exceeding the anterior edge of vertebral body) and prevertebral type (tumor exceeding anterior edge of vertebral body). Posterior tumor resection was performed for paraspinal type and posterior combined with anterior tumor resection for prevertebral type. Xray, CT and MRI examinations were performed at 1 week, 3 months, 6 months, 12 months and every year to evaluate tumor resection, recurrence, spinal stability and internal fixation, spinal cord nerve function was evaluated, and postoperative pain improvement was evaluated. ResultsIn8 cases of paraspinal type, posterior tumor resection with fixation was performed in 5, and simple posterior tumor resection was performed in 3. In 3 cases of prevertebral type, posterior combined with anterior resection was performed in 2, and posterior combined with anterior resection with fixation was performed in 1. There was a statistically significant difference in JOA and VAS scores between preoperative and postoperative(P=0.03,P<0.001). Postoperative histopathology confirmed neurilemmoma in 9 and neurofibroma in 2. All 11 cases were followed up, and the followup period ranged from 6 months to 5 years. No tumor recurrence was found in all patients, the neurological symptoms were significantly improved, there was no pain in the chest, waist and back, and there was no loosening or fracture of the internal fixation. ConclusionsThe distance between the furthest transverse end of the tumor and the posterior midline of the spine ≥ 6cm is a huge dumbbell tumor at the thoracolumbar junction, which can be divided into paraspinal type and prevertebral type. Satisfactory resection can be achieved by simple posterior tumor resection in paraspinal type, and satisfactory resection can be achieved by posterior combined with anterior tumor resection in prevertebral type.
Key words: giant paraspinal dumbbell tumor at thoracolumbar junction; clinical classification; surgical treatment strategy
椎管內外啞鈴形神經鞘瘤多位于硬膜外,起源于脊神經根,多見于后根。腫瘤生長緩慢,可由硬膜外順神經根長至椎管外或硬膜內,也可由椎管外長至椎管內[1]。椎管內外溝通性腫瘤通過椎間孔累及椎管內外,由于腫瘤形態多呈啞鈴形,故又稱為“啞鈴形”腫瘤。病理類型主要為神經鞘瘤、神經纖維瘤和惡性神經鞘瘤[2]。胸腰交界椎旁啞鈴形腫瘤因在病程初期無明顯的臨床癥狀患者不易察覺,胸腰交界椎旁啞鈴形腫瘤盡管生長緩慢,但仍容易生長成巨大的胸腰交界椎旁啞鈴形腫瘤。胸腰交界椎旁巨大啞鈴形腫瘤生長位置特殊,毗鄰肋骨及腎臟等腹部臟器,并且涉及巨大的椎管外腫瘤成分,手術暴露與手術切除均存在較大的困難[36]。本研究回顧性分析南部戰區總醫院2018年1月—2023年1月收治的11例胸腰交界椎旁巨大啞鈴形腫瘤患者,結合手術實踐經驗,明確胸腰交界椎旁巨大啞鈴形腫瘤定義,將腫瘤橫向最遠端距脊柱后正中線距離≥6 cm定義為胸腰交界椎旁巨大啞鈴形腫瘤,提出了新的胸腰交界椎旁巨大啞鈴形腫瘤臨床分型及其對應的手術方案,在一期腫瘤全切與減少患者創傷的原則上,根據術前臨床分型選擇胸腰交界椎旁巨大啞鈴形腫瘤最佳手術治療策略。
1資料與方法
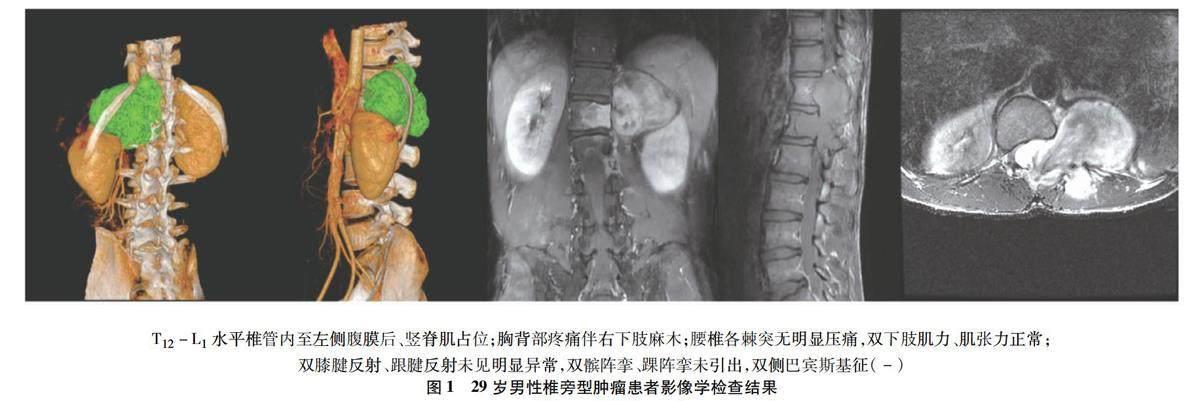
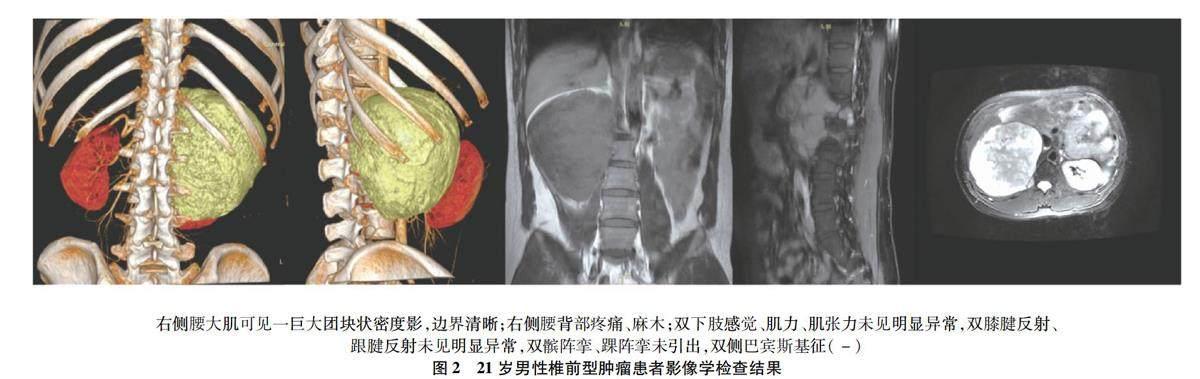
1.1一般資料共納入胸腰交界椎旁巨大啞鈴形腫瘤患者11例,其男7 例,女4例,年齡 21~61歲,平均年齡(41±13.68)歲;臨床表現為胸背部疼痛11例,下肢麻木8例,下肢乏力4例,步態不穩5例,11例患者均未出現大小便障礙。排除其他腫瘤、脊柱畸形、脊柱骨折、脊柱感染以及結核、類風濕性關節炎等病理性病變。所有患者術前均進行全脊柱正側位、胸腰椎正側位X線、胸腰椎計算機斷層掃描(computer tomography,CT)三維重建以及胸腰椎核磁共振成像(magnetic resonance imaging,MRI)平掃+增強檢查,影像學見硬膜囊及神經根受壓,腫瘤橫向最遠端距脊柱后正中線距離6.5~8.3 cm,腫瘤椎管內部分橫向大小0.56~1.36 cm、腫瘤椎管內橫向占比7.3%~16.8%。術前MRI示,全部病例均存在胸腰交界椎旁巨大啞鈴形腫瘤。本研究通過南部戰區總醫院醫學倫理委員會批準(審批號:NBZQZYY2024037),所有患者均知情同意并簽署知情同意書。
1.2定義、臨床分型及其手術策略根據術前胸椎MRI檢查,在PACS影像系統上對腫瘤進行測量。將腫瘤橫向最遠端距脊柱后正中線距離≥6 cm定義為胸腰交界椎旁巨大啞鈴形腫瘤,并將腫瘤腹側是否超過椎體前緣作為臨界點,胸腰交界椎旁巨大啞鈴形腫瘤未超過椎體前緣為椎旁型,采用后路正中入路腫瘤切除術;胸腰交界椎旁巨大啞鈴形腫瘤超過椎體前緣為椎前型,采用后路旁正中入路聯合前路肋緣入路腫瘤切除術。
1.3手術方法
1.3.1椎旁型術前檢查見圖1。采用后路正中入路腫瘤切除術。患者取俯臥位,常規消毒、鋪無菌巾;C臂機定位腫瘤節段,沿棘突后正中切口依次切開皮膚、皮下、筋膜,于棘突左右兩側行骨膜下鈍性分離推籌肌內至橫突根部;超聲骨刀沿椎體關節突內側緣切除相應椎板,分離黃韌帶,顯露硬膜囊,探查腫物。絲線縫扎懸吊椎管內腫物后神經剝離子分離,分離腫物表面肌肉,取出椎管內外全部腫物。
1.3.2椎前型術前檢查見圖2。采用后路旁正中入路聯合前路肋緣入路腫瘤切除術。患者取俯臥位,常規消毒、鋪無菌巾。C臂機定位腫瘤節段手術切口,沿棘突后正中切椎旁2 cm縱行切口依次切開皮膚、皮下、筋膜,行肌間隙入路鈍性分離椎旁肌橫突,超聲骨刀沿椎體關節突內側緣切除相應椎板,分離黃韌帶,顯露硬膜囊,探查腫物,神經剝離子游離腫物。改變患者體位,取仰臥位,常規消毒、鋪無菌巾。行肋緣下切口逐層進腹,探查腹膜后巨大腫物,沿腫物包膜與側腹膜、腰大肌肉、腎周脂肪囊間隙,使用電刀及超聲刀逐步游離,取出腹膜后全部腫物。
1.4療效評估指標記錄手術時間及術中出血量,術后3 d行胸腰椎正側位X線檢查,評估內固定及脊柱情況;行胸腰椎CT檢查評估內固定及脊柱情況;行胸腰椎MRI平掃+增強評估腫瘤切除情況及脊髓壓迫解除情況。術后1周、3個月、6個月、12個月及每年進行隨訪,行體格檢查、臨床評價及X線、CT及MRI檢查,評價腫瘤切除情況、是否復發及脊柱穩定性、內固定情況。采用日本骨科協會(Japanese orthopedic association,JOA)評分評估脊髓神經功能,并計算JOA評分改善率,JOA評分值越高脊髓神經功能越好,反之脊髓神經功能越差;采用疼痛視覺模擬評分(visual analogu scale,VAS)評估患者手術前后胸背部疼痛程度及改善情況。VAS評分范圍為0~10分。
1.5統計學分析所得數據均導入SPSS 26.0統計學軟件進行統計學分析,統計分析所得數據的均值與標準差,手術前后JOA評分、VAS評分比較采用秩和檢驗,以P<0.05認為兩變量相關性顯著。
2結果
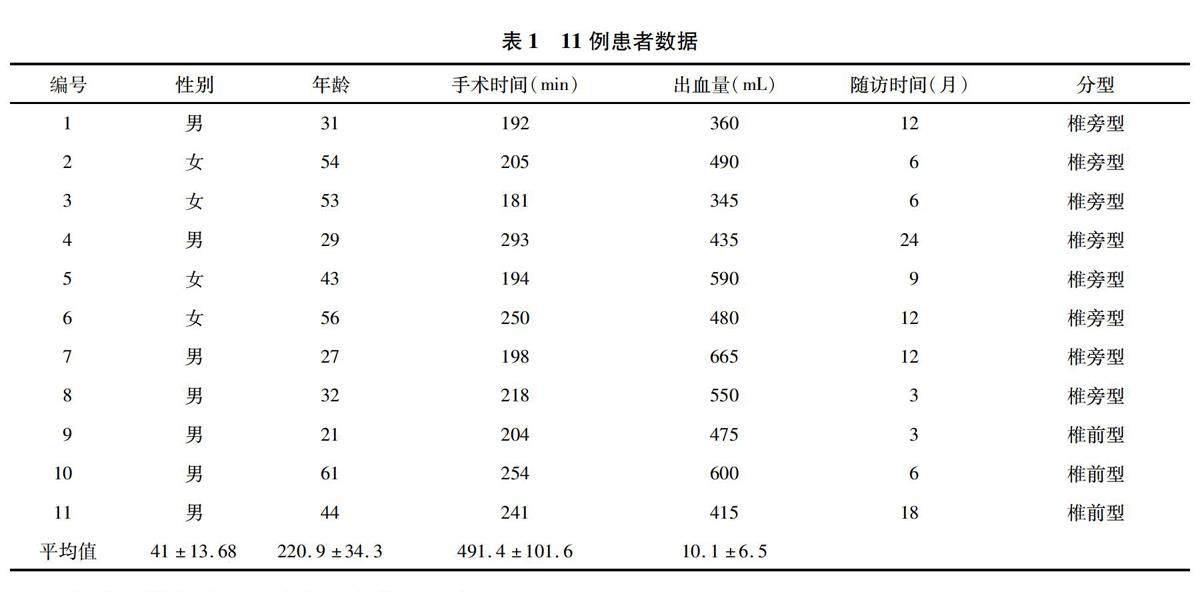
納入的11例患者,胸腰椎交界腫瘤橫向最遠端距脊柱后正中線距離均≥6 cm,均為胸腰交界椎旁巨大啞鈴形腫瘤,8例胸腰交界椎旁巨大啞鈴形腫瘤未超過椎體前緣,為椎旁型;3例胸腰交界椎旁巨大啞鈴形腫瘤超過椎體前緣,為椎前型。11例患者手術均成功施行,術中見腫瘤與脊髓神經根粘連,硬膜囊受壓,椎管外腫瘤較大,有完整包膜,質地較硬,跟周圍組織分界清楚。腫瘤完全切除,手術時間(220.9±34.3)min,術中出血量(491.4±101.6)mL,術中無脊髓及動脈損傷,術后無相關并發癥發生。見表1。
術后X線片及CT示內固定位置良好,MRI示腫瘤切除理想,脊髓壓迫解除。術后所有患者神經功能障礙癥狀均有顯著改善。術后病理檢查見腫瘤的最長徑6.3~11.2cm,平均(9.5±4.4)cm,術后組織病理學確診為神經鞘瘤9例,神經纖維瘤2例。末次隨訪JOA評分為(14.7±2.0)分,與術前相比較,差異有統計學意義(P=0.005);末次隨訪VAS為(0.27±0.5)分,與術前相比較,差異有統計學意義(P<0.001)。所有患者均獲得隨訪,隨訪時間為3~24個月,平均(10.1±6.5)個月,隨訪期間X線、CT示內固定無松動或斷裂,脊柱序列良好,無腫瘤復發。見表2。
3討論
胸腰交界椎旁巨大啞鈴形腫瘤生長緩慢、腫瘤通過椎間孔累及椎管內外,胸腰交界椎旁啞鈴形腫瘤因在病程初期無明顯的臨床癥狀患者不易察覺,盡管胸腰交界椎旁啞鈴形腫瘤生長緩慢,但仍容易生長成巨大的胸腰交界椎旁啞鈴形腫瘤。胸腰交界椎旁巨大啞鈴形腫瘤生長位置特殊,毗鄰肋骨及腎臟等腹部臟器,復雜的解剖結構及巨大的椎管外腫瘤成分,給手術帶來了巨大的挑戰,手術暴露與手術切除均存在較大的困難。腫瘤分型與手術方式的選擇密切相關,手術入路的選擇是胸腰交界椎旁巨大啞鈴形腫瘤手術治療的關鍵。
現有文獻報道中,先后提出了Eden分型(Ⅰ型:硬膜內和硬膜外;Ⅱ型:硬膜內、硬膜外和椎旁;Ⅲ型:硬膜內和椎旁;Ⅳ型:椎板和椎旁)、Toyama/Asazuma分型(Ⅰ型,椎管內硬膜內外啞鈴形腫瘤;Ⅱ型,腫瘤位于硬膜外,并累及椎間孔;Ⅲ型,腫瘤累及硬膜內,沿椎間孔生長;Ⅳ型,腫瘤侵犯前方椎體;Ⅴ型,腫瘤侵犯椎板等后方結構;Ⅵ型,腫瘤對前后方結構均有侵犯,并穿過神經孔,至椎旁)等脊柱啞鈴型腫瘤的分型[78],以及頸椎啞鈴型腫瘤分型[914],上述啞鈴型腫瘤分型均是在影像學軸位方向上對腫瘤進行分型。而當胸腰交界椎旁巨大啞鈴形腫瘤軸向生長受周圍組織限制時,便會以縱向生長為主,因此上述啞鈴型腫瘤分型對于胸腰交界椎旁巨大啞鈴形腫瘤來說并不適用。
對于大多數體積較小的胸腰椎交界腫瘤來說,通過單純后路正中入路基本就可以實現腫瘤的全部切除,真正有挑戰性的是巨大的啞鈴形腫瘤,國內外學者提出了多種解決這一具有挑戰性的方法,包括單純后路入路、后路+側路入路和后路+前路入路,但仍無研究對胸腰交界椎旁巨大啞鈴形腫瘤做出定義,臨床上對手術入路的選擇也取決于手術醫生的主觀經驗,術中如果改變術式,不僅增加了手術時間,還會給患者帶來不必要的創傷[1520]。術前識別胸腰椎巨大交界腫瘤及其分型對于手術計劃至關重要,為此本研究界定了胸腰交界椎旁巨大啞鈴形腫瘤為腫瘤橫向最遠端距脊柱后正中線距離≥6 cm,并將腫瘤腹側是否超過椎體前緣作為臨界點,胸腰交界椎旁巨大啞鈴形腫瘤未超過椎體前緣為椎旁型,采用后路正中入路腫瘤切除術;胸腰交界椎旁巨大啞鈴形腫瘤超過椎體前緣為椎前型,采用后路旁正中入路聯合前路肋緣入路腫瘤切除術。Eden及Toyama/Asazuma各類分型均可分為椎前型和椎旁型,此分型根據胸腰交界椎旁巨大啞鈴形腫瘤的生長特點,以影像學矢狀位為分型基礎,解決了現有啞鈴型腫瘤分型不適用于胸腰交界椎旁巨大啞鈴形腫瘤的缺點,為胸腰交界椎旁巨大啞鈴形腫瘤分型提供了新的思路。
本研究中,根據分型標準及對應的手術選擇,8例為椎旁型,3例為椎前型。采用后正中入路應先用神經剝離子探查腫瘤所涉及的神經,在椎間孔處離斷腫瘤,先處理腫瘤在椎管內的部分。采用后路旁正中入路聯合前路肋緣入路時先游離腫瘤在椎管外的部分,減少巨大腫瘤在術中對神經的牽扯,再沿著腫瘤邊緣逐漸剝離至椎管內,再切除椎管內腫瘤。胸腔、腹腔內腫瘤常與胸膜、腹膜粘連,應避免術中胸膜、腹膜損傷引起氣胸、氣腹。
所有患者術后均得到了滿意的臨床療效,一期手術均實現腫瘤完全切除,后期隨訪均未見腫瘤復發。以上臨床結果提示,此分型及手術選擇的可靠性,在保證腫瘤完全切除的同時,避免術中不必要的手術操作,解決了手術入路選擇的難題,為胸腰交界椎旁巨大啞鈴形腫瘤手術策略的選擇提供了指導。
利益沖突:所有作者均聲明不存在利益沖突。
[參 考 ?文 ?獻]
[1]Celli P,Trillò G,Ferrante L.Spinal extradural schwannoma[J].J Neurosurg Spine,2005,2(4):447456.
[2]Hilton DA,Hanemann CO.Schwannomas and their pathogenesis[J].Brain Pathol,2014,24(3):205220.
[3]Lee MT,Panbehchi S,Sinha P,et al.Giant spinal nerve sheath tumoursSurgical challenges:case series and literature review[J].Br J Neurosurg,2019,33(5):541549.
[4]Kalsi P,Zaidman N,Jain A,et al.Surgical management of giant thoracic paraspinal schwannomas[J].World Neurosurg,2021,149:e1155e1165.
[5]林鋒,何明方,鐘冬勝,等.椎管內外啞鈴狀神經鞘瘤的臨床特點及治療方式探討[J].中國醫學創新,2019,16(13):140147.
[6]Mastoraki A,Toska F,Tsiverdis I,et al.Retroperitoneal schwannomas:dilemmas in diagnostic approach and therapeutic management[J].J Gastrointest Cancer,2013,44(4):371374.
[7]Eden K.The dumbbell tumours of the spine[J].Br J Surg,2005,28(112):549570.
[8]Asazuma T,Toyama Y,Maruiwa H,et al.Surgical strategy for cervical dumbbell tumors based on a threedimensional classification[J].Spine(Phila Pa 1976),2004,29(1):E10E14.
[9]陳華江,肖建如,楊興海,等.頸椎啞鈴形腫瘤MRI分型探討[J].脊柱外科雜志,2006,4(4):208211.
[10]陳海鋒,李丹,王躍龍,等.頸椎啞鈴型腫瘤的臨床分型及手術入路的選擇[J].中華醫學雜志,2014,94(19):14441447.
[11]Goel A,Muzumdar D,Nadkarni T,et al.Retrospective analysis of peripheral nerve sheath tumors of the second cervical nerve root in 60 surgically treated patients[J].J Neurosurg Spine,2008,8(2):129134.
[12]Jiang L,Lv Y,Liu XG,et al.Results of surgical treatment of cervical dumbbell tumors:surgical approach and development of an anatomic classification system[J].Spine (Phila Pa 1976),2009,34(12):13071314.
[13]肖建如,楊興海,陳華江,等.頸椎管啞鈴形腫瘤的外科分期及手術策略[J].中華骨科雜志,2006(12):798802.
[14]Okubo T,Nagoshi N,Tsuji O,et al.Resection of cervical dumbbellshaped schwannoma using posterior unilateral approach:impact on postoperative cervical function and clinical outcomes[J].Global Spine J,2023:21925682231178205.
[15]Rong HT,Fan YS,Li SP,et al.Management of dumbbell and paraspinal tumors of the thoracic spine using a singlestage posterolateral approach:case series[J].Orthop Surg,2018,10(4):343349.
[16]Kurland DB,Lau D,Dalle Ore CL,et al.Combined retropleural thoracotomy and posterior spinal approach for thoracic dumbbell Schwannoma:Case series and review of the literature[J].J Clin Neurosci,2022,106:173179.
[17]李洋,鄒福建,鄧雷,等.頸椎管內外溝通性腫瘤一期全切的手術治療策略[J].臨床神經外科雜志,2023,20(1):2835.
[18]Takeyama M,Koshino T,Nakazawa A,et al.Giant intrasacral cellular schwannoma treated with high sacral amputation[J].Spine (Phila Pa 1976),2001,26(10):E216E219.
[19]Ngerageza JG,Ito K,Aoyama T,et al.Posterior laminoplastic laminotomy combined with a paraspinal transmuscular approach for removing a lumbar dumbbellshaped schwannoma:a technical note[J].Neurol Med Chir (Tokyo),2015,55(9):756760.
[20]施建黨,趙晨,丁惠強,等.前后聯合入路切除胸腰段椎管巨大啞鈴形腫瘤的療效觀察[J].中國修復重建外科雜志,2016,30(2):183188.