非妊娠期糖尿病巨大兒臨床分析
馮秀敏
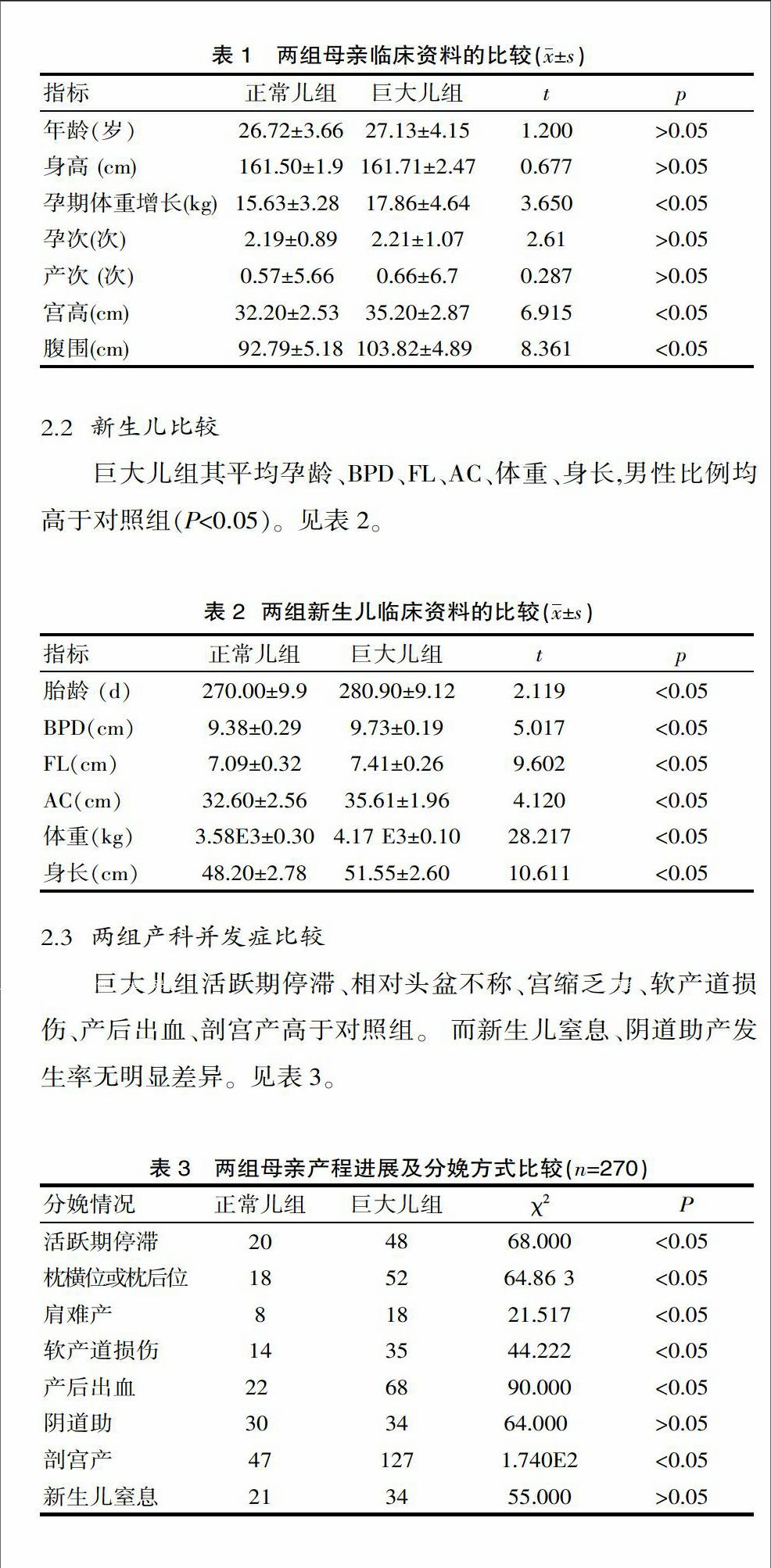
[摘要] 目的 探討非妊娠期糖尿病巨大兒的臨床特征及相關因素分析。 方法 整群選擇2012年6月—2014年6月在該院出生的非妊娠期糖尿病巨大兒和母親270例,隨機選擇同期分娩的270例正常體重兒或母親回顧性對照分析。 結果 非妊娠期糖尿病巨大兒平均胎齡、BPD、FL、AC、身長、體重分別為280.90 d、9.73 cm、7.41 cm、35.61 cm、51.55 cm 、4170 g,明顯高于對照組的270 d、9.38 cm、7.09 cm、32.60 cm、48.20 cm、3580 g,巨大兒組男性180例,多于對照組的119例;巨大兒母親的孕期體重增長17.86 kg,高于對照組的15.63 kg;巨大兒組產程進展及枕位異常100例、產后出血68例、剖宮產127例,而對照組分別為38例、22例及47例。 結論 非妊娠期糖尿病巨大兒以男性居多,其發生與母親孕期體重增長、宮高、腹圍因素有關,并導致母親分娩過程中產程進展異常發生率、產后出血率、剖宮產率顯著增加,積極預防非糖尿病巨大兒的發生是提高產科質量的重要措施。
[關鍵詞] 巨大兒;非妊娠期糖尿病;宮高;腹圍
[中圖分類號] R587.1 [文獻標識碼] A [文章編號] 1674-0742(2015)05(b)-0043-02
Clinical Anlysis of Non-gestational Diabetes Macrosomia
FENG Xiu-min
Department of Gynecology and ObStetrics, Tieying Hospital of Fengtai District, Beijing, 100079 China
[Abstract] Objective In this paper,the clinical characteristics and related factors of non-gestational diabetes macrosomia was explored. Methods 270 cases of non-gestational diabetes macrosomia(or mother) born during June 2012 -June 2014 were compared with 270 cases with normal-birth-weight newborn randomly selected in the same period for the retrospective case-control study in our hospital. Results The average gestational age, BPD, FL, AC, body length, body weight were 280.90 days, 9.73 cm, 7.41 cm, 35.61 cm, 51.55 cm, 4170 grams, apparently higher than 270 days, 9.38 cm, 7.09 cm, 32.60 cm, 48.20 cm, 3580 grams of the control group respectively;there were 180 cases of male in macrosomia group, more than the 119 cases in the control group. The mother's pregnancy weight gain was 17.86 kilograms, which was more than 15.63 kilograms of the control group. There were 100 cases labor progress and pillow abnormalities ,68 cases postpartum hemorrhage , 127 cases cesarean section in macrosomia group,while in the control group there were 38 cases, 22 cases and 47 cases respectively. Conclusion The male are in the majority in the non-gestational diabetes macrosomia, their incidences were related to their motherrs' weight gain, uterine height, and abdomen circumference, which led to the high rate of abnormal progress during the stages of labor, postpartum hemorrhage and ratio of cesarean section delivery significantly. So, positively prevent the happening of the diabetic macrosomia is one of the important measures to improve the quality of obstetrics.
[Key words] Macrosomia;Non-gestational diabetes;Uterine fundal height;Abdominal circumference
隨著家庭對孕產婦的重視、生活水平的改善及生活方式的改變,巨大兒的發生率呈逐年上升的趨勢,其中非糖尿病巨大兒所占比例增高。胎兒體重超過4000 g者稱為巨大兒,巨大兒屬于高危妊娠,對母親可造成陰道分娩過程中產程延長、難產、軟產道損傷、繼發性宮縮乏力、產后出血、手術助產、剖宮產率增加;對胎兒可導致新生兒產傷如肩難產、鎖骨骨折、臂叢神經損傷、顱內出血、新生兒窒息甚至死亡等[1]。因此,對其臨產特征及發生的相關因素進行探討具有重要意義。該研究采用病例對照方法對2012年6月—2014年6月在該院出生的非妊娠期糖尿病巨大兒270例及同期隨機分娩的正常體重兒270例進行回顧性分析,現報道如下。……

