Sv2/Rv3比值在定位流出道室性期前收縮或室性心動過速中的應用價值
胡喜田,陳勤聰,穆 東,李子莉,呂新湖,魏小剛
(河北省石家莊市第一醫院心內二科,河北 石家莊 050011)
Sv2/Rv3比值在定位流出道室性期前收縮或室性心動過速中的應用價值
胡喜田,陳勤聰,穆東,李子莉,呂新湖,魏小剛
(河北省石家莊市第一醫院心內二科,河北 石家莊 050011)
[摘要]目的探討V2導聯S波與V3導聯R波振幅(S-wave amplitude in lead V2divided by R-wave amplitude in lead V3,Sv2/Rv3)比值、胸前導聯移行區指數(transitional zone index,TZI)在鑒別右心室流出道(right ventricular outflow tract,ROVT)起源室性期前收縮( premature ventricular beat,PVB)/室性心動過速(right ventricular tachycardia,VT)與左心室流出道(Left ventricular outflow tract,LOVT )起源PVB/VT中的價值。方法回顧性分析成功進行射頻消融的60例流出道PVB/VT患者的心電圖和電生理資料,通過體表心電圖測取的Sv2/Rv3比值和TZI對PVB/VT的起源部位進行定位分析。結果60例患者均經過消融成功。消融靶點:ROVT起源45例,LOVT起源15例;LOVT起源PVB/VT的TZI較ROVT起源PVB/VT明顯小。TZI<0作為LOVT起源PVB/VT臨界值,其對LOVT起源PVB/VT的敏感度為80.0%,特異度為82.2%,準確度為81.7%,陽性預測值為60.0%,陰性預測值為92.5%。LOVT起源PVB/VT的Sv2/Rv3比值較ROVT起源PVB/VT明顯小。Sv2/Rv3比值<1.5作為LOVT起源PVB/VT臨界值,其對LOVT起源PVB/VT的敏感度為86.7%,特異度為84.4%,準確度為85.0%,陽性預測值為65.0%,陰性預測值為95.0%。結論Sv2/Rv3比值、TZI對流出道PVB/VT定位診斷具有較好的預測價值。
[關鍵詞]室性早搏復合征;心電描記術;導管消融術
doi:10.3969/j.issn.1007-3205.2015.07.005
流出道特發性室性心動過速(ventricular tachycardia,VT)或室性期前收縮(premature ventricular beat,PVB)最常見的起源部位為右心室流出道(right ventricular outflow tract,ROVT)、主動脈竇、肺動脈、希氏束附近等[1-4],心電圖表現為左束支傳導阻滯和電軸右偏。通過體表心電圖可以定位流出道PVB/VT的起源部位,為臨床提供參照,減少手術時間、費用、X線曝光時間。目前有幾種心電圖定位方法得到臨床推薦[5-8],但它們容易受到導聯位置、心臟解剖、心臟轉位、心室肥厚、體型、胸部畸形、優勢傳導通路存在等[6,9-11]影響,其準確度與實用性受到限制。本研究對射頻消融成功的60例流出道PVB/VT患者的心電圖和電生理資料進行回顧性分析,評價最新心電圖定位指標V2導聯S波與V3導聯R波振幅(S-wave amplitude in lead V2divided by R-wave amplitude in lead V3,Sv2/Rv3)比值[11]與臨床已驗證的胸前導聯移行區指數(transitional zone index,TZI)[7]在指數定位流出道VT、PVB的應用價值,提供新的定位流出道起源指標。
1資料與方法
1.1一般資料2010年1月—2014年2月河北省石家莊市第一醫院心內科連續進行射頻消融成功的流出道PVB/VT 60例,男性36例,女性24例,年齡18~65歲,平均( 42.5±13.3 )歲。超聲心動圖檢查除外心力衰竭患者,其中ROVT起源45例,左心室流出道(left ventricular outflow tract,LOVT)起源VT 15例。流出道PVB/VT的心電圖特點為:左束支傳導阻滯伴電軸右偏,Ⅱ、Ⅲ、aVF導聯有高振幅的R波,V1導聯QRS波為rS型。
1.2方法
1.2.1用Sv2/Rv3比值判斷流出道起源所有研究對象均在安靜環境下描記心電圖,用日本光電Cardimax Fx-740212導聯心電圖機,選擇12導聯同步描記心電圖。記錄PVB/VT發作時和竇性心律心電圖,心電圖振幅10 mm,速度25 mm/s,電極置于標準的胸前導聯和肢體導聯。特別關注胸前導聯V1位于胸骨右緣第Ⅳ肋間,V2位于胸骨左緣第Ⅳ肋間,因為不確切的導聯位置可能導致記錄的PVB/VT QRS波明顯改變[12]在同一12導聯心電圖上,應用游標卡尺進行PVB/VT和竇性心律時的心電圖分析。Sv2/Rv3比值測定相關定義:Sv2/Rv3比值是指PVB/VT在V2導聯QRS波的S波與V3導聯QRS的R波振幅的比值。測量患者心電圖PVB/VT在V2導聯QRS波的S波與V3導聯R波的幅度,并進行兩者振幅比值的計算,Sv2/Rv3比值≤ 1.5 時提示PVB/VT起源于LOVT,若>1.5時,提示起源于ROVT。見圖1。
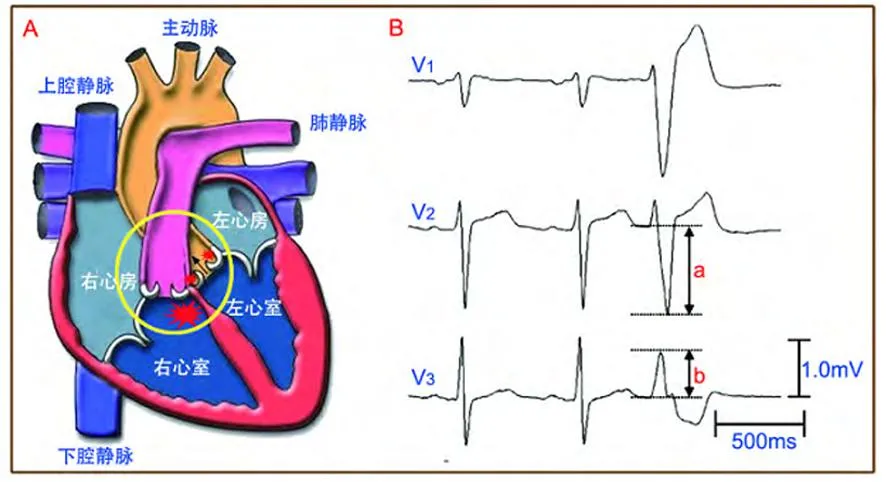
圖1流出道局部解剖關系與Sv2/Rv3比值測定示意圖
Figure 1A transition zone of outflow of anatomy and Sv2/Rv3
1.2.2用TZI判斷流出道起源按照Yoshida等[11]提出的方法測取TZI。確定移行區導聯:當胸導聯的R波與S波比值為0.9~1.1時則為移行區,正常時移行區位于V3或V4導聯。移行區積分:移行區所在的導聯數即為移行區的積分,如出現在導聯V4則積4分,出現在V4與V5導聯之間則積4.5分,見表1,圖2。移行區指數:用PVB或VT的移行區積分減去竇性心律的移行區積分為移行區指數,當其<0時提示位于主動脈竇內,≥0時提示位于ROVT。

表1 胸前導聯R波移行部位與胸前導

圖2流出道解剖與胸前導聯移行區積分示意圖
Figure 2A transition zone of outflow of anatomy and chest lead transitional zone index
1.3統計學方法應用SPSS 18.0軟件進行統計學分析。受試者工作曲線分析得出最佳臨界值,計算敏感度、特異度、準確度、陽性預測值、陰性預測值。P<0.05為差異有統計學意義。
2結果
2.1電生理標測消融結果患者手術即刻成功60例,ROVT消融成功45例,LOVT消融成功15例。60例中PVB 46例、VT 14例。
2.2TZI對流出道PVB/VT定位診斷60例患者12導聯心電圖中,有49例與電生理檢查結果相符,其準確度為81.7%(49/60),其中對ROVT起源PVB/VT的準確度為82.2%(37/45),對LOVT起源PVB/VT的準確度為80.0%(12/15)。TZI<0定位LOVT起源PVB/VT的敏感度、特異度、準確度、陽性預測值和陰性預測值分別為80.0%、82.2%、81.7%、60.0%和92.5%。Sv2/Rv3比值對流出道PVB/VT定位診斷:60例患者12導聯心電圖中,有51例與電生理檢查結果相符,其準確度為85.0%(51/60),其中對ROVT起源PVB/VT的準確度為84.4%(38/45),對LOVT起源PVB/VT的準確度為86.7%(13/15)。 Sv2/Rv3比值≤1.5定位LOVT起源PVB/VT的敏感度、特異度、準確度、陽性預測值和陰性預測值分別為86.7%、84.4%、85.0%、65.0%和95.0%。后者指標更好,見表2。

表2 TZI、Sv2/Rv3比值定位LOVT起源PVB/VT
3討論
射頻消融是治療流出道PVB/VT的主要方法之一,對藥物療效差、心臟擴大心功能下降的患者能起到根治作用[3,13-18];但LOVT起源PVB/VT和ROVT起源PVB/VT的消融術式、 有效消融靶點等方面都存在明顯不同,因而迫切需要術前心電圖能作出更高水平的鑒別,目前心電圖已為臨床提供良好的借鑒。由于ROVT和主動脈竇、大靜脈、二尖瓣環與主動脈竇連接處等解剖關系鄰近,以及心臟轉位、胸廓畸形等影響使心電圖定位PVB/VT的起源部位存在一定的誤差,尋找一種敏感度和特異度均高的心電圖指標成為臨床心電圖學研究的熱點。
LVOT 與 RVOT毗鄰,兩者均與主動脈根部相毗鄰,主動脈根部占據心臟的中心部位,ROVT位于主動脈根部左側前面[16]。這些解剖特點造成起源于主動脈竇的PVB/VT較ROVT起源的PVB/VT在胸前V1、V2導聯R波持續時間更長,R/S比值更高[11]。因此,應用V1、V2導聯R波或S波幅度可能找到合理的心電圖定位指標,解剖分析顯示V3導聯位置與ROVT的距離較主動脈根部更近。解剖特點決定V3導聯R波幅度與V2導聯S波幅度可用于定位流出道PVB/VT起源,具有較高的敏感度和特異度,Sv2/Rv3比值較上述兩項指標的敏感度、特異度更高。
Quyang等[5]在心電圖進行鑒別的研究中發現,起源于主動脈竇的PVB/VT,其 V1導聯QRS波的R波時限指數和R波振幅指數均明顯大于ROVT起源的PVB/VT的相應值,提出鑒別兩者的心電圖標準:①先確定PVB/VT具有心室流出道起源的一般心電圖特點;②胸導聯的移行區位于V2導聯;③V1導聯的R波時限指數≥50%,R波振幅指數≥30%。凡滿足上述條件的PVB/VT則起源于主動脈竇,未能滿足者起源于ROVT。當患者的心臟無明顯轉位時,上述診斷與鑒別標準的敏感度高達80%,特異度為79%。此心電圖鑒別標準在臨床應用時發現,當患者原本竇性心律就存在心臟轉位時,能明顯影響PVB/VT起源部位精確定位。Brian等[6]在研究中發現,R波時限指數和R/S振幅指數對心臟轉位的患者中定位診斷價值降低,提出一個“V2移行比”的概念,即VT時R/R+S或竇性心律時R/R+S的比值來克服心臟轉位等影響,LOVT起源的VT的V2移行比顯著大于ROVT起源的VT,當V2轉變比>0.6時,預測LOVT起源VT的準確度為91%,而當VT時胸前導聯移行晚于竇性心律時,則可100%排除LOVT起源的可能。2011年,Yoshida等[7]提出TZI的概念可用于ROVT或LOVT起源PVB/VT的鑒別,并具有鑒別兩者較高的敏感度和特異度,可以避免心室轉位和本身心電圖干擾作用,進一步提高定位診斷的準確度。2014年,Yoshida等[11]再次提出一項新指標Sv2/Rv3比值,通過觀察207例流出道PVB/VT并成功進行了射頻消融治療的患者,其中心律失常起源于ROVT 154例,起源于LOVT 53例,Sv2/Rv3比值鑒別兩者的敏感度為89%,特異度為94%,較R波時限指數和R/S振幅指數,Sv2/Rv3定位更加準確,且差異有統計學意義;該組病例不僅包括器質性心臟病患者,而且包括非器質性心臟病患者,拓寬了心電圖定位PVB/VT起源的應用范圍。
本研究通過回顧性分析60例流出道PVB/VT心電圖顯示:TZI與射頻消融的準確度為81.7%(49/60),其中對ROVT起源PVB/VT的準確度為82.2%(37/45),對LOVT起源PVB/VT的準確度為80.0%(12/15);Sv2/Rv3比值與射頻消融手術的準確度為85.0%(51/60),其中對ROVT起源PVB/VT的準確度為84.4%(38/45),對LOVT起源PVB/VT的準確度為86.7%(13/15);TZI<0定位主動脈竇起源心律失常的敏感度為80.0%,特異度為82.2%,準確度為81.7%,陽性預測值為60.0%,陰性預測值92.5%;Sv2/Rv3比值≤1.5的敏感度為86.7%,特異度為84.4%,準確度為85.0%,陽性預測值為65.0%,陰性預測值為95.0%。表明Sv2/Rv3比值較胸前導聯移行比有更好的準確度和特異度,傾向于更有臨床應用的優勢,這與Yoshida 等[7,11]的研究一致。關于兩者的優劣需要通過擴大樣本例數進一步研究。通過臨床驗證顯示,TZI與Sv2/Rv3比值均是定位流出道起源部位的可靠指標,有一定的臨床應用價值,值得臨床推廣應用。
本研究手術例數較少,且為回顧性研究,研究入組分析時間跨度較長,對心電圖的分析靠手測,可能存在標準化不足,影響研究的可靠性。今后如能增加手術例數,進行前瞻性研究設計,可能會獲得更為可靠的臨床研究結果。
[參考文獻]
[1]Yamada T,McElderry HT,Okada T,et al.Idiopathic left ventricular arrhythmias originating adjacent to the left aortic sinus of valsalva: electrophysiological rationale for the surface electrocardiogram[J].J Cardiovasc Electrophysiol,2010,21(2): 170-176.
[2]Yamada T,McElderry HT,Doppalapudi H,et al.Idiopathic ventricular arrhythmias originating from the left ventricular summit: anatomic concepts relevant to ablation[J].Circ Arrhythm Electrophysiol,2010,3(6):616-623.
[3]Aliot EM,Stevenson WG,Almendral-Garrote JM,et al.EHRA/HRS Expert Consensus on Catheter Ablation of Ventricular Arrhythmias : developed in a partnership with the European Heart Rhythm Association(EHRA),a Registered Branch of the European Society of Cardiology (ESC),and the Heart Rhythm Society(HRS);in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA)[J].Europace,2009,11(6):771-817.
[4]Yokokawa M,Good E,Crawford T,et al.Reasons for failed ablation for idiopathic right ventricular outflow tract-like ventricular arrhythmias[J].Heart Rhythm,2013,10(8):1011-1018.
[5]Ouyang F,Fotuhi P,Ho SY,et al.Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp: electrocardiographic characterization for guiding catheter ablation[J].J Am Coll Cardiol,2002,39(3):500-508.
[6]Brian BP,Park RE,Marchlinski FE,et al.The V(2) transition ratio: a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin[J].J Am Coll Cardiol,2011,57(22):2255-2262.
[7]Yoshida N,Inden Y,Uchikawa T,et al.Novel transitional zone index allows more accurate differentiation between idiopathic right ventricular outflow tract and aortic sinus cusp ventricular arrhythmias[J].Heart Rhythm,2011,8(3):349-356.
[8]Cheng Z,Cheng K,Deng H,et al.The R-wave deflection interval in lead V3 combining with R-wave amplitude index in lead V1: a new surface ECG algorithm for distinguishing left from right ventricular outflow tract tachycardia origin in patients with transitional lead at V3[J].Int J Cardiol,2013,168(2):1342-1348.
[9]Yamada T,Murakami Y,Yoshida N,et al.Preferential conduction across the ventricular outflow septum in ventricular arrhythmias originating from the aortic sinus cusp[J].J Am Coll Cardiol,2007,50(9):884-891.
[10]王宇彬,楚建民,宋書凱,等.室間隔優勢傳導導致主動脈竇起源室性早搏呈左束支阻滯傳導圖形[J].中華心血管病雜志,2013,41(1):13-17.
[11]Yoshida N,Yamada T,McElderry HT,et al.A novel electrocardiographic criterion for differentiating a left from right ventricular outflow tract tachycardia origin: the V2S/V3R index[J].J Cardiovasc Electrophysiol,2014,25(7):747-753.
[12]Anter E,Frankel DS,Marchlinski FE,et al.Effect of electrocardiographic lead placement on localization of outflow tract tachycardias[J].Heart Rhythm,2012,9(5):697-703.
[13]李健,于波,楊耀,等.冠狀動脈竇內射頻消融室性心律失常的研究[J].臨床心電學雜志,2013,22(1):37-40.
[14]吳曉羽,李為民,譚震,等.起源于左ROVT心動過速和早搏的射頻導管消融治療[J].中華心血管病學雜志,2007,35(7):620-624.
[15]路長鴻,常瑜,朱凌華,等.射頻導管消融治療主動脈左冠狀竇室性心律失常療效觀察[J].中國循證心血管醫學雜志,2011,3(2):136-137.
[16]Anderson RH.Clinical anatomy of the aortic root[J].Heart,2000,84(6):670-673.
[17]Fang F,Wen C,Yang L,et al.Radiofrequency ablation can reverse the structural remodeling caused by frequent premature ventricular contractions originating from the right ventricular outflow tract even in a“normal heart”[J].Clinics(Sao Paulo),2013,68(10):1312-1317.
[18]Penela D,van Huls van Taxis C,Aguinaga L.Neurohormonal,structural,and functional recovery pattern after premature ventricular complex ablation is independent of structural heart disease status in patients with depressed left ventricular ejection fraction a Prospective multicenter study[J].J Am Coll Cardiol,2013,62(13):1195-1202. T,McElderry HT,Okada T,et al.Idiopathic left ventricular arrhythmias originating adjacent to the left aortic sinus of valsalva: electrophysiological rationale for the surface electrocardiogram[J].J Cardiovasc Electrophysiol,2010,21(2): 170-176.
[2]Yamada T,McElderry HT,Doppalapudi H,et al.Idiopathic ventricular arrhythmias originating from the left ventricular summit: anatomic concepts relevant to ablation[J].Circ Arrhythm Electrophysiol,2010,3(6):616-623.
[3]Aliot EM,Stevenson WG,Almendral-Garrote JM,et al.EHRA/HRS Expert Consensus on Catheter Ablation of Ventricular Arrhythmias : developed in a partnership with the European Heart Rhythm Association(EHRA),a Registered Branch of the European Society of Cardiology (ESC),and the Heart Rhythm Society(HRS);in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA)[J].Europace,2009,11(6):771-817.
[4]Yokokawa M,Good E,Crawford T,et al.Reasons for failed ablation for idiopathic right ventricular outflow tract-like ventricular arrhythmias[J].Heart Rhythm,2013,10(8):1011-1018.
[5]Ouyang F,Fotuhi P,Ho SY,et al.Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp: electrocardiographic characterization for guiding catheter ablation[J].J Am Coll Cardiol,2002,39(3):500-508.
[6]Brian BP,Park RE,Marchlinski FE,et al.The V(2) transition ratio: a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin[J].J Am Coll Cardiol,2011,57(22):2255-2262.
[7]Yoshida N,Inden Y,Uchikawa T,et al.Novel transitional zone index allows more accurate differentiation between idiopathic right ventricular outflow tract and aortic sinus cusp ventricular arrhythmias[J].Heart Rhythm,2011,8(3):349-356.
[8]Cheng Z,Cheng K,Deng H,et al.The R-wave deflection interval in lead V3 combining with R-wave amplitude index in lead V1: a new surface ECG algorithm for distinguishing left from right ventricular outflow tract tachycardia origin in patients with transitional lead at V3[J].Int J Cardiol,2013,168(2):1342-1348.
[9]Yamada T,Murakami Y,Yoshida N,et al.Preferential conduction across the ventricular outflow septum in ventricular arrhythmias originating from the aortic sinus cusp[J].J Am Coll Cardiol,2007,50(9):884-891.
[10]王宇彬,楚建民,宋書凱,等.室間隔優勢傳導導致主動脈竇起源室性早搏呈左束支阻滯傳導圖形[J].中華心血管病雜志,2013,41(1):13-17.
[11]Yoshida N,Yamada T,McElderry HT,et al.A novel electrocardiographic criterion for differentiating a left from right ventricular outflow tract tachycardia origin: the V2S/V3R index[J].J Cardiovasc Electrophysiol,2014,25(7):747-753.
[12]Anter E,Frankel DS,Marchlinski FE,et al.Effect of electrocardiographic lead placement on localization of outflow tract tachycardias[J].Heart Rhythm,2012,9(5):697-703.
[13]李健,于波,楊耀,等.冠狀動脈竇內射頻消融室性心律失常的研究[J].臨床心電學雜志,2013,22(1):37-40.
[14]吳曉羽,李為民,譚震,等.起源于左ROVT心動過速和早搏的射頻導管消融治療[J].中華心血管病學雜志,2007,35(7):620-624.
[15]路長鴻,常瑜,朱凌華,等.射頻導管消融治療主動脈左冠狀竇室性心律失常療效觀察[J].中國循證心血管醫學雜志,2011,3(2):136-137.
[16]Anderson RH.Clinical anatomy of the aortic root[J].Heart,2000,84(6):670-673.
[17]Fang F,Wen C,Yang L,et al.Radiofrequency ablation can reverse the structural remodeling caused by frequent premature ventricular contractions originating from the right ventricular outflow tract even in a“normal heart”[J].Clinics(Sao Paulo),2013,68(10):1312-1317.
[18]Penela D,van Huls van Taxis C,Aguinaga L.Neurohormonal,structural,and functional recovery pattern after premature ventricular complex ablation is independent of structural heart disease status in patients with depressed left ventricular ejection fraction a Prospective multicenter study[J].J Am Coll Cardiol,2013,62(13):1195-1202.
(本文編輯:許卓文)
[中圖分類號]R541.7
[文獻標志碼]A
[文章編號]1007-3205(2015)07-0759-05
V2S/V3R index for differentiating origin of idiopathic outflow tract ventricular arrhythmia
HU Xi-tian,CHEN Qin-cong,MU Dong,LI Zi-li,LV Xin-hu,WEI Xiao-gang
(Department of Cardiology,the First Hospital of Shijiazhuang City,Shijiazhuang 050011,China)
[Abstract]ObjectiveTo explore the value of S-wave amplitude in lead V2divided by R-wave amplitude in lead V3(Sv2/Rv3) and transitional zone index(TZI)for distinguishing the ROVT PVB/VT from left ventricular outflow tract(LOVT).MethodsRetrospective analysis was made in the electrocardiogram and electrophysiology from 60 patients with outflow tract PVB/VT,differentifating the ROVT PVB/VT from LOVT by Sv2/Rv3 index and TZI in electrocardiogram.ResultsA total of 60 patients underwent radiofrequency catheter ablation successfully,originating from right ventricular outflow tract(ROVT) in 45 cases,originating from LOVT in 15 cases.The TZI was significantly lower in LOVT origin than in RVOT origin.A cutoff value of TZI<0 predicting LOVT origin with sensitivity 80.0%,specificity 82.2%,accuracy 81.7%,positive predictive value 60.0% and negative predictive value 92.5%.The Sv2/Rv3 index was significantly lower in LOVT origin than in RVOT origin.A cutoff value of Sv2/Rv3 index≤1.5 predicting LOVT with sensitivity 86.7%,specificity 84.4%,accuracy 85.0%,positive predictive value 65.0% and negative predictive value 95.0%.ConclusionWe presented a new simple surface ECG algorithm,Sv2/Rv3 index and transitional zone index,which can reliably distinguish LVOT from RVOT origin in idiopathic outflow tract PVB/VT.
[Key words]ventricular premature complexes;electrocardiography;catheter ablation

