心理護理對產后抑郁癥的預防
孫素改,李春雷,左喜愛
(張家口市第二醫院,河北 張家口 075000)
?
心理護理對產后抑郁癥的預防
孫素改,李春雷,左喜愛
(張家口市第二醫院,河北 張家口 075000)
摘要:目的觀察心理護理對產后抑郁癥發生的預防效果。方法選取定期產檢并分娩的孕婦84例,隨機分為治療組和對照組,各42例,對照組給予孕婦常規產前知識講座、定期心理培訓;治療組在對照組的常規處置基礎上,對親密家庭人員和孕婦行心理干預及預防產后抑郁癥相關知識講座,2組產婦均在產后15 d采用愛丁堡產后抑郁自評量表(EPDS)、生活質量評定量表(QOL)進行評分,并對比2組產后抑郁癥發生率。結果治療組EPDS評分明顯低于對照組(P<0.05),QOL評分明顯高于對照組(P<0.05),治療組抑郁癥發生率明顯低于對照組(P<0.05)。結論親密家庭人員和孕婦同時進行心理干預培訓及預防產后抑郁癥相關知識講座能明顯降低孕婦產后抑郁率,對預防產后抑郁癥發生作用顯著。
關鍵詞:親密家庭人員;心理干預;產后抑郁癥
產后抑郁癥是一組非精神的抑郁綜合征,大多發病在產后2周內,產婦表現為失眠乏力、情緒激動、悲傷、抑郁等,不僅影響產婦的身心健康,還對嬰兒的身心健康也有一定的影響[1-3],發病率為3.8%~16.7%,且有逐年上升的趨勢[4-6]。本研究不僅對孕婦進行心理干預治療,同時對產婦親密家庭人員進行心理培訓,并講解預防產后抑郁癥相關知識,取得良好效果。報道如下。
1資料與方法
1.1一般資料選取2013年1月—12月我院定期產檢并分娩的符合納入標準的孕婦84例,隨機分為治療組及對照組,各42例。治療組年齡22~35歲;1胎24例,2胎18例;對照組年齡21~35歲;1胎29例,2胎13例。入選產婦產前均無心理障礙,頭腦清晰,無心理及精神方面疾病,自愿參加調查,并能獨立完成問卷。
1.2治療方法2組產婦產前均定期實施常規產前知識講座 、定期孕婦心理培訓。治療組在此基礎上對家庭親密人員共同進行心理培訓及預防產后抑郁癥相關知識講座,包括:1)入院前孕婦分娩知識宣教,讓孕婦及親密家庭人員明白抑郁是產后最常見的心理問題,容易引起產婦抑郁的問題如母親角色轉換,嬰兒哺乳問題等,由專業人員對孕婦及親密家庭人員進行心理護理培訓。2)讓親密家庭人員積極和孕、產婦交流溝通, 激發孕、產婦對周圍事物、生活的興趣,減輕產婦產后出現情緒不穩,擔心、焦慮等,從而避免發展成抑郁癥,并講解產后抑郁癥相關知識。3)親密家庭人員為產婦提供親密、舒適的家庭休養環境,滿足產婦的生活需要,更多關心和體貼產婦,隨時進行心理、生活的幫助,如鼓勵產婦堅持母乳喂養嬰兒的信心,幫助產婦康復鍛煉,使產婦放松身心,產生愉悅的情緒 。有研究表明,親密家庭人員的情感支持對產婦心理可起到正向性作用,能最大程度滿足產婦心理需求[7]。
1.3調查方法2組產婦均于產后15 d進行問卷調查,問卷發放及評分固定由3名經驗豐富的主管護師進行處理,采用愛丁堡產后抑郁自評量表(EPDS)進行抑郁程度評分,EPDS 共 10項,10項相加滿分為30 分。陰性:總分≤12分;陽性:總分>13分,評分陽性產婦即可確認為產后抑郁癥。采用生活質量評定量表(QOL)進行生存質量評分,QOL共6個領域,24個方面以及1個一般健康狀況和生存質量的評分,得分越高生存質量越好。評價問卷由3名經驗豐富的主管護師當場發放,由產婦親自填寫完成后回收,并由主管護師確認問卷真實有效。2組共發放問卷84份,全部有效回收。

2結果
2.12組分娩前后EPDS、QOL評分比較見表1。

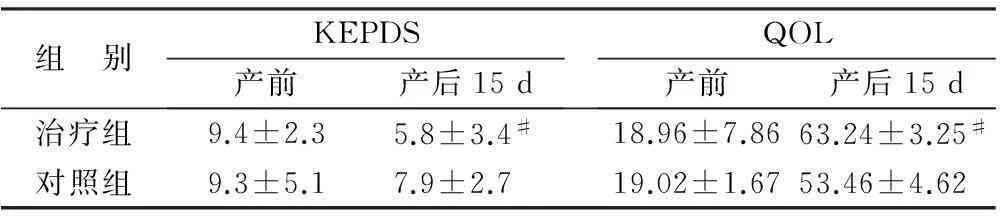
組 別KEPDS產前產后15dQOL產前產后15d治療組9.4±2.35.8±3.4#18.96±7.8663.24±3.25#對照組9.3±5.17.9±2.7 19.02±1.6753.46±4.62
注:與對照組比較,#P<0.05
2.22組抑郁癥發生率比較治療組抑郁自評量表陽性者3例(7.1%),對照組陽性者7例(16.7%),2者比較,差異有統計學意義(P<0.05)。
3小結
產后抑郁癥的發病是多方面因素相互作用的結果,主要有生物學因素、心理因素和社會因素等3個方面[8-10]。孕婦的心理情緒與親密家庭人員各方面的支持密不可分,本研究通過專業的心理知識培訓及預防產后抑郁癥相關知識講座,親密家庭人員更了解孕產婦生理、心理的變化以及抑郁癥發生的危險因素。發揮親密家庭人員的主觀能動性,應用學習的專業心理知識去護理孕、產婦,從多方面了解孕、產婦的心理情緒,對其擔心、焦慮的問題隨時給予解答,幫助孕、產婦克服各種不良情緒的產生,避免各種心理障礙誘發產后抑郁癥的發生[11-13]。
參考文獻:
[1]BENER A,BURGUT F T,GHULOUM S,et al.A study of postpartum depression in a fast developing country:prevalence and related factors[J].International Journal of Psychiatry in Medicine,2012,43(4):325-337.
[2]VIGOD S L.Prevalence and risk factors for postpartum deression among women with preterm and low-birth-weight infants:a systematic review[J].BJOG :an International Journal of Obstetrics and Gynaecology,2010,117(5):540-550.
[3]MOSHKI M,BALOOCHI BEYDOKHTI T,CHERAVI K.The effect of educational intervention on prevention of postpartum depression:an application of health locus of control[J].Journal of Clinical Nursing,2014,23(15/16):2256-2263.
[4]BOBO W V,YAWN B P.Concise review for physicians and other clinicians:postpartum depression[J].Mayo Clinic Proceedings,2014,89(6):835-844.
[5]VLIEGEN N,CASALIN S,LUYTEN P.The course of postpartum depression[J].Harvard Review of Psychiatry,2014,22(1):1-22.
[6]SLATTENGREN A H,PRASAD S,KAISERUDDIN M A.PURLs:should you screen for postpartum depression?[J].The Journal of Family Practice,2013,62(11):E1-E3.
[7]姜越娟,姜群群.產后抑郁癥的心理學研究進展[J].中國藥物經濟學,2013(5):542-543.
[8]DUDEK D,JAESCHKE R,SIWEK M,et al.Postpartum depression:identifying associations with bipolarity and personality traits.Preliminary results from a cross-sectional study in Poland[J].Psychiatry Research,2014,215(1):69-74.
[9]GAILLARD A,LE STRAT Y,MANDELBROT L,et al.Predictors of postpartum depression:prospective study of 264 women followed during pregnancy and postpartum[J].Psychiatry Research,2014,215(2):341-346.
[10]SOCKOL L E,EPPERSON C N,BARBER J P.Preventing postpartum depression:a meta-analytic review[J].Clinical Psychology Review,2013,33(8):1205-1217.
[11]STUART S,KOLEVA H.Psychological treatments for perinatal depression[J].Best Practice & Research Clinical Obstetrics & Gynaecology,2014,28(1):61-70.
[12]VENKATESH K K,ZLOTNICK C,TRICHE E W,et al.Accuracy of brief screening tools for identifying postpartum depression among adolescent mothers[J].Pediatrics,2014,133(1):45-53.
[13]朱躍蘭,唐啟盛,楊歆科,等.產后抑郁癥生物學相關病因及發病機制研究進展[J].北京中醫藥,2013(3):168-176.
Psychological nursing in preventing postpartum depression
SUN Sugai,LI Chunlei,ZUO Xiai
(The Second Hospital of Zhangjiakou City in Hebei Province,Zhangjiakou 075000,Hebei Province,China)
Abstract:ObjectiveTo observe the effect of professional psychological intervention to the pregnant women and their intimate family members in preventing the occurrence of postpartum depression.MethodsA total of 84 pregnant women who came for regular antenatal examination and delivery were included in the study and randomized into the observation group and the control group with 42 cases in each group.The pregnant women in the control group were given routine prenatal knowledge lecture and regular psychological training.On this basis,the pregnant women in the observation group were given psychological intervention to the pregnant women and their intimate family members and related knowledge lecture about how to prevent the postpartum depression.EPDS and QOL were used for scoring for the pregnant women in the two groups 15 d after delivery.The occurrence rate of postpartum depression in the two groups was compared.ResultsEPDS score in the observation group was significantly lower than that in the control group (P<0.05),while QOL score was significantly higher than that in the control group (P<0.05).he occurrence rate of depression in the observation group was significantly lower than that in the control group (P<0.05).ConclusionPsychological intervention to the pregnant women and their intimate family members and related knowledge lecture about how to prevent the postpartum depression can significantly reduce the postpartum depression rate with a significant effect to prevent the postpartum depression.
Keywords:intimate family members;psychological intervention;postpartum depression
(收稿日期:2015-10-20)
文章編號:2095-6258(2016)01-0156-03
中圖分類號:R248.3
文獻標志碼:A
作者簡介:孫素改(1971-),女,大學本科,主管護師,主要從事婦產科臨床研究。
基金項目:河北省科技研究與發展指導項目(1021957D)。
DOI:10.13463/j.cnki.cczyy.2016.01.054