膀胱孤立性纖維性腫瘤1例報告
——影像與病理分析
武日江,張輝,王效春,譚艷,秦江波,王樂,張磊
WU Ri-jiang1, ZHANG Hui2*, WANG Xiao-chun2, TAN Yan2, QIN Jiang-bo2, WANG Le2, ZAHNG Lei2
膀胱孤立性纖維性腫瘤1例報告
——影像與病理分析
武日江1,張輝2*,王效春2,譚艷2,秦江波2,王樂2,張磊2
WU Ri-jiang1, ZHANG Hui2*, WANG Xiao-chun2, TAN Yan2, QIN Jiang-bo2, WANG Le2, ZAHNG Lei2
孤立性纖維瘤;磁共振成像;擴散加權成像;病理學
患者,女,85歲,主因尿痛、排尿不暢、左下腹疼痛2月余入院,無尿頻、尿急、血尿等不適,尿量較少。專科檢查:恥骨聯合上膀胱區隆起,觸及質硬包塊,活動度欠佳。
盆腔CT及MRI檢查,CT平掃示膀胱內巨大混雜密度軟組織腫塊影,等低密度相間分布,邊界清,大小約9 cm×13 cm×12 cm (左右徑×前后徑×上下徑),增強掃描病灶呈地圖樣不均勻強化、持續強化(圖1~3)。MRI平掃示膀胱巨大軟組織腫塊影,T1WI呈稍低信號,T2WI呈混雜信號,擴散加權成像(diffusion weighted imaging,DWI)為不均勻稍高信號影(圖4~8),動態增強掃描動脈期不均勻強化,靜脈期及延遲期呈持續性強化、延遲強化(圖9~12)。患者于2016年3月18日行膀胱部分切除術,術中見膀胱巨大腫物,基底位于膀胱三角區,突入腔內,表面光滑,電刀將黏膜做橫行切口,在黏膜下鈍性分離腫物,將腫物完整分離后切除腫物,并送病理。
病理檢查:標本肉眼所見:腫物大小約10 cm×13 cm×11 cm,縱行剖開見腫物內部由核心及外層組成,核心為魚肉樣,外層大小約4 cm,粉紅色。鏡檢:低倍鏡下腫瘤境界清楚,由交替分布的細胞豐富區和細胞稀疏區及血管外皮瘤樣區域構成,瘤細胞呈條束狀。高倍鏡下腫瘤細胞呈梭形,胞質少、紅染,核染色質均勻,核仁不明顯,未見核分裂象(圖13)。免疫組化:CD31(-)、CD34(+)(圖14)、CD56(+)、CgA (-)、CK20(-)、CK7(-)、HMB45(-)、melan-A (-)、S-100(-)、SMA (-)、Syn (-)。
病理診斷:(膀胱)孤立性纖維性腫瘤(低度惡性)。
討論 SFT由Klemperer和Rabin首次提出[1],早期認為SFT起源于間皮或間皮下間葉細胞。隨后學者采用免疫組化技術及電鏡對其進行研究,認為SFT起源于CD34陽性的樹突狀間葉細胞,具有向纖維母細胞、肌纖維母細胞、血管外皮細胞等分化的特征[2]。可發生于身體多處,原發于膀胱的SFT非常罕見。
膀胱SFT臨床表現為血尿、尿路刺激癥、盆腔壓迫癥狀,手術切除是治療該腫瘤的主要方案[3]。肉眼觀SFT呈界限清楚的孤立性實性腫塊,呈灰白至棕褐色,少數可見出血、囊變等,鏡下最重要的特點是:富細胞區與細胞稀少區交替排列,有致密瘢痕樣膠原沉積以及血管外皮瘤樣區[4]。通常CD34是比較特異和敏感的免疫標記物[5-6]。
影像學表現:CT平掃多為混雜密度軟組織腫塊影,腫瘤體積較大,SFT一般無鈣化,增強掃描動脈期,腫塊呈地圖樣不均勻強化,靜脈及延遲期病變強化范圍擴大、密度逐漸趨向均勻,呈“快進慢出”型強化[7]。本病例CT 表現與之相仿。
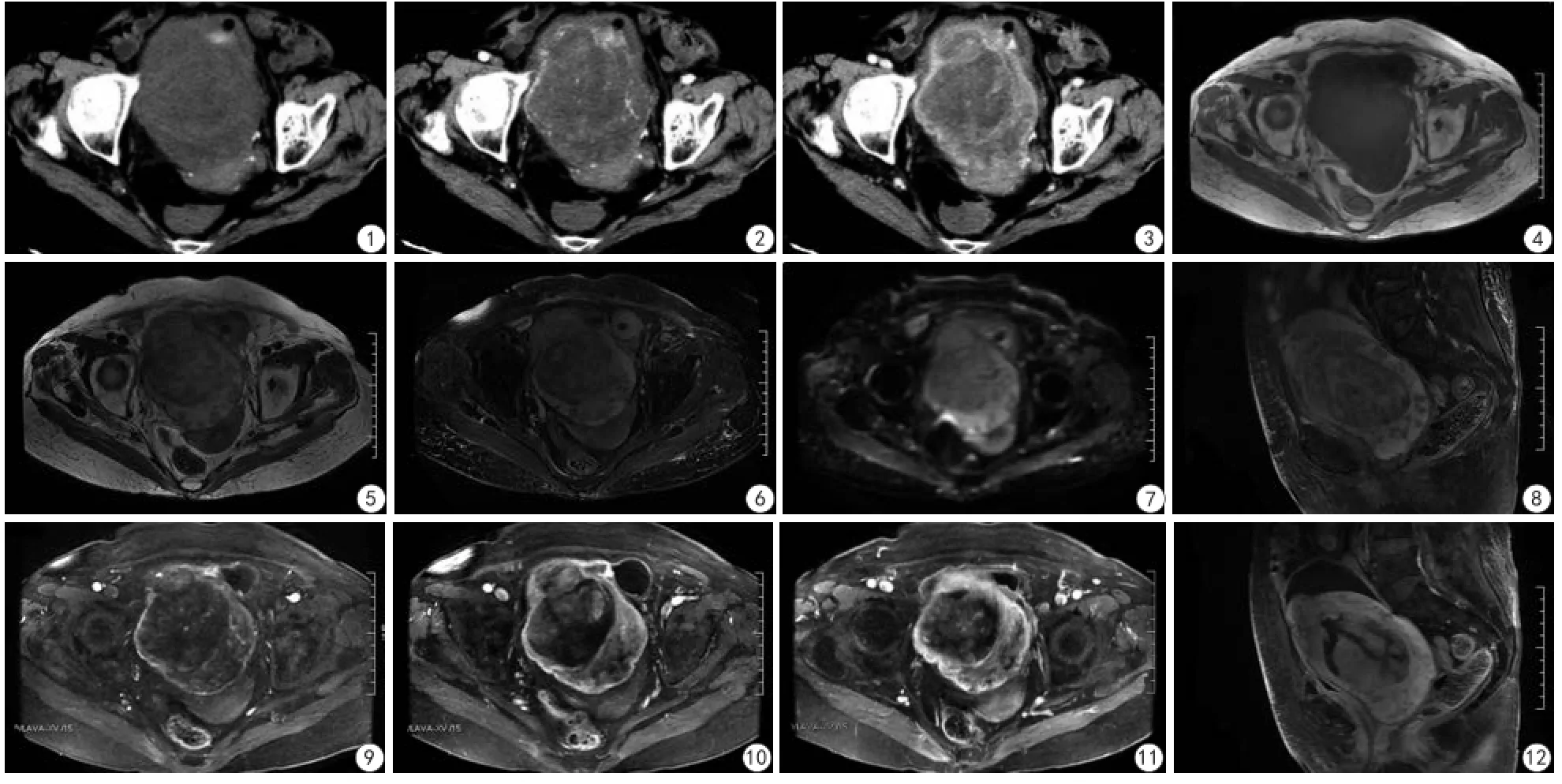
圖1 ~12 患者,女,85歲。圖1 CT平掃示膀胱巨大混雜密度軟組織腫塊,邊界清;圖2~3 CT增強掃描病灶呈地圖樣不均勻強化、持續強化;圖4~8 MRI平掃示膀胱巨大軟組織腫塊影,T1WI呈稍低信號,T2WI呈混雜信號,DWI呈不均勻稍高信號影;圖9~12 MRI動態增強掃描動脈期不均勻強化,靜脈期及延遲期呈持續性強化、延遲強化Fig. 1—12 Patient, female, 85 years old. Fig.1 Plain CT images showed that a huge soft tissue mass in the bladder, and its boundary was clear; Fig.2—3 Enhanced CT images showed that the tumor was presented as map-like inhomogeneous enhancement and delayed enhancement; Fig.4—8 On T1 weighted images, there was heterogeneous mild hypointense. On T2 weighted images, there was heterogeneous mixed signal. On diffusion weighted images, there was a little high signal; Fig.9—12 Dynamic enhanced scan demonstrated inhomogeneous enhancement on artery phase and progressive enhancement on portal and delayed phase.
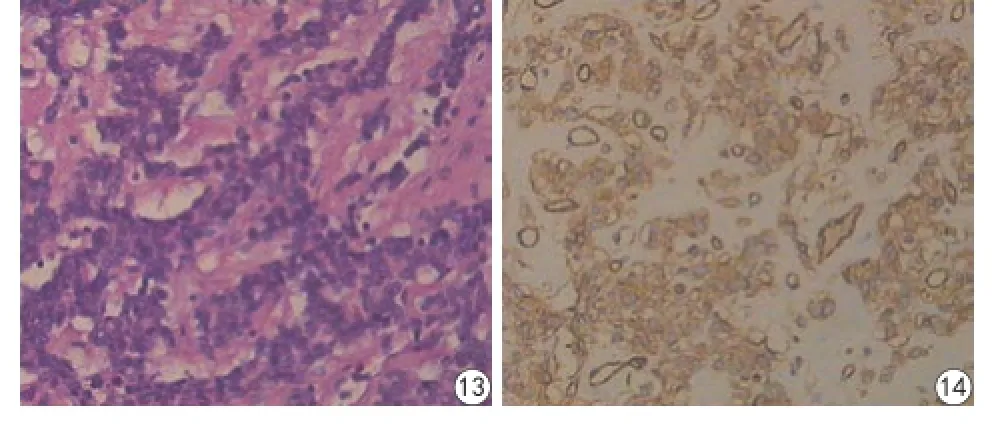
圖13 ~14 患者,女,85歲。圖13 腫瘤富細胞豐富區與乏細胞區交替分布,瘤細胞呈條束狀排列,膠原、間質血管豐富(HE ×200);圖 14 免疫組 織化學檢查示孤立性 纖維性腫瘤 (solitary fibrous tumor,SFT )細胞胞漿CD34+( ×200)Fig. 13—14 Patient, female, 85 years old. Fig.13 Hypercellular and hypocellular areas were alternated in the tumor. The tumor cells were spindleshaped and arranged in bundles or helicoid pattern with obvious interstitial blood vessel (HE ×200); Fig.14 By immunohistochemistry, the tumor cells were positive for CD34+ ( ×200).
MRI信號特點常可反映腫瘤的組織特征。SFT在T1WI上多呈等低信號,T2WI呈混雜信號[7]。有學者認為T2WI低信號區是由于病灶內富含膠原纖維基質、細胞結構稀疏所致,等高信號區是由富細胞區構成[8-9]。SFT增強掃描呈明顯不均勻強化、持續強化、延遲強化,并且認為腫瘤的持續強化區對應于組織學上的富細胞區、富血管區,延遲強化區對應于膠原組織或細胞結構稀疏區[8,10]。本病例在T1WI上呈等低信號,在T2WI上呈混雜信號,DWI為不均勻稍高信號,動態增強掃描動脈期T2WI上等信號區中度強化,靜脈期及延遲期持續性強化,T2WI上高信號及低信號區呈延遲強化,部分低信號區各期均未強化。鏡下瘤體內見富細胞區、乏細胞區交替分布,較多間質血管及膠原纖維,由此可解釋富細胞早期中度強化,持續性強化,乏細胞區、膠原纖維區及黏液樣變性造成細胞外間隙擴大,對比劑在細胞外間隙內聚積,導致呈延遲強化的特點,與文獻報道[8]相近。因此CT、MRI檢查對于SFT具有一定的診斷價值。
綜上所述,膀胱SFT影像定性診斷較困難,當CT檢查發現孤立性混雜密度軟組織腫塊,增強掃描呈地圖樣不均勻樣強化;MRI檢查T2WI呈混雜信號,增強掃描動脈期不均勻強化,靜脈期及延遲期呈持續性強化、延遲強化時,應考慮到SFT的可能。總之,膀胱SFT臨床少見,其確診仍有賴于病理組織學及免疫組織化學檢查,但該腫瘤具有相對典型的影像學特征。
[References]
[1]Klemperer P, Rabin CB. Primary neoplasms of the pleura: a report of five cases. Am J Ind Med, 1992, 22(1): 1-31.
[2]Poyraz A, Kilic D, Hatipoglu A, et al. Pedunculated solitary fibrous tumours arising from the pleura. Monaldi archives for chest disease, 2016, 65(3): 165-168.
[3]Chen Y, Zhu S, Liu GX, et al. One case report of solitary fibrous tumor of bladder and literature review. Journal of Clinical Urology, 2014, 29(5): 405-407.陳崯, 祝帥, 劉光香, 等. 膀胱孤立性纖維瘤1例報告并文獻復習. 臨床泌尿外科雜志, 2014, 29(5): 405-407.
[4]Yue ZY, Dong YD, Hu YY, et al. One case report of solitary fibrous tumor of bladder. Chin J Diagn Pathol, 2016, 23(4): 314-315.岳振營, 董艷光, 胡營營, 等. 膀胱孤立性纖維性腫瘤1例. 診斷病理學雜志, 2016, 23(4): 314-315.
[5]Ruan HJ, Huang AH, Cheng S, et al. Clinicopathologic features of solitary fibrous tumor in urogenital system. Chin J Pathol, 2016, 45(4): 248-251.阮華娟, 黃愛華, 成晟, 等. 泌尿生殖系統孤立性纖維性腫瘤的臨床病理學分析. 中華病理學雜志, 2016, 45(4): 248-251.
[6]Pata F, Orsini V, Lucisano AM, et al. Solitary fibrous tumor of the pelvis: an uncommon soft-tissue tumor. Ann Ital Chir, 2010, 81(6): 457-460.
[7]Liu H, Wang YT, Bai YH, et al. The CT, MRI features and pathological basis of solitary fibrous tumor of the pleural. J Clin Radiol, 2014, 33(6): 863-867.劉衡, 王永濤, 柏永華, 等. 胸膜外孤立性纖維瘤的CT、MRI表現及其病理基礎. 臨床放射學雜志, 2014, 33(6): 863-867.
[8]Chong S, Kim TS, Cho EY, et al. Benign localized fibrous tumour of the pleura: CT features with histopathological correlations. Clinical radiology, 2006, 61(10): 875-882.
[9]Ginat DT, Bokhari A, Bhatt S, et al. Imaging features of solitary fibrous tumors. American Journal of Roentgenology, 2011, 196(3): 487-495.
[10]Kakihara D, Yoshimitsu K, Eto M, et al. MRI of retroperitoneal solitary fibrous tumor in the suprarenal region. American Journal of Roentgenology, 2007, 188(6): 512-514.
Solitary fibrous tumor of bladder: a report of one case: imaging and patholog
Solitary fibrous tumors; Magnetic resonance imaging; Diffusion weighted imaging; Pathology
1.山西醫科大學醫學影像學系,太原 030001
2.山西醫科大學第一醫院影像科,太原 030001
1Department of Medical Imaging, Shanxi Medical University, Taiyuan 030001, China
2Department of Radiology, First Clinical Medical College, Shanxi Medical University, Taiyuan 030001, China
張輝,E-mail:zhanghui_mr@163.com
2016-09-23接受日期:2016-10-31
R445.2;R738.6
B
10.12015/issn.1674-8034.2017.02.013
*Correspondence to: Zhang H, E-mail: zhanghui_mr@163.com
Received 23 Sep 2016, Accepted 31 Oct 2016