腦白質疏松癥對急性缺血性卒中患者影響的Meta分析
付敏郡,胡 郎,趙亞亞,蔣珍秀,劉 寧
卒中是目前世界上第三大死亡原因,好發于中老年人,具有發病率高、病死率高、致殘率高等特點。急性缺血性卒中(AIS)是卒中的主要類型,會危及患者的生命安全,影響患者的生活質量。腦白質疏松癥(LA)又稱腦白質高信號,是指分布于腦室周圍、大腦皮質下白質及半卵圓中心的彌漫性病灶或散在病灶[1]。研究表明,LA是缺血性卒中、腦出血及癡呆的獨立危險因素[2]。目前,LA對AIS患者影響的研究報道較多,但尚存在較大爭議[3]。本研究采用Meta分析方法評估LA對AIS患者的影響,旨在為臨床診療提供參考。
1 資料與方法
1.1 文獻納入與排除標準
1.1.1 文獻納入標準 (1)研究類型:病例對照研究。(2)研究對象:符合《各類腦血管疾病診斷要點》[4]中的AIS診斷標準,經顱腦CT或MRI檢查確診;發病時間≤1周;性別、年齡不限。(3)暴露因素:經顱腦CT或MRI檢查證實存在LA,有明確的LA嚴重程度分級方法。(4)結局指標:改良Rankin量表(mRS)評分、Barthel指數(BI)評分、顱內出血轉化發生率、癥狀性顱內出血[5]發生率、病死率、卒中復發率及血管再通率。
1.1.2 文獻排除標準 (1)重復文獻;(2)文獻質量較差或存在數據雷同等無法利用的文獻;(3)原始數據不完整的文獻;(4)綜述;(5)基礎研究。
1.2 檢 索 策 略 計 算 機 檢 索 PubMed、EMBase、Web of Science(WOS)、The Cochrane Library、萬方數據知識服務平臺、中國生物醫學文獻數據庫(CBM)和中國知網(CNKI)等,檢索時間為建庫至2017-11-30。中文檢索詞為“腦白質疏松癥、腦白質高信號、腦白質損傷、腦小血管病、急性缺血性腦卒中、急性腦梗死”;英文檢索詞為“leukoaraiosis、white matter hyperintensities、cerebral small vascular diseases、white matter lesions、acute ischemic stroke”。
1.3 數據提取 由2位研究人員根據文獻納入與排除標準獨立篩選文獻、提取信息并進行方法學質量評價,如遇分歧則討論解決或交由第三方裁定。依據PICO原則(P:研究對象;I:干預措施;C:對照;O:結局指標)設計信息提取表,提取內容包括文獻的基本信息(第一作者、發表年份)、受試人群基本特征(例數、中位年齡)、干預措施、結局指標。
1.4 文獻質量評價 采用紐卡斯爾-渥太華量表(NOS)[6]進行文獻質量評價,從對象選擇、可比性、結局和暴露3方面進行評價,滿分9分,NOS評分5~9分為文獻質量較高。
1.5 統計學方法 采用RevMan 5.3軟件進行Meta分析,計數資料采用OR及其95%CI進行分析,計量資料采用MD及其95%CI進行分析。各文獻間統計學異質性分析采用χ2檢驗,I2>50%且P<0.1表明各文獻間有統計學異質性,采用隨機效應模型進行Meta分析;I2≤50%且P≥0.1表明各文獻間無統計學異質性,采用固定效應模型進行Meta分析。繪制倒漏斗圖以分析發表偏倚。以P<0.05為差異有統計學意義。
2 結果
2.1 檢索結果及納入文獻質量評價 共檢索相關文獻988篇,排除重復文獻311篇,閱讀文題及摘要后排除612篇文獻,閱讀全文后排除36篇文獻,最終納入29篇文獻[7-35],其中英文文獻28篇,中文文獻1篇,包括15 883例患者,NOS評分均≥6分,文獻質量較高,詳見表1。文獻篩選流程見圖1。
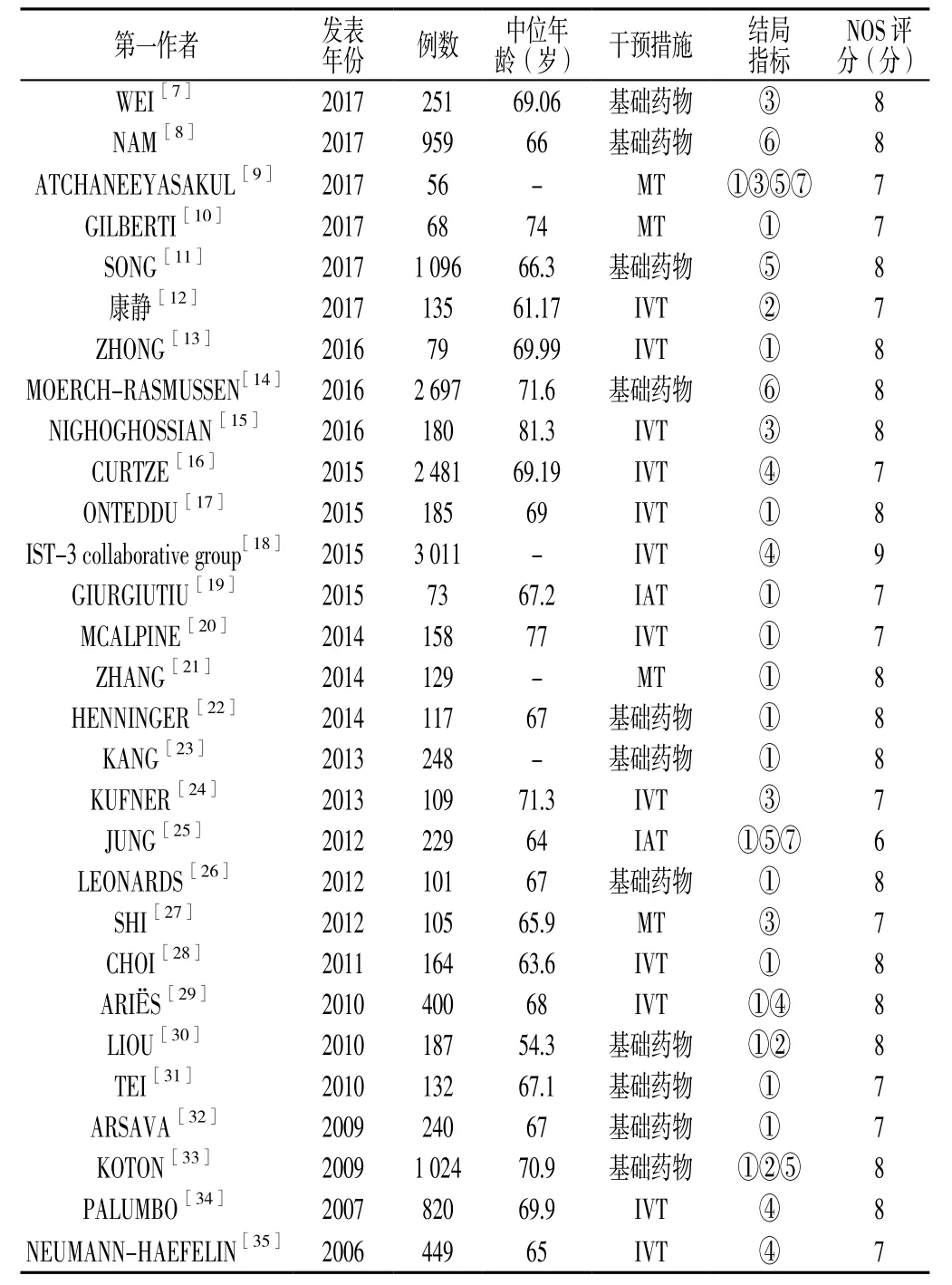
表1 納入文獻的基本特征及質量評價Table 1 Basic characteristics and quality evaluation of the involved literatures
2.2 Meta分析結果
2.2.1 mRS 評 分 17 篇 文 獻[9-10,13,17,19-23,25-26,28-33]報道了mRS評分,各文獻間有統計學異質性(P<0.000 01,I2=81%),采用隨機效應模型進行Meta分析;結果顯示,有LA組患者mRS評分高于無LA組,差異有統計學意義〔MD=1.71,95%CI(1.29,2.27),P=0.000 2,見圖 2〕。
2.2.2 BI評分 3 篇文獻[12,30,33]報道了 BI評分,各文獻間無統計學異質性(P=0.47,I2=0%),采用固定效應模型進行Meta分析;結果顯示,有LA組患者BI評分低于無LA組,差異有統計學意義〔MD=2.51,95%CI(1.62,3.88),P<0.000 1,見圖 3〕。
2.2.3 顱內出血轉化發生率 5 篇文獻[7,9,15,24,27]報道了顱內出血轉化發生率,各文獻間無統計學異質性(P=0.19,I2=34%),采用固定效應模型進行Meta分析;結果顯示,有LA組患者顱內出血轉化發生率高于無LA組,差異有統計學意義〔OR=1.34,95%CI(1.15,1.58),P=0.000 3,見圖 4〕。
2.2.4 癥狀性顱內出血發生率 5 篇文獻[16,18,29,34-35]報道了癥狀性顱內出血發生率,各文獻間無統計學異質性(P=0.13,I2=43%),采用固定效應模型進行Meta分析;結果顯示,有LA組患者癥狀性顱內出血發生率高于無LA組,差異有統計學意義〔OR=1.69,95%CI(1.31,2.19),P<0.000 1,見圖 5〕。
2.2.5 病死率 4 篇文獻[9,11,25,33]報道了病死率,各文獻間有統計學異質性(P=0.004,I2=77%),采用隨機效應模型進行Meta分析;結果顯示,兩組患者病死率比較,差異無統計學意義〔OR=1.11,95%CI(0.66,1.85),P=0.69,見圖 6〕。
2.2.6 卒中復發率 2 篇文獻[8,14]報道了卒中復發率,各文獻間無統計學異質性(P=0.41,I2=0%),采用固定效應模型進行Meta分析;結果顯示,有LA組患者卒中復發率高于無LA 組,差異有統計學意義〔OR=1.55,95%CI(1.26,1.91),P<0.000 1,見圖 7〕。
2.2.7 血管再通率 2 篇文獻[9,25]報道了血管再通率,各文獻間無統計學異質性(P=0.39,I2=0%),采用固定效應模型進行Meta分析;兩組患者血管再通率比較,差異無統計學意義〔OR=1.04,95%CI(0.74,1.45),P=0.83,見圖 8〕。
2.3 發表偏倚 繪制倒漏斗圖分析報道mRS評分文獻的發表偏倚,結果顯示,散點分布不對稱,多數散點位于中下部,提示報道mRS評分文獻的發表偏倚可能較大(見圖9)。因報道其他結局指標的文獻數量較少,倒漏斗圖分析誤差較大,故未繪制倒漏斗圖。
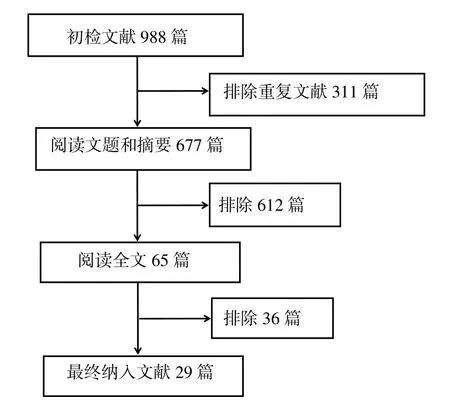
圖1 文獻篩選流程Figure 1 Flow chart for literature screening
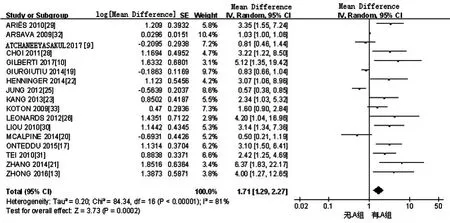
圖2 無/有LA組患者mRS評分比較的森林圖Figure 2 Forest plot for comparison of mRS score in patients with leukoaraiosis or not
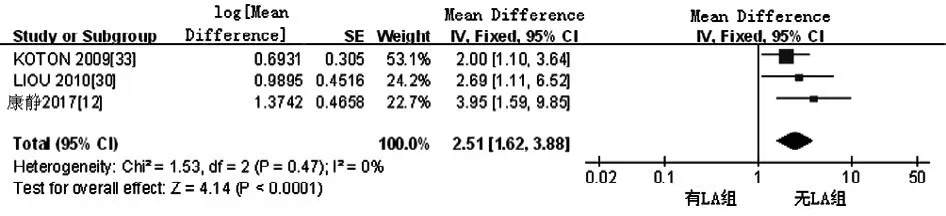
圖3 無/有LA組患者BI評分比較的森林圖Figure 3 Forest plot for comparison of BI score between without LA group and LA group
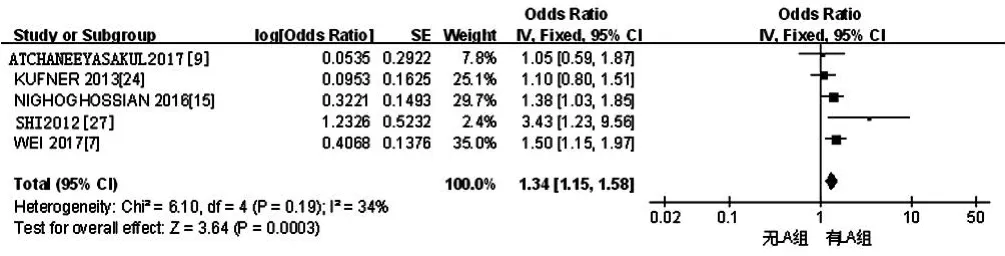
圖4 無/有LA組患者顱內出血轉化發生率比較的森林圖Figure 4 Forest plot for comparison of incidence of intracranial hemorrhagic transformation in patients with leukoaraiosis or not
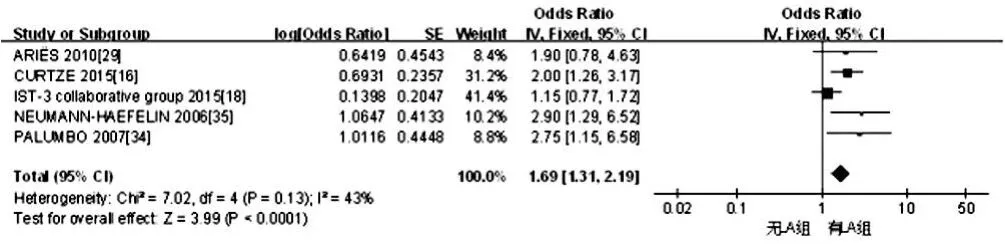
圖5 無/有LA組患者癥狀性顱內出血發生率比較的森林圖Figure 5 Forest plot for comparison of incidence of symptomatic intracerebral hemorrhage in patients with leukoaraiosis or not
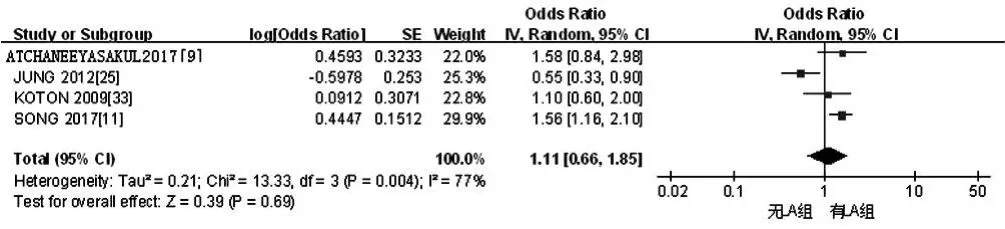
圖6 無/有LA組患者病死率比較的森林圖Figure 6 Forest plot for comparison of fatality rate in patients with leukoaraiosis or not
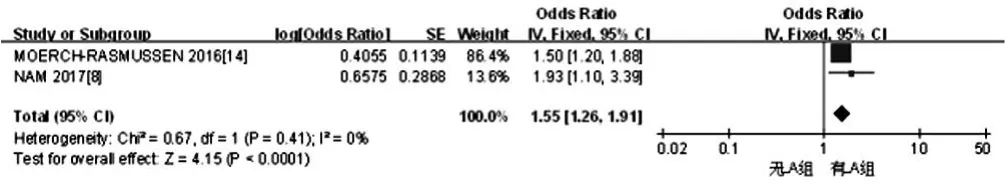
圖7 無/有LA組患者卒中復發率比較的森林圖Figure 7 Forest plot for comparison of recurrent rate of stroke in patients with leukoaraiosis or not
3 討論
LA是由Hachinski在1987年首次提出的一個影像學診斷術語,用來描述腦皮質下白質CT密度灶,多見于老年人[36]。LA在T2加權像與液體衰減反轉恢復(FLAIR)序列表現為白質高信號,病變部位小血管管壁出現增厚、透明樣變,導致血管曲折、狹窄,造成管腔內血流量減少,不利于卒中患者側支循環的建立[2]。LIN等[37]研究結果顯示,非癡呆人群LA發生率約為73.0%,40~80歲住院患者LA發生率約為58.3%,>80歲住院患者LA發生率約為82.7%。研究表明,LA與癡呆、殘疾、卒中等關系密切[38]。多項研究表明,LA是腦小血管相關性疾病,主要病理表現為不同程度的髓鞘和軸突脫失、小動脈硬化和輕微的神經膠質細胞增生等[39-40]。
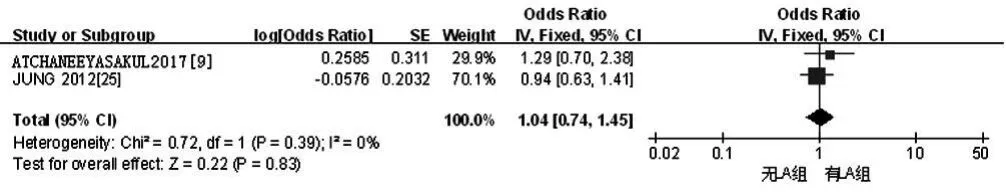
圖8 無/有LA組患者血管再通率比較的森林圖Figure 8 Forest plot for comparison of vascular recanalization rate in patients with leukoaraiosis or not
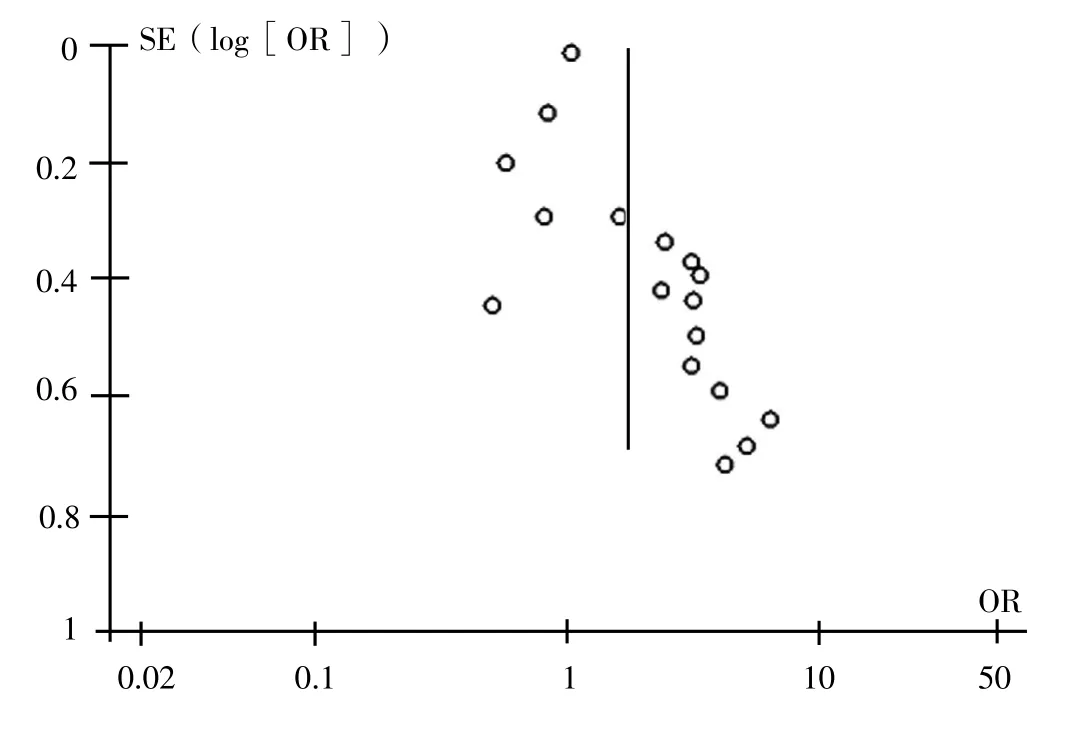
圖9 報道mRS評分文獻發表偏倚的倒漏斗圖Figure 9 Inverted funnel plot for publication bias of involved literatures reported mRS score
AIS合并LA患者上皮細胞、星形膠質細胞損傷及氧化應激反應會破壞血管內皮細胞完整性,使血-腦脊液屏障通透性增加,同時LA區域腦微循環長期損傷會誘發缺血組織出血轉化[41-42]。研究表明,卒中后梗死灶面積擴大會影響患者預后,而LA是梗死灶面積擴大的獨立危險因素[3]。RYU等[43]通過對5 000例卒中患者進行研究發現,卒中合并LA患者神經功能損傷較重,且治療3個月后患者神經功能改善效果較差。SENDA等[44]研究表明,AIS合并LA患者神經功能損傷較重、認知功能較差,會嚴重影響患者的生活質量。多項研究表明,有LA的卒中患者溶栓治療后出血轉化發生率高于無LA的卒中患者[45-47]。KUMRAL等[48]研究表明,AIS合并LA患者卒中復發率高于未合并LA者。
本Meta分析結果顯示,有LA組患者mRS評分高于無LA組,提示AIS合并LA患者神經功能損傷較重;有LA組患者BI評分低于無LA組,提示AIS合并LA患者日常生活活動能力較差;有LA組患者顱內出血轉化發生率、癥狀性顱內出血發生率、卒中復發率高于無LA組,與既往研究結果一致[8],提示AIS合并LA患者顱內出血轉化發生率、癥狀性顱內出血發生率、卒中復發率較高;兩組患者病死率、血管再通率間無差異,與既往研究結果一致[49]。
本Meta分析的局限性:(1)納入文獻均為病例對照研究,且多為單中心研究,可能降低結果的可信性;(2)納入文獻均為已發表文獻,未檢索相關會議論文等,可能對研究結果產生一定影響。
參考文獻
[1]WARDLAW J M,SMITH C,DICHGANS M.Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging[J].Lancet Neurol,2013,12(5):483-497.DOI:10.1016/S1474-4422(13)70060-7.
[2]ETHERTON M R,WU O,ROST N S.Recent Advances in Leukoaraiosis: White Matter Structural Integrity and Functional Outcomes after Acute Ischemic Stroke[J].Curr Cardiol Rep,2016,18(12):123.DOI:10.1007/s11886-016-0803-0.
[3]FIERINI F,POGGESI A,PANTONI L.Leukoaraiosis as an outcome predictor in the acute and subacute phases of stroke[J].Expert Rev Neurother,2017,17(10):963-975.DOI:10.1080/14737175.2017.1371013.
[4]各類腦血管疾病診斷要點[J].中華神經科雜志,1996,29(6):60-61.
[5]LARRUE V,VON KUMMER R R,MüLLER A,et al.Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II)[J].Stroke,2001,32(2):438-441.
[6]WELLS G A,SHEA B,O'CONNELL D,et al.The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis[J].The Ottawa Hospital Research Institute,2013,3:1-4.
[7]WEI C C,ZHANG S T,WANG Y H,et al.Association between leukoaraiosis and hemorrhagic transformation after cardioembolic stroke due to atrial fibrillation and/or rheumatic heart disease[J].J Neurol Sci,2017,378:94-99.DOI:10.1016/j.jns.2017.05.001.
[8]NAM K W,KWON H M,LIM J S,et al.Clinical relevance of abnormal neuroimaging findings and long-term risk of stroke recurrence[J].Eur J Neurol,2017,24(11):1348-1354.DOI:10.1111/ene.13391.
[9]ATCHANEEYASAKUL K,LESLIE-MAZWI T,DONAHUE K,et al.White Matter Hyperintensity Volume and Outcome of Mechanical Thrombectomy With Stentriever in Acute Ischemic Stroke[J].Stroke,2017,48(10):2892-2894.DOI:10.1161/STROKEAHA.117.018653.
[10]GILBERTI N,GAMBA M,PREMI E,et al.Leukoaraiosis is a predictor of futile recanalization in acute ischemic stroke[J].J Neurol,2017,264(3):448-452.DOI:10.1007/s00415-016-8366-y.
[11]SONG T J,KIM J,SONG D,et al.Total Cerebral Small-Vessel Disease Score is Associated with Mortality during Follow-Up after Acute Ischemic Stroke[J].J Clin Neurol,2017,13(2):187-195.DOI:10.3988/jcn.2017.13.2.187.
[12]康靜,李晨曦,范百亞,等.急性腦梗死患者腦白質疏松程度與靜脈溶栓治療后日常生活能力恢復的關系[J].血栓與止血學,2017,23(4):591-594,598.
[13]ZHONG G,YAN S,ZHANG S,et al.Association between Leukoaraiosis and Poor Outcome is not due to Reperfusion Inefficiency after Intravenous Thrombolysis[J].Transl Stroke Res,2016,7(5):439-445.DOI:10.1007/s12975-016-0473-7.
[14]MOERCH-RASMUSSEN A,NACU A,WAJE-ANDREASSEN U,et al.Recurrent ischemic stroke is associated with the burden of risk factors[J].Acta Neurol Scand,2016,133(4):289-294.DOI:10.1111/ane.12457.
[15]NIGHOGHOSSIAN N,ABBAS F,CHO T H,et al.Impact of leukoaraiosis on parenchymal hemorrhage in elderly patients treated with thrombolysis[J].Neuroradiology,2016,58(10):961-967.DOI:10.1007/s00234-016-1725-7.
[16]CURTZE S,HAAPANIEMI E,MELKAS S,et al.White Matter Lesions Double the Risk of Post-Thrombolytic Intracerebral Hemorrhage[J].Stroke,2015,46(8):2149-2155.DOI:10.1161/STROKEAHA.115.009318.
[17]ONTEDDU S R,GODDEAU R P Jr,MINAEIAN A,et al.Clinical impact of leukoaraiosis burden and chronological age on neurological deficit recovery and 90-day outcome after minor ischemic stroke[J].J Neurol Sci,2015,359(1/2):418-423.DOI:10.1016/j.jns.2015.10.005.
[18]IST-3 collaborative group.Association between brain imaging signs,early and late outcomes,and response to intravenous alteplase after acute ischaemic stroke in the third International Stroke Trial (IST-3): secondary analysis of a randomised controlled trial[J].Lancet Neurol,2015,14(5):485-496.DOI:10.1016/S1474-4422(15)00012-5.
[19]GIURGIUTIU D V,YOO A J,FITZPATRICK K,et al.Severity of leukoaraiosis,leptomeningeal collaterals,and clinical outcomes after intra-arterial therapy in patients with acute ischemic stroke[J].J Neurointerv Surg,2015,7(5):326-330.DOI:10.1136/neurintsurg-2013-011083.
[20]MCALPINE H,CHURILOV L,MITCHELL P,et al.Leukoaraiosis and early neurological recovery after intravenous thrombolysis[J].J Stroke Cerebrovasc Dis,2014,23(9):2431-2436.DOI:10.1016/j.jstrokecerebrovasdis.2014.05.012.
[21]ZHANG J,PURI A S,KHAN M A,et al.Leukoaraiosis predicts a poor 90-day outcome after endovascular stroke therapy[J].AJNR Am J Neuroradiol,2014,35(11):2070-2075.DOI:10.3174/ajnr.A4029.
[22]HENNINGER N,KHAN M A,ZHANG J,et al.Leukoaraiosis predicts cortical infarct volume after distal middle cerebral artery occlusion[J].Stroke,2014,45(3):689-695.DOI:10.1161/STROKEAHA.113.002855.
[23]KANG H J,STEWART R,PARK M S,et al.White matter hyperintensities and functional outcomes at 2 weeks and 1 year after stroke[J].Cerebrovasc Dis,2013,35(2):138-145.DOI:10.1159/000346604.
[24]KUFNER A,GALINOVIC I,BRUNECKER P,et al.Early infarct FLAIR hyperintensity is associated with increased hemorrhagic transformation after thrombolysis[J].Eur J Neurol,2013,20(2):281-285.DOI:10.1111/j.1468-1331.2012.03841.x.
[25]JUNG S,MONO M L,FINDLING O,et al.White matter lesions and intra-arterial thrombolysis[J].J Neurol,2012,259(7):1331-1336.DOI:10.1007/s00415-011-6352-y.
[26]LEONARDS C O,IPSEN N,MALZAHN U,et al.White matter lesion severity in mild acute ischemic stroke patients and functional outcome after 1 year[J].Stroke,2012,43(11):3046-3051.DOI:10.1161/STROKEAHA.111.646554.
[27]SHI Z S,LOH Y,LIEBESKIND D S,et al.Leukoaraiosis predicts parenchymal hematoma after mechanical thrombectomy in acute ischemic stroke[J].Stroke,2012,43(7):1806-1811.DOI:10.1161/STROKEAHA.111.649152.
[28]CHOI J H,BAE H J,CHA J K.Leukoaraiosis on magnetic resonance imaging is related to long-term poor functional outcome after thrombolysis in acute ischemic stroke[J].J Korean Neurosurg Soc,2011,50(2):75-80.DOI:10.3340/jkns.2011.50.2.75.
[29]ARI?S M J,UYTTENBOOGAART M,VROOMEN P C,et al.tPA treatment for acute ischaemic stroke in patients with leukoaraiosis[J].Eur J Neurol,2010,17(6):866-870.DOI:10.1111/j.1468-1331.2010.02963.x.
[30]LIOU L M,CHEN C F,GUO Y C,et al.Cerebral white matter hyperintensities predict functional stroke outcome[J].Cerebrovasc Dis,2010,29(1):22-27.DOI:10.1159/000255970.
[31]TEI H,UCHIYAMA S,USUI T,et al.Posterior circulation ASPECTS on diffusion-weighted MRI can be a powerful marker for predicting functional outcome[J].J Neurol,2010,257(5):767-773.DOI:10.1007/s00415-009-5406-x.
[32]ARSAVA E M,RAHMAN R,ROSAND J,et al.Severity of leukoaraiosis correlates with clinical outcome after ischemic stroke[J].Neurology,2009,72(16):1403-1410.DOI:10.1212/WNL.0b013e3181a18823.
[33]KOTON S,SCHWAMMENTHAL Y,MERZELIAK O,et al.Cerebral leukoaraiosis in patients with stroke or TIA: clinical correlates and 1-year outcome[J].Eur J Neurol,2009,16(2):218-225.DOI:10.1111/j.1468-1331.2008.02389.x.
[34]PALUMBO V,BOULANGER J M,HILL M D,et al.Leukoaraiosis and intracerebral hemorrhage after thrombolysis in acute stroke[J].Neurology,2007,68(13):1020-1024.DOI:10.1212/01.wnl.0000257817.29883.48.
[35]NEUMANN-HAEFELIN T,HOELIG S,BERKEFELD J,et al.Leukoaraiosis is a risk factor for symptomatic intracerebral hemorrhage after thrombolysis for acute stroke[J].Stroke,2006,37(10):2463-2466.DOI:10.1161/01.STR.0000239321.53203.ea.
[36]HACHINSKI V C,POTTER P,MERSKEY H.Leuko-araiosis[J].Arch Neurol,1987,44(1):21-23.
[37]LIN Q,HUANG W Q,MA Q L,et al.Incidence and risk factors of leukoaraiosis from 4683 hospitalized patients: A cross-sectional study[J].Medicine (Baltimore),2017,96(39):e7682.DOI:10.1097/MD.0000000000007682.
[38]SIBOLT G,CURTZE S,MELKAS S,et al.White matter lesions are associated with hospital admissions because of hip-fractures and trauma after ischemic stroke[J].Stroke,2014,45(10):2948-2951.DOI:10.1161/STROKEAHA.114.006116.
[39]PANTONI L.Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges[J].Lancet Neurol,2010,9(7):689-701.DOI:10.1016/S1474-4422(10)70104-6.
[40]PRINS N D,SCHELTENS P.White matter hyperintensities,cognitive impairment and dementia: an update[J].Nat Rev Neurol,2015,11(3):157-165.DOI:10.1038/nrneurol.2015.10.
[41]DE SILVA T M,MILLER A A.Cerebral Small Vessel Disease:Targeting Oxidative Stress as a Novel Therapeutic Strategy?[J].Front Pharmacol,2016,7:61.DOI:10.3389/fphar.2016.00061.eCollection 2016.
[42]LLOMBART V,DOMINGUEZ C,BUSTAMANTE A,et al.Fluorescent molecular peroxidation products: a prognostic biomarker of early neurologic deterioration after thrombolysis[J].Stroke,2014,45(2):432-437.DOI:10.1161/STROKEAHA.113.003431.
[43]RYU W S,WOO S H,SCHELLINGERHOUT D,et al.Stroke outcomes are worse with larger leukoaraiosis volumes[J].Brain,2017,140(1):158-170.DOI:10.1093/brain/aww259.
[44]SENDA J,ITO K,KOTAKE T,et al.Association of Leukoaraiosis With Convalescent Rehabilitation Outcome in Patients With Ischemic Stroke[J].Stroke,2016,47(1):160-166.DOI:10.1161/STROKEAHA.115.010682.
[45]LIN Q,LI Z,WEI R,et al.Increased Risk of Post-Thrombolysis Intracranial Hemorrhage in Acute Ischemic Stroke Patients with Leukoaraiosis: A Meta-Analysis[J].PLoS One,2016,11(4):e0153486.DOI:10.1371/journal.pone.0153486.
[46]CHARIDIMOU A,PASI M,FIORELLI M,et al.Leukoaraiosis,Cerebral Hemorrhage,and Outcome After Intravenous Thrombolysis for Acute Ischemic Stroke: A Meta-Analysis (v1)[J].Stroke,2016,47(9):2364-2372.DOI:10.1161/STROKEAHA.116.014096.
[47]KONGBUNKIAT K,WILSON D,KASEMSAP N,et al.Leukoaraiosis,intracerebral hemorrhage,and functional outcome after acute stroke thrombolysis[J].Neurology,2017,88(7):638-645.DOI:10.1212/WNL.0000000000003605.
[48]KUMRAL E,GüLLüO L U H,ALAKBAROVA N,et al.Association of leukoaraiosis with stroke recurrence within 5 years after initial stroke[J].J Stroke Cerebrovasc Dis,2015,24(3):573-582.DOI:10.1016/j.jstrokecerebrovasdis.2014.10.002.
[49]INZITARI D,PRACUCCI G,POGGESI A,et al.Changes in white matter as determinant of global functional decline in older independent outpatients: three year follow-up of LADIS(leukoaraiosis and disability) study cohort[J].BMJ,2009,339:b2477.DOI:10.1136/bmj.b2477.