認知行為康復干預對小細胞肺癌化療患者胃腸道反應、睡眠質量及生活質量的影響
馮莉梨 楊希 徐慧芳
[摘要] 目的 探討認知行為康復干預對小細胞肺癌(SCLC)化療患者胃腸道反應、睡眠質量及生活質量的影響。方法 選取2016年1月~2018年12月在我院化療SCLC患者94例,采用拋硬幣法分為干預組與對照組,每組47例。兩組均予以EP方案(足葉乙苷+順鉑)進行化療。對照組予以健康教育、心理干預及飲食干預等常規康復措施,觀察組在對照組基礎上予以認知行為康復干預。兩組均干預4周。觀察兩組干預期間胃腸道反應發生率,并比較干預前與干預4周后睡眠質量及生活質量變化。 結果 干預4周期間,干預組胃腸道反應發生率(40.43%)明顯低于對照組(61.70%),差異有統計學意義(χ2=4.262,P<0.05)。干預4周后,兩組PSQI評分均較干預前不同程度顯著下降(P<0.05或P<0.01);且干預組下降幅度較對照組更顯著(P<0.05);同時兩組軀體、心理、社會和物質功能等生活質量各項評分較干預前明顯上升(P<0.05或P<0.01),且干預組上升幅度較對照組更明顯(P<0.05)。 結論 認知行為康復干預用于SCLC化療患者不僅可緩解或減輕化療期間的胃腸道反應,而且可改善其睡眠質量,提高患者的生活質量,改善其預后。
[關鍵詞] 小細胞肺癌;化療;認知行為康復干預;胃腸道反應;睡眠質量;生活質量
[中圖分類號] R473.73? ? ? ? ? [文獻標識碼] B? ? ? ? ? [文章編號] 1673-9701(2020)22-0092-04
Effect of cognitive behavioral rehabilitation intervention on gastrointestinal reactions, sleep quality and quality of life in patients with small cell lung cancer undergoing chemotherapy
FENG Lili1? ?YANG Xi1? ?XU Huifang2
1.Health Management Center, Taizhou Central Hospital in Zhejiang Province (the Affiliated Hospital of Taizhou University), Taizhou? ?318000, China; 2.Department of Thoracic Surgery, Taizhou Central Hospital in Zhejiang Province (the Affiliated Hospital of Taizhou University), Taizhou? ?318000, China
[Abstract] Objective To investigate the effect of cognitive behavioral rehabilitation intervention on gastrointestinal reactions, sleep quality and quality of life in patients with small cell lung cancer(SCLC) undergoing chemotherapy. Methods A total of 94 patients with SCLC in our hospital who underwent chemotherapy from January 2016 to December 2018 were selected. They were divided into intervention group(n=47) and control group(n=47) by coin-throwing methods. Both groups were treated with the EP regimen(Etoposide+Cisplatin) for chemotherapy. In the control group, routine rehabilitation measures such as health education, psychological intervention and dietary intervention were given. The observation group was given cognitive behavioral rehabilitation intervention based on the treatment of the control group. Both groups were intervened for 4 weeks. The incidence of gastrointestinal reactions during interventions between two groups was observed, and the changes in sleep quality and quality of life were compared before and 4 weeks after intervention. Results During the 4 weeks of intervention, the incidence of gastrointestinal reactions in the intervention group(40.43%) was significantly lower than that(61.70%) in the control group(χ2=4.262, P<0.05). After 4 weeks of intervention, the PSQI scores of the two groups were significantly lower than those before intervention(P<0.05 or P<0.01). And the varying decrease of the intervention group was more significant than that of the control group(P<0.05). At the same time, the scores of quality of life including physical, psychological, social and substances function were significantly higher than those before intervention(P<0.05 or P<0.01). And the increase of the intervention group was more significant than that of the control group(P<0.05). Conclusion Cognitive behavioral rehabilitation intervention for SCLC patients can not only alleviate or reduce the gastrointestinal reactions during chemotherapy, but also improve their sleep quality, improve their quality of life and improve their prognosis.
[Key words] Small cell lung cancer; Chemotherapy; Cognitive behavioral rehabilitation intervention; Gastrointestinal reactions; Sleep quality; Quality of life
肺癌是我國發病率最高的惡性腫瘤之一,其中小細胞肺癌(Small cell lung cancer,SCLC)較常見,惡性程度極高,易發生轉移,預后相對較差[1,2]。化療是治療SCLC患者常用的方法,化療在殺滅癌細胞病灶同時也損傷了正常細胞及組織,易發生胃腸道反應和睡眠障礙,降低患者生活質量[3,4]。以往多采用常規健康教育、飲食干預和心理干預等方法干預治療SCLC化療后胃腸道反應和睡眠障礙,但臨床效果欠佳[5,6]。認知行為康復干預是一種通過改變患者對于事物的認知,建立合理認知概念的干預方法,但用于SCLC化療后胃腸道反應和睡眠障礙目前國內報道較少[7,8]。本研究分析認知行為康復干預對SCLC化療患者胃腸道反應、睡眠障礙及生活質量的影響,現報道如下。
1 資料與方法
1.1 一般資料
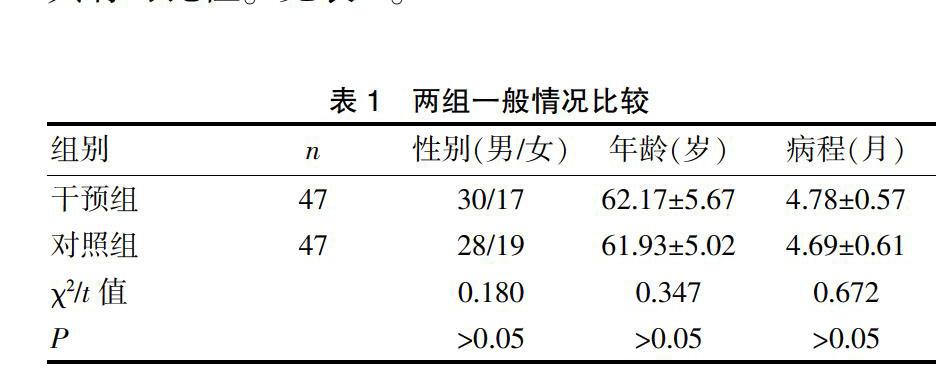
選取2016年1月~2018年12月在我院化療的SCLC患者共94例。納入標準[9]:(1)符合《中國原發性肺癌診療規范(2015年版)》中的診斷標準[10],且經病理或組織學證實;(2)預期生存時間>3個月。排除標準[11]:(1)伴有其他部位的腫瘤;(2)重要臟器功能障礙。采用拋硬幣法分為干預組與對照組各47例。兩組性別、年齡及病程等比較差異無統計學意義(P>0.05),具有可比性。見表1。
1.2 方法
兩組患者均予以EP方案(足葉乙苷+順鉑)進行化療。對照組予以健康教育、心理干預及飲食干預等常規康復措施。干預組患者在對照組基礎上予以認知行為康復干預,包括:(1)認知干預:向患者介紹化療期間可能引起的胃腸道反應及應對措施,使患者做好心理準備,提高患者對化療認知度,改變以往的錯誤認知,使患者徹底接受正確的觀念,提高治療的遵醫行為;(2)行為干預:患者于化療前后開展能力所及的適度有氧運動,如步行、太極拳、跳健身舞、騎自行車等,以促進胃腸道蠕動,提高機體免疫功能;向患者講解飲食注意事項,囑患者化療前吃一點餅干或面包等干且溫和的食物;控制三餐前后1 h的飲水量,盡量不飲水或少飲水,化療期間多吃高蛋白質、高維生素易消化的食物,忌餐后立即躺下休息,以免食物反流引起惡心、嘔吐。兩組均干預4周。觀察兩組干預期間胃腸道反應的發生率,并比較干預前與干預4周后睡眠質量和生活質量變化。
1.3 觀察指標
1.3.1 胃腸道反應? 包括惡心、嘔吐、腹瀉、便秘和食欲減退等胃腸道反應。
1.3.2 睡眠質量評估[10]? 采用匹茲堡睡眠質量指數量表(Pittsburgh sleep quality index,PSQI)進行評估,內容包括睡眠質量、入睡時間、睡眠時間、睡眠效率、睡眠障礙、催眠藥物及日間功能障礙7項,每項3分,總分21分,分數越高提示患者睡眠質量越差。
1.3.3 生活質量評估[12]? 采用生活質量GQOL-74問卷評估患者生活質量,內容包括物質功能、心理功能、軀體功能和社會功能共4項,每項評分為100分,分數越高提示患者生活質量越高。
1.4 統計學處理
采用SPSS20.0統計學軟件進行分析,計量資料以均數±標準差(x±s)表示,采用t檢驗,計數資料以[n(%)]表示,采用χ2檢驗,P<0.05為差異有統計學意義。
2 結果
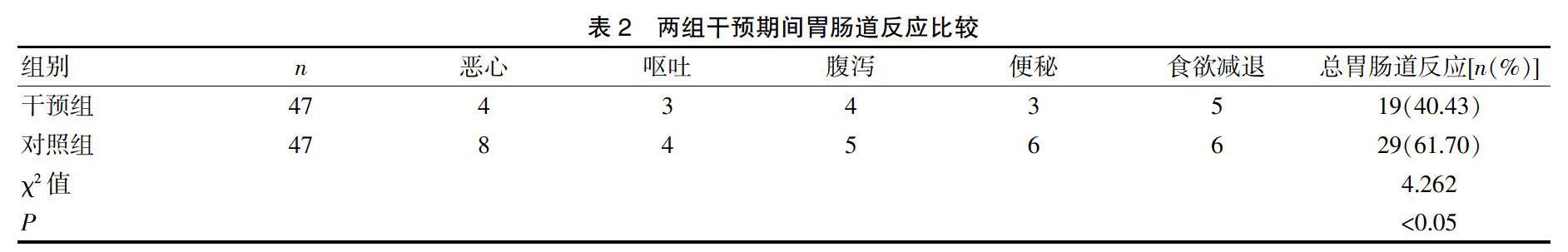
2.1 兩組干預期間胃腸道反應比較
干預4周期間,干預組胃腸道反應發生率(40.43%)明顯低于對照組(61.70%),差異有統計學意義(χ2=4.262,P<0.05)。見表2。
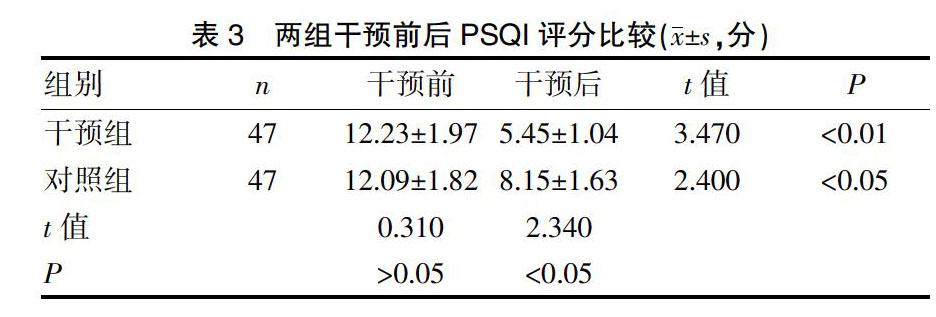
2.2 兩組干預前后PSQI評分比較
干預前,兩組PSQI評分比較差異無統計學意義(P>0.05);干預4周后,兩組PSQI評分均較干預前不同程度顯著下降(P<0.05或P<0.01);且干預組下降幅度較對照組更顯著(P<0.05)。見表3。
2.3 兩組干預前后生活質量評分比較
干預前,兩組軀體、心理、社會和物質功能等生活質量各項評分比較差異無統計學意義(P>0.05);干預4周后,兩組軀體、心理、社會和物質功能等生活質量各項評分較干預前明顯上升(P<0.05或P<0.01),且干預組上升幅度較對照組更明顯(P<0.05)。見表4。
3 討論
近年來由于人口老齡化及逐漸加重的環境污染,肺癌的發病率及病死率呈逐年上升的趨勢且逐漸年輕化[13,14]。SCLC是肺癌中一種惡性程度極高的腫瘤,發病率占肺癌的15%~20%;好發于中老年男性,發病早期就易發生轉移、病情進展迅速,對患者生存安全構成重大威脅[15]。化療是目前SCLC最常用常見的治療手段之一,能有效控制癌細胞的生長,延長其生存期限,但化療藥在殺滅癌細胞的同時,也殺傷正常細胞及組織,所引起的副作用及不良反應仍較突出,影響患者的生活質量[16,17]。SCLC化療期間患者常見不良反應是胃腸道反應和睡眠障礙,其發病率為60%~90%,若長期得不到有效控制治療,不僅會導致患者營養狀況不良和免疫功能下降,還會對患者的生理和心理造成一定的影響,產生焦慮、抑郁等負性情緒,影響患者化療的依從性,使得患者治療無法耐受而中斷治療,嚴重影響化療的效果及延長患者生命的意義。因此,如何采取措施緩解或減輕化療期間的胃腸道反應,改善其睡眠質量,提高患者的生活質量,對SCLC化療患者具有重要的意義[18,19]。
認知行為康復干預是由60年代提出的一種有結構、短程、認知取向的心理干預治療方法,主要是通過改變或影響個體已有的認知和行為思維模式來影響個體的行為水平,改善心理問題的各種主動措施,是目前世界上流行最為廣泛,使用最多的心理治療方法。認知行為康復干預是一種臨床上常用的心理治療干預模式,起源于心理學、行為學和教育學,是基于行為與認知心理學的基本原理結合,側重于個人應對策略的發展,目標是解決來訪者當前問題,改變其不正確的認知、行為和情緒調節的無用模式,從而緩解來訪者痛苦并減輕其相關癥狀[20,21]。以往認知行為康復干預主要應用于糾正學生的學習障礙及精神疾病的干預治療,取得了較好的效果[22,23]。本研究將認知行為康復干預用于SCLC化療患者亦取得了較好的效果,通過認知干預提高患者對疾病的認知及化療認知度,改變以往的不正確認知,使患者徹底接受正確的觀念,建立正確的認知模式,提高治療的遵醫行為,使患者主動接受并積極配合治療,提高化療的效果,減少不良反應,有效緩解或減輕心理緊張,改善睡眠質量[24-26];同時加強化療期間的飲食干預,以緩解或減輕化療期間的胃腸道反應,增強患者營養狀況及免疫功能,增加患者治療疾病的信心,提高患者的生活質量[27,28]。本研究示干預4周期間,干預組胃腸道反應發生率(40.43%)明顯低于對照組(61.70%)。提示認知行為康復干預用于SCLC化療患者可緩解或減輕化療期間的胃腸道反應。同時研究還發現,干預4周后,干預組PSQI評分下降幅度較對照組更明顯,且干預組患者軀體、心理、社會和物質功能等生活質量各項評分上升幅度亦較對照組更明顯。提示認知行為康復干預用于SCLC化療患者可改善其睡眠質量,提高患者生活質量,改善其預后。
總之,認知行為康復干預用于SCLC化療患者不僅可緩解或減輕化療期間胃腸道反應,且可改善其睡眠質量,提高患者生活質量,改善其預后。本研究納入的病例數相對偏少、觀察時間相對偏短,必要時增加納入的病例數及延長觀察時間進行深入研究。
[參考文獻]
[1] Imai H,Shukuya T,Yoshino R,et al. Efficacy and safety of platinum combination chemotherapy re-challenge for relapsed patients with non-small-cell lung cancer after postoperative adjuvant chemotherapy of cisplatin plus vinorelbine[J]. Chemotherapy,2014,59(4):307-313.
[2] Thakur MK,Ruterbusch JJ,Schwartz AG,et al. Risk of second lung cancer in patients with previously treated lung cancer:Analysis of surveillance,epidemiology,and end results(SEER) data[J]. J Thorac Oncol,2018,13(1):46-53.
[3] Calixto- Lima L,de Andrade EM,Gomes AP,et al. Dietetic management in gastrointestinal complications from antimalignant chemotherapy[J]. Nutr Hosp,2012,27(1):65-75.
[4] 盧久琴,馬亮亮,王心悅,等. 肺癌患者化療相關嘔吐前驅癥狀的篩選及其與化療相關嘔吐的關系[J]. 中國腫瘤雜志,2014,36(7):511-515.
[5] Ishikawa A,Ohara G,Nakazawa K,et al. Chemotherapy-in-duced complications in patients with lung cancer:An evaluation by pharmacists[J]. Mol Clin Oncol,2013,10(1):65-68.
[6] 劉桂霞,章新瓊. 化療期肺癌患者應對方式與胃腸道反應的相關性[J]. 廣東醫學,2016,37(5):735-738.
[7] 何圓,劉芳,錢曉濤,等. 認知行為干預晚期肺癌化療患者焦慮、抑郁模式分析[J]. 重慶醫學,2015,44(20):2776-2779.
[8] Sherwood P,Given BA,Given CW,et al. A cognitive behavioral intervention for symptom management in patients with advanced cancer[J]. Oncol Nurs Forum,2005, 32(6):1190-1198.
[9] Mitchell SA,Beck SL,Hood LE,et al. Putting evidence into practice:Evidence-based interventions for fatigue during and following cancer and its treatment[J]. Clin J Oncol Nurs,2007,11(1):99-113.
[10] 支修益,石遠凱,于金明. 中國原發性肺癌診療規范(2015年版)[J]. 中華腫瘤雜志,2015,37(1):67-78.
[11] Roberto HA,Kristopher PC,Pankaj P. Surgical vs percutaneous radiofrequency ablation for hepatocellular carcinoma in dangerous locations[J]. World Journal of Gastroenterology,2011,17(1):123-129.
[12] 黎銀煥,周燕斌,黃琬玲,等. 肺癌患者睡眠與生活質量影響因素的回歸分析[J]. 中華腫瘤防治雜志,2011, 18(23):1874-1877.
[13] Samet JM. Is there more to learn about the epidemiology of lung cancer?[J]. Eur J Epidemiol,2016,31(12):1159-1160.
[14] Hirai F,Seto T,Shimokawa M,et al. Split-dose cisplatin and vinorelbine as adjuvant chemoth erapy for completely resected non-small cell lung cancer[J]. Anticancer Res,2014,34(2):927-931.
[15] Borghaei H,Paz-Ares L,Horn L,et al. Nivolumab versus docetaxel in advanced nonsquamous non-smallcell lung cancer [J]. N Engl J Med,2015,373(17):1627-1639.
[16] Dubey AK,Gupta U,Jain S. Epidemiology of lung cancer and approaches for its prediction:A systematic review and analysis[J]. Chin J Cancer,2016,35(1):71.
[17] Evison M,Edwards T,Balata H,et al. Prevalence of nodal metastases in lymph node stations 8 & 9 in a large UK lung cancer surgical centre without routine pre-operative EUS nodal staging[J]. Lung Cancer,2018,115(2):127-130.
[18] 楊志彥,楚新霞. 化療前后肺癌患者生活質量、焦慮抑郁情緒變化及生活質量影響因素[J]. 中國醫藥導報,2016,13(5):122-125.
[19] Andreyev HJ,Norman AR,Oates J,et al. Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies?[J]. Eur J Cancer,2018,34(4):503-509.
[20] Gupta D,Lis CG,Granick J,et al. Malnutrition was associated with poor quality of life in colorectal cancer:A retrospective analysis[J]. J Clin Epidemiol,2006,59(7):704-709.
[21] Devine E. Meta-analysis of the effect of psychoeducational interventions on pain in adults with cacer[J]. Oncol Nurs Forum,2003,30(1):75-89.
[22] Lee H,Lim Y,Yoo MS,et al. Effects of a nurse-led cognitive-behavior therapy on fatigue and quality of life of patients with breast cancer undergoing radiotherapy:An exploratory study[J]. Cancer Nurs,2011,34(6):E22-30.
[23] Kwekkeboom KL,Abbott-Anderson K,Wanta B. Feasibility of a patient-controlled cognitive-behavioral intervention for pain,fatigue,and sleep disturbance in cancer[J].Oncol Nurs Forum,2010,37(3):E151-E159.
[24] 劉翠芹. 認知行為干預對肺癌化療患者生活質量的影響研究[J]. 吉林醫學,2013,34(29):6170-6171.
[25] 林曉紅,彭婧,李平東,等. 認知行為干預對肺癌哀痛患者焦慮抑郁情緒的影響[J]. 國際醫藥衛生導報,2015, 21(18):2773-2775.
[26] Kwekkeboom KL,Abbott-Anderson K,Cherwin C,et al. Pilot randomized controlled trial of a patient-controlled cognitive-behavioral intervention for the pain,fatigue,and sleep disturbance symptom cluster in cancer[J]. J Pain Symptom Manage,2012,44(6):810-822.
[27] Campbell CL,Campbell LC. A systematic review of cognitive behavioral interventions in advanced cancer[J]. Patient Educ Couns,2012,89(1):15-24.
[28] 黃麗霞,李華珍,吳秋霞,等. 分散注意力與認知行為干預在癌痛規范化治療中的效果研究[J]. 中國醫藥科學,2016,6(11):197-200.
(收稿日期:2019-09-11)

