腹腔鏡膽囊切除術與傳統開腹膽囊切除術治療膽結石臨床效果的對比分析

【摘要】" 目的" 通過臨床對比分析,探討腹腔鏡膽囊切除術對膽結石患者圍手術期指標、胃腸功能和并發癥的影響。方法" 選取2020年1月- 2022年12月醫院收治的60例膽結石患者作為研究對象,根據組間性別、年齡、結石直徑、結石數等基本資料均衡可比的原則進行分組,每組30例。觀察組采用腹腔鏡膽囊切除術治療,對照組采用傳統開腹膽囊切除術治療。對比兩組患者圍手術期指標手術時間、術中出血量、視覺模擬評分(VAS)及胃腸功能恢復情況、住院期間并發癥情況。結果" 手術過程中,觀察組患者手術時間短于對照組,術中出血量少于對照組,差異有統計學意義(Plt;0.05)。雙因素方差分析結果顯示,手術前、手術后6h、手術后12h,兩組患者VAS評分均逐漸降低,各觀察時點間差異有統計學意義(P時間lt;0.05);術后6h、12h,觀察組VAS評分均低于對照組,組間差異有統計學意義(P組間lt;0.05)。手術后,觀察組首次排便時間、肛門首次排氣時間、首次進食時間均短于對照組,差異有統計學意義(Plt;0.05);住院期間觀察組并發癥總發生率低于對照組,差異有統計學意義(Plt;0.05)。結論" "膽結石患者通過腹腔鏡膽囊切除術治療有利于改善手術指標,降低疼痛感,改善胃腸功能,降低并發癥。
【關鍵詞】" 膽結石;腹腔鏡膽囊切除術;出血量;胃腸功能;并發癥
中圖分類號" R657.41" " 文獻標識碼" A" " 文章編號" 1671-0223(2023)14--04
Comparative analysis of clinical effects of laparoscopic cholecystectomy and traditional open cholecystectomy in the treatment of gallstones Hou Yuchun. Department of Surgery, Funing County Traditional Chinese Medicine Hospital, Yancheng 224400, China
【Abstract】" Objective To explore the effect of laparoscopic cholecystectomy on perioperative parameters, gastrointestinal function and complications in patients with gallstones through clinical comparative analysis. Methods" Sixty patients with gallstones admitted to the hospital from January 2020 to December 2022 were selected as the research subjects. They were divided into groups based on the principle of balanced and comparable basic data such as gender, age, stone diameter, and number of stones between groups, with 30 patients in each group. The observation group was treated with laparoscopic cholecystectomy, and the control group was treated with traditional open cholecystectomy. Compare the perioperative indicators of surgery time, intraoperative bleeding volume, visual analogue pain score (VAS), gastrointestinal function recovery, and complications during hospitalization between two groups of patients. Results During the surgery, the observation group had shorter surgery time and less intraoperative bleeding compared to the control group, with a statistically significant difference (Plt;0.05). The results of bivariate analysis of variance showed that the VAS scores of the two groups of patients gradually decreased before surgery, 6 hours after surgery, and 12 hours after surgery, and there was a statistically significant difference between the observation points (Ptimelt;0.05). At 6 and 12 hours after surgery, the VAS score of the observation group was lower than that of the control group, and the difference between the groups was statistically significant (Pgrouplt;0.05). After surgery, the observation group had shorter first bowel movement time, first anal exhaust time, and first meal time compared to the control group, with statistically significant differences (Plt;0.05). The total incidence of complications in the observation group during hospitalization was lower than that in the control group, and the difference was statistically significant (Plt;0.05). Conclusion Laparoscopic cholecystectomy for gallstone patients can improve the surgical indicators, reduce pain, improve gastrointestinal function and reduce complications.
【Key words】" "Gallstone; Laparoscopic cholecystectomy; Bleeding volume; Gastrointestinal function; Complication
膽結石是指在膽道系統形成的結石,膽結石可以分為膽囊結石和膽管結石,通常所說的膽結石患者則理解為膽囊結石[1-2]。某些慢性疾病,包括肝臟疾病、糖尿病、部分內分泌疾病以及某些藥物、不健康的飲食生活習慣,都會促進膽囊結石的形成[3-6]。膽管結石的形成和膽管內的炎癥、異物、寄生蟲、病毒感染等有關,我國不同地區膽結石的發生率不同,具體的表現形式也不相同。膽結石的治療主要是根據結石相關的癥狀,以及是否合并有發癥,采取藥物或外科手術治療[7]。既往臨床中常用的治療方法主要為超聲碎石、傳統開腹膽囊切除術等,雖臨床療效肯定,但存在較多并發癥[8]。隨著腹腔鏡技術的發展與推廣,腹腔鏡膽囊切除術為患者的取石手術創造了更加有利的條件[9]。本研究通過臨床對比觀察,探討傳統開腹膽囊切除術與腹腔鏡膽囊切除術對膽結石患者圍手術期指標、胃腸功能和并發癥的影響,結果報告如下。
1" 對象與方法
1.1" 研究對象
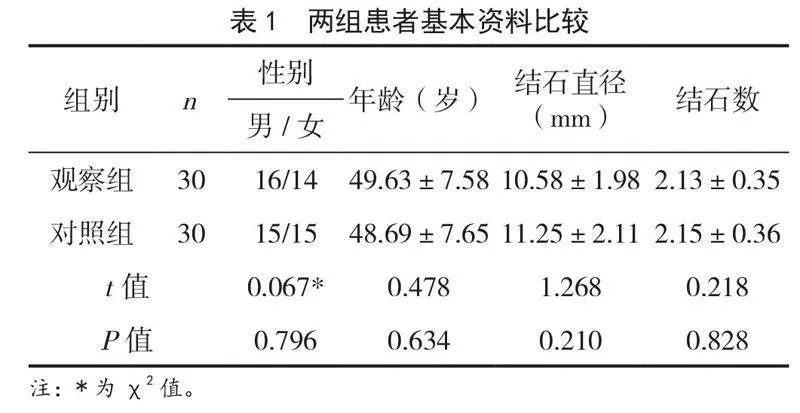
選取2020年1月- 2022年12月醫院收治的60例膽結石患者作為研究對象。納入標準:均符合《外科急腹癥診斷思路》中膽結石診斷標準[10];20~75歲;膽結石直徑3~15mm。排除標準:液系統疾病;存在膽道手術史;惡性腫瘤;肝內膽管狹窄、膽管囊狀擴張。根據組間性別、年齡、結石直徑、結石數等基本資料均衡可比的原則進行分組,每組30例。兩組患者基線資料比較,差異無統計學意義(Pgt;0.05),見表1。本研究經醫院醫學理論委員會通過。
1.2" 手術方法
1.2.1" 對照組" 采用傳統開腹膽囊切除術。作10cm左右的縱行手術切口,行腹壁切開的操作,組織分離,完全暴露病灶,解剖出膽囊管,離斷膽囊動脈,使得病灶切除,電凝止血,逐層縫合切口,術后引流。
1.2.2" 觀察組" 腹腔鏡膽囊切除術治療,于臍下1cm做切口,將腹腔鏡置入,取第2孔,于腋前線和肋弓交界處取第3孔。切除膽囊,顯露膽囊,取出膽囊,檢查術野,止血沖洗腹腔創面,縫合,術畢,常規給予5d抗生素,術后6周造影正常后拔管。
所有患者的手術均有同一小組的醫師、護士等工作人員共同參與完成。
1.3" 觀察指標
(1)圍手術期指標:包括手術時間、術中出血量。
(2)疼痛程度:通過視覺模擬評分(VAS)評估患者疼痛程度,總分10分,分數越高,疼痛越重[11]。
(3)術后胃腸功能:包括首次排便時間、肛門首次排氣時間、首次進食時間。
(4)并發癥情況:包括肺部感染、腹部感染。
1.4" 數據分析方法
運用SPSS 26.0統計學軟件分析處理數據,計數資料計算百分率(%),組間率比較采用χ2檢驗;計量資料用“均數±標準差”表示,兩組間均數比較采用t檢驗;各觀察時點間及組間均數比較采用雙因素重復測量的方差分析。以Plt;0.05為差異有統計學意義。
2" 結果
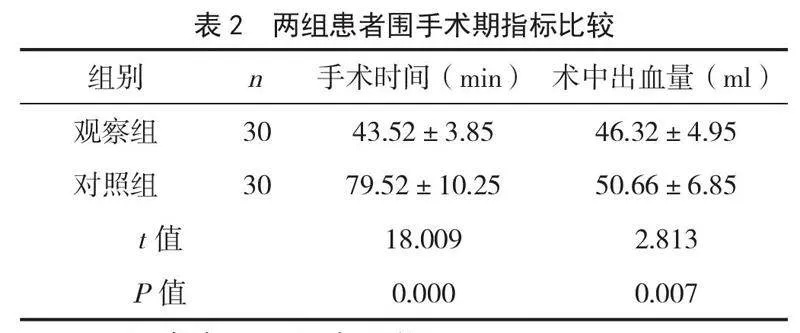
2.1" 兩組患者圍手術期指標比較
手術過程中,觀察組手術時間短于對照組,術中出血量少于對照組,差異有統計學意義(Plt;0.05),見表2。
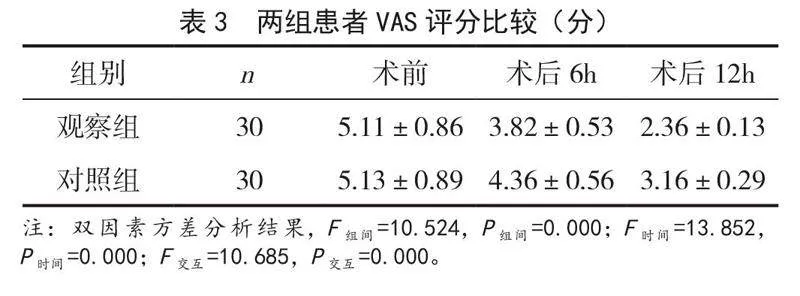
2.2" 兩組患者VAS評分比較
雙因素方差分析結果顯示,手術前、手術后6h、手術后12h,兩組患者VAS評分均逐漸降低,各觀察時點間差異有統計學意義(P時間lt;0.05);術后6h、12h,觀察組VAS評分均低于對照組,組間差異有統計學意義(P組間lt;0.05),見表3。
2.3" 兩組患者術后胃腸功能比較
手術后,觀察組首次排便時間、肛門首次排氣時間、首次進食時間均短于對照組,差異有統計學意義(Plt;0.05),見表4。
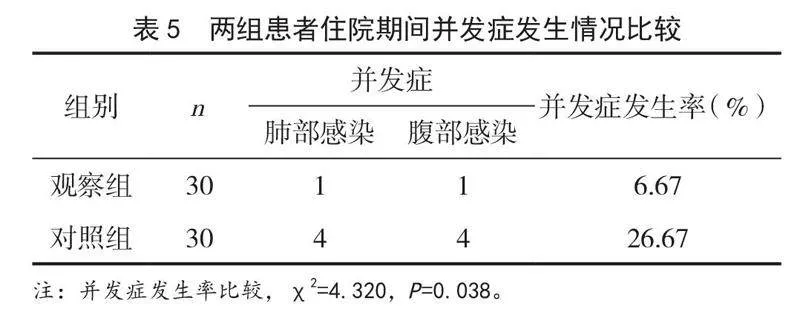
2.4" 兩組患者并發癥發生情況比較
手術后,觀察組出現肺部感染1例,腹部感染1例,對照組出現肺部感染4例,腹部感染4例,觀察組住院期間并發癥總發生率低于對照組,差異有統計學意義(Plt;0.05),見表5。
3" 討論
膽結石是指膽道系統包括膽囊或膽管內發生結石的疾病。膽結石包含2個部分,一個是膽囊結石,另一個是肝內膽管或是肝外膽管結石。膽道系統形成結石的機制與膽汁代謝有關,但目前對于膽囊結石或者是膽管結石的發病的原因尚不清楚,通常與生活環境、飲食習慣、生存地域以及生活環境的水質等有關[12-14]。不同手術對患者的影響存在差異,目前臨床上需尋求安全有效的治療方法。
本研究發現,觀察組手術時間于對照組,觀察組術中出血量均少于對照組,提示膽結石患者通過腹腔鏡膽囊切除術治療可縮短術時間、術中出血量。采用傳統開腹膽囊切除術難以取出,有利于進一步將結石破碎后,取出更加方便快捷[15]。腹腔鏡膽囊切除術治療膽結石患者促進患者的恢復原因可能是由于腹腔鏡膽囊切除術可其創傷較小,有助于保護患者的空腔臟器,促進恢復,提高手術效率。本研究中,觀察組VAS評分低于對照組,提示腹腔鏡膽囊切除術治療膽結石患者,可緩解疼痛感。研究指出,腹腔鏡膽囊切除術治療膽結石患者,有利于緩解患者的疼痛感[16]。因此,本研究和上述相關報道一致表明腹腔鏡膽囊切除術治療可緩解膽結石患者疼痛感。
本研究還發現,觀察組術后恢復優于對照組,提示膽結石患者通過腹腔鏡膽囊切除術治療可改善胃腸功能。腹腔鏡膽囊切除術手術簡單方便,促進患者恢復,對患者的影響較小,手術用時較少[17-18]。此外,腹腔鏡膽囊切除術在臨床中表現為創傷小、易于操作,在治療膽結石中的效果較為明顯[19]。此外,觀察組住院期間并發癥總發生率低于對照組,提示膽結石患者通過腹腔鏡膽囊切除術治療可降低并發癥。研究指出,在行腹腔鏡治療之前,應充分進行手術指征評估,降低并發癥[20]。
綜上所述,膽結石患者通過腹腔鏡膽囊切除術治療有利于改善手術指標,降低疼痛感,改善胃腸功能,降低并發癥。
4" 參考文獻
[1] Talha A,Abdelbaki T,Farouk A,et al.Cholelithiasis after bariatric surgery,incidence,and prophylaxis:Randomized controlled trial[J].Surg Endosc,2020,34(12):5331-5337.
[2] Villarroel M,de la Serna-Higuera C,Pérez-Miranda M.Single-session endoscopic ultrasound-guided gallbladder drainage combined with ERCP for acute cholecystitis and choledocholithiasis in a nonsurgical patient[J].Endoscopy,2021,53(7):275-276.
[3] Ruiz Pardo J,García Marín A,Ruescas García FJ,et al.Differences between residual and primary choledocholithiasis in cholecystectomy patients[J].Rev Esp Enferm Dig,2020,112(8):615-619.
[4] Lyu Y,Cheng Y,Li T,et al.Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis:A meta-analysis[J].Surg Endosc,2019,33(10):3275-3286.
[5] Leong HY,Chang YK,Ooi CW,et al.Liquid biphasic electric partitioning system as a novel integration process for betacyanins extraction from red-purple pitaya and antioxidant properties assessment[J].Front Chem,2019,7(15):201.
[6] Kuo CM,Chiu YC,Liang CM,et al.Limited precut sphincterotomy combined with endoscopic papillary balloon dilation for common bile duct stone removal in patients with difficult biliary cannulation[J].BMC Gastroenterol,2016,16(1):1-6.
[7] Littlefield A,Lenahan C.Cholelithiasis:Presentation and management[J].J Mid Wom Heal,2019,64(3):289-297.
[8] Reiter S,Dunkel A,Dawid C,et al.Targeted LC-MS/MS profiling of bile acids in various animal tissues[J].J Agric Food Chem,2021,69(36):10572-10580.
[9] Zou Q,Ding Y,Li CS,et al.A randomized controlled trial of emergency LCBDE+LC and ERCP+LC in the treatment of choledocholithiasis with acute cholangitis[J].Wideochir Inne Tech Maloinwazyjne,2022,17(1):156-162.
[10] 金中奎.外科急腹癥診斷思路[M].北京:人民軍醫出版社,2010:102-103.
[11] Lyu Y,Cheng Y,Li T,et al.Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic" retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis:A meta-analysis[J].Surg Endosc,2019,33(10):3275-3286.
[12] 嚴廣斌.視覺模擬評分法[J].中華關節外科雜志:電子版,2014,8(2):12.
[13] Miri SR,Movaghar ER,Safaei M,et al.Neuroendocrine tumor of the common bile duct:A case report of extremely rare cause for obstructive jaundice[J].Int J Surg Case Rep,2020,77(18):303-306.
[14] Sabbah M,Nakhli A,Bellil N,et al.Predictors of failure of endoscopic retrograde pancreatocholangiography during common bile duct stones[J].Heliyon,2020,6(11):515-518.
[15] 馬芳,張勇,張劍. ERCP與LCBDE治療膽總管結石患者的臨床療效觀察[J].肝膽外科雜志,2019,27(3):183-186.
[16] 裴賽麗,王震宇.腹腔鏡聯合十二指腸鏡與膽總管一期縫合治療膽囊合并膽總管結石的療效比較[J].中華消化內鏡雜志,2020,37(6):435-440.
[17] Nagem R,Alberti LR,de Campos-Lobato LF.Is it safe to recommend cholecystectomy whenever gallstones develop after bariatric surgery?[J].Obes Surg,2021,31(1):179-184.
[18] Singh K,Dahiya D,Kaman L,et al.Prevalence of non-alcoholic fatty liver disease and hypercholesterolemia in patients with gallstone disease undergoing laparoscopic cholecystectomy[J].Pol Przegl Chir,2019,92(1):18-22.
[19] Campagna RAJ, Belette AM, Holmstrom AL,et al.Addressing the gap in laparoscopic common bile duct exploration training for rural surgeons:Imparting procedural ability is not enough[J].Surg Endosc,2021,35(9):5140-5146.
[20] Mwachiro M,Chol N,Simel I,et al.Establishment of an endoscopic retrograde cholangiopancreatography (ERCP) program in rural Kenya:A review of patient and trainee outcomes[J].Surg Endosc,2021,35(12):7005-7014.
[2023-04-12收稿]