急性冠脈綜合征患者CYP2C19基因多態性與氯吡格雷療效的關系
王光亮 林爽 吳雪梅
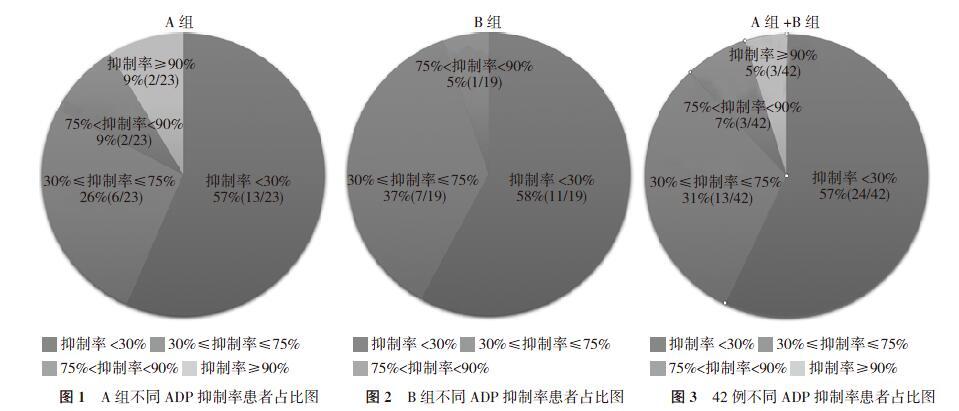
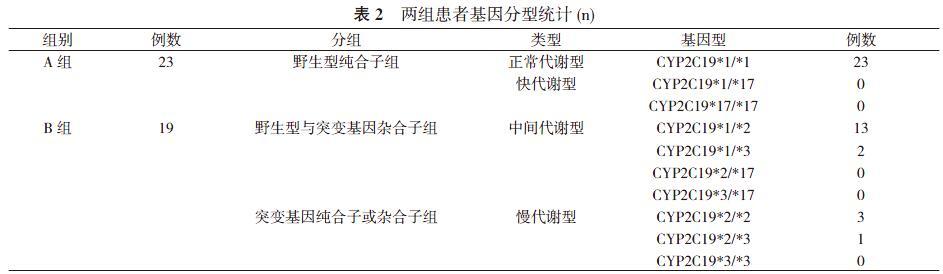
【摘要】 目的 探討急性冠狀動脈(冠脈)綜合征患者CYP2C19基因多態性與氯吡格雷療效的關系。方法 42例急性冠脈綜合征患者, 根據CYP2C19基因多態性分為A組(正常代謝+快代謝型, 23例)和B組(中間代謝+慢代謝型, 19例)。。兩組患者均行CYP2C19基因型檢測、血栓彈力圖檢測。觀察比較兩組患者二磷酸腺苷(ADP)抑制情況、ADP抑制率, 并統計基因分型。結果 A組中野生型純合子組包括正常代謝型患者23例, 均為CYP2C19*1/*1基因型;快代謝型0例。B組中野生型與突變基因雜合子組包括中間代謝型患者15例, 其中CYP2C19*1/*2基因型13例, CYP2C19*1/*3基因型2例;突變基因純合子或雜合子組包括慢代謝型患者4例, 其中CYP2C19*2/*2基因型3例, CYP2C19*2/*3基因型1例。B組中ADP抑制率<30%的發生率為58%, 高于A組的57%, 但差異無統計學意義(P>0.05)。42例患者中服用氯吡格雷后ADP抑制率<30%患者24例(57%), 其中停用氯吡格雷更換為替格瑞洛繼續服用患者14例(33%), 14例患者中替格瑞洛頓服12 h后復查血小板ADP抑制率均>30%患者13例(31%), 但仍有ADP抑制率<30%患者1例(2%)。A組平均ADP抑制率為(39.5±28.4)%, B組平均ADP抑制率為(31.5±21.6)%, B組平均ADP抑制率低于A組, 但差異無統計學意義(P>0.05)。結論 本研究結果支持CYP2C19多態性僅為眾多影響氯吡格雷療效的因素之一, 并不能最終決定氯吡格雷療效。氯吡格雷服用后的抗血小板聚集療效, 還受眾多其他因素的影響, 仍需進一步研究。
【關鍵詞】 CYP2C19基因;血栓彈力圖;血小板;二磷酸腺苷抑制率
DOI:10.14163/j.cnki.11-5547/r.2019.31.003
Correlation between CYP2C19 gene polymorphism and clopidogrel efficacy in patients with acute coronary syndrome ? WANG Guang-liang, LIN Shuang, WU Xue-mei. Northeastern International Hospital Geriatrics Center, Shenyang 110000, China
【Abstract】 Objective ? To discuss the correlation between CYP2C19 gene polymorphism and clopidogrel efficacy in patients with acute coronary syndrome. Methods ? A total of 42 patients with acute coronary syndrome were divided into two groups: group A (normal metabolism type + fast metabolism type,23 cases) and group B (intermediate metabolism type + slow metabolism type, 19 cases) according to CYP2C19 gene polymorphism. All patients were tested for CYP2C19 genotype and thromboelastography. The general information, adenosine diphosphate (ADP) inhibition, CYP2C19 gene polymorphism and ADP inhibition rate of the two groups were observed and compared, and the genotypes were analyzed. Results ? In group A, the wild-type homozygous group included 23 patients with normal metabolic type, all of whom were CYP2C19 * 1 / * 1 genotype, and 0 patient with fast metabolic type. In group B, the heterozygotes of wild type and mutant gene group included 15 patients with intermediate metabolism, of which 13 patients with CYP2C19 * 1 / * 2 genotype and 2 patients with CYP2C19 * 1 / * 3 genotype. The homozygous or heterozygous group of the mutant gene included 4 patients with slow metabolism, of which 3 patients with CYP2C19 * 2 / * 2 genotype and 1 patient with CYP2C19 * 2 / * 3 genotype. The incidence of ADP inhibition rate <30% was 58% in group B, which was higher than 57% in group A, but the difference was not statistically significant (P>0.05). Of the 42 patients,24 cases (57%) had ADP inhibition rate <30% after taking clopidogrel, of which 14 cases (33%) who discontinued clopidogrel and changed to telgrelor. Among the 14 patients, 13 cases (31%) had platelet ADP inhibition rate >30% after 12 h of tegriloton administration, but 1 case (2%) had ADP inhibition rate of<30%. The mean ADP inhibition rate was (39.5±28.4)% in group A, which was (31.5±21.6)% in group B, the mean ADP inhibition rate in group B was lower than that in group A, but the difference was not statistically significant (P>0.05). Conclusion ? The results of this study support that CYP2C19 polymorphism is only one of the factors that affect the efficacy of clopidogrel, and cannot ultimately determine the efficacy of clopidogrel. The anti-platelet aggregation effect of clopidogrel is also influenced by many other factors, which need further study.
【Key words】 CYP2C19 gene; Thromboelastogram; Platelet; adenosine diphosphate inhibition rate
氯吡格雷是一種需要細胞色素P450(CYP450)進行生物轉化的前藥[1, 2], 需要肝細胞色素P450 2C19(CYP2C19)的干預才能激活[3], 所以肝細胞色素P450 2C19(CYP2C19)基因多態性簡稱CYP2C19基因多態性, 有可能會影響到氯吡格雷的抗血小板聚集作用[4-6]。氯吡格雷的反應存在個體間差異, 不同患者服用氯吡格雷后會出現不同的抗血小板聚集療效[3]。服用氯吡格雷后的抗血小板聚集療效, 可以通過血栓彈力圖ADP抑制率表達出來[7, 8]。本研究主要為評價CYP2C19 基因多態性與血栓彈力圖ADP抑制率之間是否存在聯系展開病例統計分析, 進而探討CYP2C19 基因多態性是否會決定患者服用氯吡格雷后的抗血小板聚集療效。現報告如下。
1 資料與方法
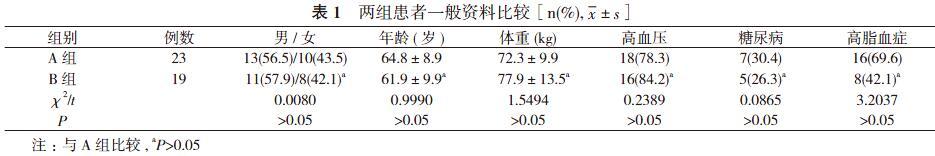
1. 1 一般資料 選取2018年4~11月本院住院的42名急性冠脈綜合征患者作為研究對象, 患者中男24例, 女18例;年齡39~82歲。根據CYP2C19 基因多態性分為A組(正常代謝+快代謝型, 23例)和B組(中間代謝+慢代謝型, 19例)。
A組中野生型純合子組包括正常代謝型(CYP2C19*1/*1)、快代謝型(CYP2C19*1/*17、CYP2C19*17/*17)。B組中野生型與突變基因雜合子組包括中間代謝型(CYP2C19*1/*2、CYP2C19*1/*3、CYP2C19*2/*17、CYP2C19*3/*17);突變基
因純合子或雜合子組包括慢代謝型(CYP2C19*2/*2、CYP2C19*2/*3、CYP2C19*3/*3)。兩組患者性別、年齡、體重等一般資料比較差異無統計學意義(P>0.05), 具有可比性。見表1。入選患者均同期行CYP2C19基因多態性檢測及血栓彈力圖ADP抑制率檢測, 所有患者行血栓彈力圖ADP抑制率檢測前確定已頓服300 mg氯吡格雷[商品名:波立維, 賽諾菲(杭州)制藥有限公司]或75 mg氯吡格雷1次/d至少4 d, 保證行血栓彈力圖ADP抑制率檢測采血前氯吡格雷累積量>300 mg。排除標準:①血小板計數>400×109/L或<100×109/L;②阿司匹林或氯吡格雷使用禁忌證;③嚴重肝臟疾病或凝血功能存在異常者;④嚴重貧血、感染或甲狀腺功能亢進等疾病者。
1. 2 方法
1. 2. 1 CYP2C19基因型檢測方法 采集患者靜脈血2 ml
(EDTA-K2抗凝), 使用天根血液基因組DNA提取試劑盒 (TIANamp Blood DNA Kit DP 318) 提取血液基因組DNA。應用美國Light Cycler cobas z480儀器檢測, 應用武漢友芝友醫療科技股份有限公司生產的人類CYP2C19基因檢測試劑盒, 根據基因檢測結果及試劑盒說明書分組。
1. 2. 2 血栓彈力圖檢測方法 血小板ADP抑制率檢測使用 TEG5000型凝血分析儀, 試劑包括高嶺土(含15% Kadin液)、激活劑、花生四烯酸(arachidonicacid, AA)和二磷酸腺苷(adenosine diphosphate, ADP), 均為美國Haemonetics公司產品。所有患者抽取靜脈血, 置于含3.13%枸櫞酸鈉進行檢查。
1. 2. 3 用藥方法 服用氯吡格雷后ADP抑制率<30%患者, 依據患者病情停用氯吡格雷更換為替格瑞洛繼續服用, 替格瑞洛方法為首劑180 mg頓服后改為90 mg/次, 2次/d 口服。
1. 3 觀察指標及判定標準 觀察比較兩組患者ADP抑制情況、ADP抑制率, 并統計基因分型。判定標準:以ADP誘導的血小板抑制率<30%為氯吡格雷低反應(LCR), ≥30%定義為氯吡格雷正常反應。ADP誘導聚集后的血小板抑制率(ADP抑制率)用于監測氯吡格雷療效。ADP抑制率<30%為無效, 30%≤ADP抑制率≤75%為起效, 75% 1. 4 統計學方法 采用SPSS19.0統計學軟件處理數據。計量資料以均數±標準差( x-±s)表示, 采用t檢驗;計數資料以率(%)表示, 采用χ2檢驗。P<0.05表示差異有統計學意義。 2 結果 2. 1 兩組患者基因分型統計 A組中野生型純合子組包括正常代謝型患者23例, 均為CYP2C19*1/*1基因型;快代謝型0例。B組中野生型與突變基因雜合子組包括中間代謝型患者15例, 其中CYP2C19*1/*2基因型13例, CYP2C19*1/*3基因型2例;突變基因純合子或雜合子組包括慢代謝型患者4例, 其中CYP2C19*2/*2基因型3例, CYP2C19*2/*3基因型1例。見表2。 2. 2 兩組患者ADP抑制情況比較 A組中服用氯吡格雷后ADP抑制率<30%患者13例(57%)。見圖1。其中停用氯吡格雷更換為替格瑞洛繼續服用患者10例(43%)。替格瑞洛頓服12 h后復查血小板ADP抑制率, ADP抑制率>30%患者9例(39%), ADP抑制率<30%患者1例(4%), 具體原因不詳。見圖1。B組中服用氯吡格雷后ADP抑制率<30%患者11例(58%), 其中停用氯吡格雷更換為替格瑞洛繼續服用患者4例(21%)。替格瑞洛頓服12 h后復查血小板ADP抑制率, ADP抑制率均>30%患者4例(21%)。見圖2。B組中ADP抑制率<30%的發生率高于A組, 但差異無統計學意義(P>0.05)。 A組+B組42例患者中服用氯吡格雷后ADP抑制率<30%患者24例(57%), 其中停用氯吡格雷更換為替格瑞洛繼續服用患者14例(33%), 14例患者中替格瑞洛頓服12 h后復查血小板ADP抑制率均>30%患者13例(31%), 但仍有ADP抑制率<30%患者1例(2%), 具體原因不詳。見圖3。 2. 3 兩組患者ADP抑制率比較 A組平均ADP抑制率為(39.5±28.4)%, B組平均ADP抑制率為(31.5±21.6)%, B組平均ADP抑制率低于A組, 但差異無統計學意義(t=1.0094, P>0.05)。 3 討論 急性冠脈綜合征是常見的心血管系統疾病, 影響患者的生存時間及生存質量[9-11]。我國人群CYP2C19基因多態性多以基因型(*1/*1)為主。氯吡格雷是急性冠脈綜合征患者廣泛應用的藥物。 針對CYP2C19基因多態性與氯吡格雷療效的研究, 目前主要有以下兩種觀點:一種是支持CYP2C19基因多態性與氯吡格雷療效有關的研究:①Hou等[12]的薈萃分析表明, CYP2C19基因多態性中的CYP2C19*2基因型可能與氯吡格雷抵抗有關。②Idrissi等[13]的研究結果支持CYP2C19基因多態性與氯吡格雷抵抗具有明顯相關性。③Li等[14]研究發現:CYP2C19基因多態性與PCI術后1年心血管事件的高風險具有明顯相關性。④Zhong等[15]的文章提出CYP2C19基因突變(CYP2C19*2)和(CYP2C19*3)影響中國較多的人口, 并且這種突變與氯吡格雷抵抗和主要心血管不良事件的風險增加密切相關。⑤研究表明[16], 支架血栓形成與CYP2C19*2 突變導致的氯吡格雷抵抗有關, 而CYP2C19*17可能在這一過程中起到保護作用。⑥Chen等[17]研究表明, 性別、年齡、糖尿病、高血壓和高脂血癥可能導致患者對氯吡格雷低反應性。 另一種是支持CYP2C19多態性與氯吡格雷療效無關的研究:①Charfi等[18]研究了接受氯吡格雷治療1個月的71例冠心病患者, 沒有觀察到CYP2C19*2等位基因與心血管事件的發生有顯著相關性。②Notarangelo等[19]的文章指出CYP2C19基因型僅解釋了12%的氯吡格雷反應變異性, 這表明除CYP2C19以外的因素可能是更重要的。③Bouman等[20]的研究顯示CYP2C19基因型無論是慢代謝還是快代謝, 均未對氯吡格雷療效產生明顯的影響。④Calderon-Cruz等[21]提出氯吡格雷藥物低反應性與基因多態性無關。 正是由于目前以上兩種觀點爭論較為激烈, 本研究主要圍繞基因型分組, 分別檢測血小板聚集率, 探討急性冠脈綜合征患者CYP2C19基因多態性與氯吡格雷療效的關系。 本研究結果顯示, 急性冠脈綜合征患者中, B組中ADP抑制率<30%的發生率高于A組, 但差異無統計學意義(P>0.05)。說明CYP2C19基因多態性并不能完全決定服用氯吡格雷后的血栓彈力圖ADP抑制率, 支持CYP2C19多態性僅為眾多影響氯吡格雷療效的因素之一, 并不能最終決定氯吡格雷療效。同時本研究結果提示, 服用氯吡格雷后血小板ADP抑制率<30%的發生率高, 但更換成替格瑞洛后ADP抑制率多數均>30%, 但仍有ADP抑制率<30%患者1例, 具體原因不詳。 本研究入組人群數量有限, 推斷氯吡格雷療效還受眾多其他因素的影響, 但是為何種因素具體如何影響, 仍需進一步研究。 參考文獻 [1] Hankey GJ. Prasugrel or clopidogrel for long-term secondary stroke prevention? Lancet Neurol, 2019, 18(3):222-223. [2] Prasad K, Siemieniuk R, Hao Q, et al. Dual antiplatelet therapy with aspirin and clopidogrel for acute high risk transient ischaemic attack and minor ischaemic stroke: a clinical practice guideline. BMJ, 2018(363):k5130. [3] Jovani M, Chan AT. Do Aspirin and Clopidogrel Follow the Same Road Toward Prevention of Colorectal Cancer?Clinical Gastroenterology and Hepatology, 2019, 17(10):1945-1947. [4] Tangamornsuksan W, Thiansupornpong P, Morasuk T, et al. A pharmacokinetic model of drug-drug interaction between clopidogrel and omeprazole at CYP2C19 in humans. Conf Proc IEEE Eng Med Biol Soc, 2017(2017):2704-2707. [5] 楊玲, 刁珊珊, 丁意平,等. 負荷劑量氯吡格雷治療輕型缺血性腦卒中/短暫性腦缺血發作的作用及機制. 中華醫學雜志, 2019, 99(5):349-353. [6] Larson EA, Miller NJ. Point-Counterpoint: CYP2C19 Genotyping for Clopidogrel. SD Med, 2017, 70(1):13-15. [7] Li RH, Stern JA, HoV, et al. Platelet Activation and Clopidogrel Effects on ADP-Induced Platelet Activation in Cats with or without the A31P Mutation in MYBPC3. Journal of Veterinary Internal Medicine, 2016, 30(5):1619-1629. [8] Jin L, Yu H, Dong T, et al. The Prognostic Value of ADP-Induced Platelet Aggregation for Bleeding Complications in Low- Intermediate Risk Patients With Acute Coronary Syndrome Taking Clopidogrel After Percutaneous Coronary Intervention. Heart Lung & Circulation, 2017, 26(1):49-57. [9] Bonello L, Laine M, Lenesle G, et al. Meta-Analysis of Potent P2Y12-ADP Receptor Antagonist Therapy Compared to Clopidogrel Therapy in Acute Coronary Syndrome Patients with Chronic Kidney Disease. Thromb Haemost, 2018, 118(10):1839-1846. [10] Siasos G, Kioufis S, Oikonomou E, et al. Impact of C34T P2Y12 ADP receptor polymorphism and smoking status on cardiovascular outcome in coronary artery disease patients receiving clopidogrel. International Journal of Cardiology, 2016, 210(12):161-163. [11] Martischnig AM, Mehilli J, Pollak J, et al. Impact of Dabigatran versus Phenprocoumon on ADP Induced Platelet Aggregation in Patients with Atrial Fibrillation with or without Concomitant Clopidogrel Therapy (the Dabi-ADP-1 and Dabi-ADP-2 Trials). Biomed Research International, 2015(2015):1-10. [12] Hou X, Shi J, Sun H. Gene polymorphism of cytochrome P450 2C19*2 and clopidogrel resistance reflected by platelet function assays: a meta-analysis. European Journal of Clinical Pharmacology, 2014, 70(9):1041-1047. [13] Idrissi HH, Hmimech W, Khorb NE, et al. A synergic effect between CYP2C19*2, CYP2C19*3 loss-of-function and CYP2C19*17 gain-of-function alleles is associated with Clopidogrel resistance among Moroccan Acute Coronary Syndromes patients. Bmc Research Notes, 2018, 11(1):46. [14] Li X, Wang Z, Wang Q, et al. Clopidogrel-associated genetic variants on inhibition of platelet activity and clinical outcome for acute coronary syndrome patients. Basic Clin Pharmacol Toxicol. 2019, 124(1):84-93. [15] Zhong Z, Hou J, Li B, et al. Analysis of CYP2C19 Genetic Polymorphism in a Large Ethnic Hakka Population in Southern China. Medical Science Monitor International Medical Journal of Experimental & Clinical Research, 2017(23):6186-6192. [16] Kirac D, Erdem A, Avcilar T, et al. Effects of genetic factors to stent thrombosis due to clopidogrel resistance after coronary stent placement. Cell Mol Biol (Noisy-le-grand), 2016, 62(1):51-55. [17] Chen K, Zhang R, Liu H, et al. Impact of the CYP2C19 Gene Polymorphism on Clopidogrel Personalized Drug Regimen and the Clinical Outcomes. Clinical Laboratory, 2016, 62(9):1773-1780. [18] Charfi R, Mzoughi K, Boughalleb M, et al. Response to clopidogrel and of the cytochrome CYP2C19 genepolymorphism. La Tunisie medicale, 2018, 96(3):209-218. [19] Notarangelo MF, Bontardelli F, Merlini PA. Genetic and nongenetic factors influencing the response to clopidogrel. Journal of Cardiovascular Medicine, 2013, 14(14 Suppl 1):S1-S7. [20] Bouman HJ, Sch?mig E, Werkum JWV, et al. Paraoxonase-1 is a major determinant of clopidogrel efficacy. Nature Medicine, 2011, 17(1):110-116. [21] Calderón-Cruz B, Rodríguez-Galván K, Manzo-Francisco LA, et al. C3435T polymorphism of the ABCB1 gene is associated with poor clopidogrel responsiveness in a Mexican population undergoing percutaneous coronary intervention. Thrombosis Research, 2015, 136(5):894-898. [收稿日期:2019-06-21]

