烏司他丁對體外循環患兒炎癥反應及氧自由基清除能力的影響觀察
尹記輝
【摘要】 目的:觀察烏司他丁對體外循環(CPB)患兒炎癥反應及氧自由基清除能力的影響。方法:選擇2018年3月-2021年3月泰安市婦幼保健院收治的室間隔或房間隔缺損患兒120例作為研究對象,按照隨機數字表法將患兒分為觀察組及對照組,各60例。兩組均根據患兒不同情況給予CPB房間隔修補術或室間隔修補術,觀察組于開胸后主動脈插管前給予烏司他丁10 000 U/kg靜脈推注半量,另外半量混入CPB預充液中隨轉機進入體內;對照組將烏司他丁換為等量生理鹽水給予同觀察組相同操作。記錄比較兩組麻醉時間、手術時間、CPB時間、主動脈阻斷時間及住院時間;分別于術前(T0)、CPB停止4 h(T1)及術后24 h(T2)采血測定炎癥因子水平,包括血漿白細胞介素-6(IL-6)、白細胞介素-8(IL-8)、白細胞介素-10(IL-10)、腫瘤壞死因子-α(TNF-α)及C反應蛋白(CRP)水平,氧自由基清除指標包括血漿超氧化物歧化酶(SOD)、丙二醛(MDA)水平,比較不同時間兩組各因子水平差異。結果:兩組麻醉時間、手術時間、CPB時間、主動脈阻斷時間、住院時間比較,差異均無統計學意義(P>0.05)。兩組T0的IL-6、TNF-α、IL-8、IL-10、SOD、MDA比較,差異均無統計學意義(P>0.05);T1、T2,對照組IL-6、TNF-α、IL-8、MDA及觀察組IL-6、TNF-α、MDA均高于T0,觀察組上述指標均低于對照組,兩組IL-10均高于T0,且觀察組均高于對照組(P<0.05);觀察組T1的IL-8高于T0,但低于對照組(P<0.05);對照組T1、T2及觀察組T1的SOD均低于T0,觀察組T1、T2的SOD均高于對照組,差異均有統計學意義(P<0.05);T2,兩組IL-6、TNF-α、IL-10、MDA及對照組IL-8均低于T1,對照組SOD高于T1,差異均有統計學意義(P<0.05)。結論:在患兒CPB心臟手術中,烏司他丁可有效抑制促炎因子升高,上調抗炎介質的釋放,促進氧自由基清除,從而減少機體損傷。
【關鍵詞】 烏司他丁 體外循環 炎癥反應 氧自由基
Effect of Ulinastatin on Inflammatory Response and Oxygen Free Radical Scavenging Ability in Children Undergoing Cardiopulmonary Bypass/YIN Jihui. //Medical Innovation of China, 2022, 19(11): 00-005
[Abstract] Objective: To observe the effect of Ulinastatin on inflammatory response and oxygen free radical scavenging ability in children undergoing cardiopulmonary bypass (CPB). Method: A total of 120 children with ventricular septal or atrial septal defect treated in Tai’an Maternal and Child Health Care Hospital from March 2018 to March 2021 were selected as the research objects, according to the random number table method, the children were divided into observation group and control group, 60 cases in each group. Both groups were given CPB atrial septal repair or ventricular septal repair according to different conditions of children, the observation group was given half of Ulinastatin 10 000 U/kg intravenously before aortic intubation after thoracotomy, and the other half was mixed into CPB precharge and entered the body with the turn; in the control group, Ulinastatin was replaced with the same amount of Normal Saline and given the same operation as the observation group. Anesthesia time, operation time, CPB time, aortic occlusion time and hospital stay were recorded and compared between the two groups; the levels of inflammatory factors, including plasma interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-10 (IL-10) and tumor necrosis factor-α (TNF-α), and oxygen radical scavenging index, including plasma superoxide dismutase (SOD) and malondialdehyde (MDA) were measured before operation (T0), 4 h after CPB (T1) and 24 h after operation (T2), the above indexes were compared between the two groups at different times. Result: There were no significant differences in anesthesia time, operation time, CPB time, aortic occlusion time and hospital stay between the two groups (P>0.05). There were no significant differences in IL-6, TNF-α, IL-8, IL-10, SOD and MDA between the two groups at T0 (P>0.05); at T1 and T2, IL-6, TNF-α, IL-8, MDA in the control group, and IL-6, TNF-α, MDA in the observation group were higher than those at T0, the above indexes in the observation group were lower than those in the control group, IL-10 of the two groups were higher than those at T0, and the observation group were higher than those in the control group (P<0.05); IL-8 in the observation group at T1 was higher than that at T0, and that in the observation group was lower than that in the control group (P<0.05); the SOD of the control group at T1 and T2 and the observation group at T1 were lower than those at T0, and the SOD of the observation group at T1 and T2 were higher than those of the control group, the differences were statistically significant (P<0.05); at T2, IL-6, TNF-α, IL-10, MDA in the two groups and IL-8 in the control group were lower than those at T1, and SOD in the control group was higher than that at T1, the differences were statistically significant (P<0.05). Conclusion: Ulinastatin can effectively inhibit the increase of pro-inflammatory factors, up regulate the release of anti-inflammatory mediators, promote oxygen free radical scavenging and reduce body damage during CPB heart surgery in children.
[Key words] Ulinastatin Cardiopulmonary bypass Inflammatory reaction Oxygen free radical
First-author’s address: Tai’an Maternal and Child Health Care Hospital, Shandong Province, Tai’an 271000, China
doi:10.3969/j.issn.1674-4985.2022.11.001
體外循環(CPB)是嬰幼兒先天性心臟病心臟直視手術治療中的必備條件,在心臟停搏的情況下為其他組織器官提供血液供應[1-2]。在成年人中,體外循環心臟手術與全身炎癥反應(SIR)顯著升高相關,全身炎癥反應可導致嚴重術后并發癥,CPB引發的氧自由基的釋放、炎癥級聯的激活可引起多臟器損傷[3]。兒科患兒,尤其是嬰兒和新生兒,循環血漿量少,器官不成熟,因此,CPB引起的低體溫、循環變化、血液稀釋、酸堿平衡和全身炎癥反應綜合征(SIRS)的影響比成人大得多,且嬰幼兒可能有不成熟的抗氧化防御系統,因此更容易受到氧化劑應激的影響[4-5]。烏司他丁是一種尿胰蛋白酶抑制劑,被用于治療胰腺炎、膿毒癥等炎癥疾病,已有研究表明其可減少CPB后缺血再灌注損傷,從而保護心肝腎等重要臟器[6-8]。本研究選取需手術治療的先天性心臟病患兒,研究烏司他丁對體外循環患兒炎癥反應及氧自由基清除能力的影響,報道如下。
1 資料與方法
1.1 一般資料 選擇2018年3月-2021年3月泰安市婦幼保健院收治的先天性心臟病患兒120例作為研究對象,納入標準:所有患兒均行常規術前胸片檢查、心電圖、超聲心動圖、全血細胞計數和生化檢查等,確診有室間隔或房間隔缺損并需手術治療。排除標準:(1)術前存在感染;(2)凝血功能障礙;(3)肺、肝、腎功能障礙;(4)圍手術期使用類固醇治療;(5)過敏體質。按照隨機數字表法將患者分為觀察組及對照組,各60例。患兒監護人知情同意本研究,且本研究經醫院倫理委員會批準。
1.2 方法 所有患兒均在靜吸復合麻醉下進行手術,手術方式根據患兒不同情況給予房間隔修補術或室間隔修補術。于胸骨正中切口建立CPB,根據患兒缺損部位選擇心臟切口并進行缺損縫補,待患兒各指標穩定后縫合關胸。CPB建立:預充液采用乳酸格林液為基礎液,阻斷主動脈后灌注停跳液,輔以心臟局部深低溫,肝素化后插管并建立CPB。觀察組于開胸后主動脈插管前給予烏司他丁(生產廠家:廣東天普生化醫藥股份有限公司,批準文號:國藥準字H19990134,規格:10萬單位)10 000 U/kg靜脈推注半量,另外半量混入CPB預充液中隨轉機進入體內;對照組將烏司他丁換為等量生理鹽水給予同觀察組相同操作。
1.3 觀察指標 (1)比較兩組手術及住院指標:麻醉時間、手術時間、CPB時間、主動脈阻斷時間及住院時間;(2)比較兩組炎癥因子水平及氧自由基清除指標:分別于術前(T0)、CPB停止4 h(T1)及術后24 h(T2)采血測定炎癥因子水平,包括血漿白細胞介素-6(IL-6)、白細胞介素-8(IL-8)、白細胞介素-10(IL-10)、腫瘤壞死因子-α(TNF-α)及C反應蛋白(CRP)水平,氧自由基清除指標包括血漿超氧化物歧化酶(SOD)、丙二醛(MDA)水平。
1.4 統計學處理 用統計學處理軟件SPSS 26.0對所得數據進行處理。計量資料中符合正態分布者用(x±s)表示,組間比較用獨立樣本t檢驗,組內比較用配對t檢驗;計數資料用例(%)表示,比較則用字2檢驗。P<0.05為差異有統計學意義。
2 結果
2.1 兩組一般資料比較 觀察組男33例,女27例;年齡6個月~5歲,平均(2.42±0.87)歲;體重6.32~18.78 kg,平均(12.20±3.51)kg;房間隔缺損17例,室間隔缺損43例。對照組男35例,女25例;年齡7個月~5歲,平均(2.72±0.95)歲;體重6.18~19.36 kg,平均(12.48±3.34)kg;房間隔缺損15例,室間隔缺損45例。兩組一般資料比較,差異均無統計學意義(P>0.05),具有可比性。
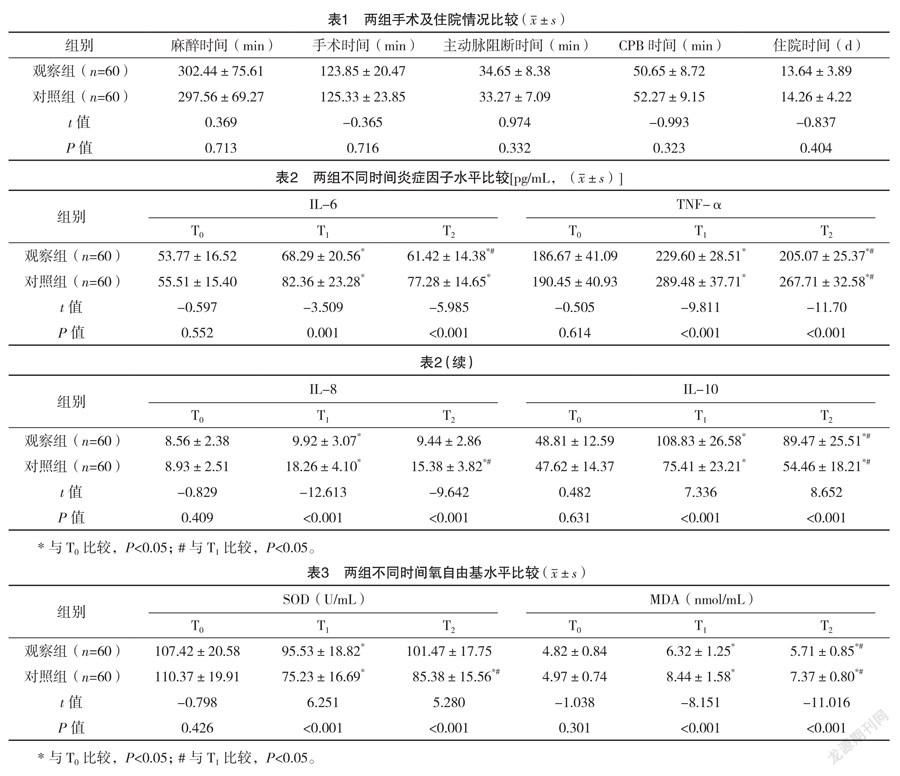
2.2 兩組手術及住院情況比較 兩組麻醉時間、手術時間、CPB時間、主動脈阻斷時間、住院時間比較,差異均無統計學意義(P>0.05),見表1。
2.3 兩組不同時間炎癥因子水平比較 兩組T0的IL-6、TNF-α、IL-8、IL-10比較,差異均無統計學意義(P>0.05);T1、T2,對照組IL-6、TNF-α、IL-8及觀察組IL-6、TNF-α均高于T0,且觀察組T1、T2的IL-6、TNF-α、IL-8均低于對照組,差異均有統計學意義(P<0.05);兩組T1、T2的IL-10均高于T0,且觀察組均高于對照組,差異均有統計學意義(P<0.05);觀察組T1的IL-8高于T0,差異有統計學意義(P<0.05);T2,兩組的IL-6、TNF-α、IL-10及對照組IL-8均低于T1,差異均有統計學意義(P<0.05)。見表2。
2.4 兩組不同時間氧自由基水平比較 T0,兩組SOD、MDA比較,差異均無統計學意義(P>0.05)。對照組T1、T2及觀察組T1的SOD均低于T0,觀察組T1、T2的SOD均高于對照組,差異均有統計學意義(P<0.05);兩組T1、T2的MDA均高于T0,且觀察組均低于對照組,差異均有統計學意義(P<0.05);T2,兩組MDA低于T1,對照組SOD高于T1,差異均有統計學意義(P<0.05)。見表3。
3 討論
在先天性心臟病患兒中,CPB在心臟手術期間維持組織的血液供應,并保護心肌組織免受缺血性損傷[9],然而,CPB與缺血/再灌注損傷有關,再灌注損傷是在缺血或缺氧一段時間后,當血液供應回到組織中時引起的組織損傷[10]。最近,體外和離體研究表明,氧化自由基的產生在心肌缺血-再灌注損傷中起著重要的病因學作用,嬰兒和新生兒可能有不成熟的抗氧化防御系統,因此更容易受到氧化劑應激的影響[11];在使用CPB進行心臟手術期間,心臟和肺部的血液供應暫時幾乎完全停止,這些器官內缺氧促使細胞積累代謝中間產物,細胞損傷誘導細胞表面黏附分子的上調和促炎細胞因子的表達[12];此外,在心臟外科手術中,不同的刺激,如血液暴露于CPB的非內皮表面及泵、人工肺、插管、抽吸和通氣回路對血細胞成分施加剪切應力,損傷紅細胞、白細胞和血小板,亦可能會引發炎癥反應[13-14]。體液和細胞級聯的激活導致循環血液中促炎細胞因子的增加和白細胞募集的增強[12],由此產生的SIRS與術后并發癥有關,包括心肌功能障礙、呼吸衰竭、急性腎損傷等。減少CPB患兒炎癥反應及氧化應激反應對機體恢復至關重要。
烏司他丁屬蛋白酶抑制劑,可清除氧自由基,穩定溶酶體膜,抑制炎癥物質,其常用于胰腺炎治療中[6,15]。其應用于心臟手術中,可減輕炎癥反應,并可明顯保護患者心肺功能[3,16-18]。本研究將其應用于室間隔或房間隔缺損患兒的CPB心臟手術中,其對麻醉時間、手術時間、CPB時間、主動脈阻斷時間、住院時間無明顯影響,但與對照組炎癥因子IL-6、TNF-α、IL-8、IL-10比較均明顯改善。CPB誘發促炎和抗炎細胞因子釋放的改變,在接受心臟手術的患者中,促炎細胞因子IL-6、TNF-α、IL-8水平的升高與不良臨床結果相關[12],TNF-α可促進多種炎癥因子釋放,在炎癥反應啟動觸發中發揮重要作用,IL-6在炎癥反應急性期升高,是炎癥反應敏感指標,IL-8是促進炎癥反應的典型介質,而IL-10則屬于抑炎因子,可保護機體免受炎癥反應損害[19],本研究結果證明烏司他丁可有效抑制促炎因子升高,上調抗炎介質的釋放。人體內SOD可有效地清除氧自由基,維持機體氧化與抗氧化平衡,在氧化應激反應中對細胞起到保護作用,自由基作用于脂質發生過氧化反應產生MDA,間接反應組織過氧化損傷程度,SOD與MDA結合分析有助于判斷機體脂質過氧化及缺血再灌注損傷的程度[20]。Sznycer-Taub等[11]研究表明CPB心臟手術可影響心肌氧化應激,本研究中使用烏司他丁的觀察組術后SOD、MDA更優,說明其有利于氧自由基清除,從而減少缺血再灌注損傷。
綜上所述,在患兒CPB心臟手術中,烏司他丁可有效抑制促炎因子升高,上調抗炎介質的釋放,促進氧自由基清除,從而減少機體損傷。
參考文獻
[1] STURMER D,BEATY C,CLINGAN S,et al.Recent innovations in perfusion and cardiopulmonary bypass for neonatal and infant cardiac surgery[J].Transl Pediatr,2018,7(2):139-150.
[2]謝柯祺,夏氫,羅繼文,等.烏司他丁對體外循環心臟手術后心肌損傷及缺血再灌注相關病理環節的影響[J].海南醫學院學報,2018,24(17),1578-1581,1586.
[3] PANG X Y,FANG C C,CHEN Y Y,et al.Effects of Ulinastatin on Perioperative Inflammatory Response and Pulmonary Function in Cardiopulmonary Bypass Patients[J/OL].Am J Ther,2016,23(6):e1680-e1689.
[4] HIRATA Y.Cardiopulmonary bypass for pediatric cardiac surgery[J].Gen Thorac Cardiovasc Surg,2018,66(2):65-70.
[5] SZNYCER-TAUB N,MACKIE S,PENG Y W,et al.Myocardial Oxidative Stress in Infants Undergoing Cardiac Surgery[J].Pediatr Cardiol,2016,37(4):746-750.
[6]張雪芹,徐曉林.烏司他丁對急性胰腺炎患者氧自由基清除能力及炎性應激的改善作用[J].昆明醫科大學學報,2017,38(8):90-93.
[7]梁麗俊,張麗芬.烏司他丁對法洛四聯癥根治術嬰幼兒炎性反應的影響和心肌保護作用[J].中國藥物與臨床,2016,16(8):1181-1183.
[8] PERMANYER E,MUNOZ-GUIJOSA C,PADRó J M,et al.Mini-extracorporeal circulation surgery produces less inflammation than off-pump coronary surgery[J].Eur J Cardiothorac Surg,2020,57(3):496-503.
[9] AZARFARIN R,DASHTI M,TOTONCHI Z,et al.Efficacy of the “head-up position” in returning cardiopulmonary bypass blood to the patient and reducing the required blood transfusion: a randomized tria[J].Iran Heart J,2017,18:6-15.
[10] SCHOFIELD Z V,WOODRUFF T M,HALAI R,et al.
Neutrophilsea key component of ischemia-reperfusion injury[J].Shock,2013,40(6):463-470.
[11] SZNYCER-TAUB N,MACKIE S,PENG Y W,et al.
Myocardial Oxidative Stress in Infants Undergoing Cardiac Surgery[J].Pediatr Cardiol,2016,37(4):746-750.
[12] KRAFT F,SCHMIDT C,VAN AKEN H,et al.Inflammatory response and extracorporeal circulation[J].Best Pract Res Clin Anaesthesiol,2015,29(2):113-123.
[13] HIRATA Y.Cardiopulmonary bypass for pediatric cardiac surgery[J].Gen Thorac Cardiovasc Surg,2018,66(2):65-70.
[14] HAPONIUK I,JAWORSKI R,PACZKOWSKI K,et al.
Postoperative kinetics of common inflammatory biomarkers after congenital heart defect procedures with extracorporeal circulation in children[J].Kardiol Pol,2018,76(6):968-973.
[15] ZHANG R,MA J,ZHENG P,et al.Ulinastatin plus biapenem for severe pneumonia in the elderly and its influence on pulmonary function and inflammatory cytokines[J].Am J Transl Res,2021,13(5):5027-5034.
[16]宗曉倩,金曉玲,馬鈺,等.烏司他丁預處理對心臟瓣膜置換患者心肌氧化應激損傷的保護作用[J/OL].中華臨床醫師雜志(電子版),2016,10(10):1437-1440.
[17]于浩,顏濤,馬濤,等.烏司他丁對復雜先天性心臟病患兒體外循環圍術期肺保護作用的研究[J].廣東醫學,2017,38(20):3184-3187.
[18]李慧蘊,楊志遠,謝周良,等.烏司他丁對體外循環下法洛四聯癥根治術患兒心肌損傷的影響[J].中華實驗外科雜志,2017,34(2):321-324.
[19] GORJIPOUR F,TOTONCHI Z,GHOLAMPOUR DEHAKI M,
et al.Serum levels of interleukin-6, interleukin-8, interleukin-10, and tumor necrosis factor-α, renal function biochemical parameters and clinical outcomes in pediatric cardiopulmonary bypass surgery[J].Perfusion,2019,34(8):651-659.
[20]董向陽,李文靜,翟波,等.烏司他丁在嬰幼兒體外循環手術中對氧自由基的影響[J].中國實用醫藥,2015,10(35):31-32.
(收稿日期:2021-09-30) (本文編輯:張爽)