經皮椎弓根內固定在無神經損傷胸腰椎骨折中的療效及對脊柱穩定性的影響
杜紹歡 陳萬安


【摘要】 目的:探究經皮椎弓根內固定在無神經損傷胸腰椎骨折中的療效及對脊柱穩定性的影響。方法:將2021年10月—2023年1月汕頭市澄海區人民醫院收治的82例無神經損傷胸腰椎骨折患者根據隨機數字表法分為對照組(n=41)和觀察組(n=41)。對照組進行開放椎弓根內固定治療,觀察組進行經皮椎弓根內固定治療。比較兩組優良率、手術時間、切口長度、術中出血量、住院時間、并發癥發生率,以及手術前后的疼痛程度[語言分級評分法(VRS)]和脊柱穩定性(傷椎前、后緣高度比、矢狀面指數及后凸Cobb角)。結果:兩組優良率比較,差異無統計學意義(P>0.05);觀察組的手術時間、住院時間及切口長度均顯著短于對照組,術中出血量顯著少于對照組,并發癥發生率顯著低于對照組,差異均有統計學意義(P<0.05);術前兩組VRS評分及脊柱穩定性指標比較,差異均無統計學意義(P>0.05);術后1、4、12周,觀察組的VRS評分均顯著低于對照組,差異均有統計學意義(P<0.05);兩組術后24周的VRS評分及術后12、24周的脊柱穩定性指標比較,差異均無統計學意義(P>0.05)。結論:經皮椎弓根內固定可減輕手術創傷,有效促進無神經損傷胸腰椎骨折患者的術后恢復,療效確切,對脊柱穩定性的效果與開放手術相近。
【關鍵詞】 經皮椎弓根內固定 胸腰椎骨折 脊柱穩定性
Effect of Percutaneous Vertebral Pedicle Internal Fixation on Thoracic and Lumbar Spine Fracture without Nerve Injury and Its Influence on Spinal Stability/DU Shaohuan, CHEN Wanan. //Medical Innovation of China, 2024, 21(07): 00-005
[Abstract] Objective: To investigate the effect of percutaneous vertebral pedicle internal fixation on thoracic and lumbar spine fracture without nerve injury and its influence on spinal stability. Method: A total of 82 patients with thoracic and lumbar spine fracture without nerve injury admitted to People's Hospital of Chenghai Shantou from October 2021 to January 2023 were divided into control group (n=41) and observation group (n=41) according to random number table method. The control group was treated with open vertebral pedicle internal fixation and the observation group was treated with percutaneous vertebral pedicle internal fixation. The excellent and good rate, operative time, incision length, intraoperative bleeding volume, hospital stay, complication rate and pain degree [verbal rating scale (VRS)] and spinal stability (anterior and posterior margin height ratio of injured vertebra, sagittal plane index and kyphotic Cobb angle) before and after surgery were compared between the two groups. Result: There was no significant difference in the excellent and good rate between the two groups (P>0.05). The operation time, hospital stay and incision length in the observation group were significantly shorter than those in the control group, the intraoperative bleeding volume was significantly less than that in the control group, and the incidence of complications was significantly lower than that in the control group, the differences were statistically significant (P<0.05). There were no significant differences in VRS scores and spinal stability indexes between the two groups before surgery (P>0.05). At 1 week and 4, 12 weeks after surgery, the VRS scores of observation group were significantly lower than those of control group, the differences were statistically significant (P<0.05). There were no significant differences between the two groups in VRS scores at 24 weeks after surgery and spinal stability indexes at 12 and 24 weeks after surgery (P>0.05). Conclusion: Percutaneous vertebral pedicle internal fixation can reduce surgical trauma and effectively promote postoperative recovery of patients with thoracic and lumbar spine fracture without nerve injury. The efficacy is accurate, and the effect on spinal stability is similar to that of open surgery.
[Key words] Percutaneous vertebral pedicle internal fixation Thoracic and lumbar spine fracture Spinal stability
First-author's address: Orthopaedic Center, People's Hospital of Chenghai Shantou, Shantou 515800, China
doi:10.3969/j.issn.1674-4985.2024.07.001
胸腰椎骨折是臨床中較為嚴重的骨折類型,其中無神經損傷的胸腰椎骨折,雖然治療難度相對更低,預后相對較好,但是其療效提升的需求仍較高,而治療后脊柱穩定性的提升,也是預后改善的重要基礎與前提[1-2]。既往臨床關于無神經損傷胸腰椎骨折的手術治療研究多見,其中椎弓根內固定是常用且效果較好的手術方式之一,而關于開放與經皮椎弓根內固定的比較性研究雖多見,但是其結果差異仍存在[3-5],同時上述手術方式對患者脊柱穩定性的研究不足。鑒于上述情況,本研究現探究經皮椎弓根內固定在無神經損傷胸腰椎骨折中的療效及對脊柱穩定性的影響,并報道如下。
1 資料與方法
1.1 一般資料
選擇2021年10月—2023年1月汕頭市澄海區人民醫院收治的82例無神經損傷胸腰椎骨折患者。納入標準:20~65歲;胸腰椎單節段骨折;無神經損傷;有效配合研究。排除標準:骨質疏松;既往胸腰椎骨折史;脊柱先天畸形;慢性疾病;病程≥1周;
多系統器官功能不全;溝通或認知障礙。根據隨機數字表法將患者分為對照組(n=41)和觀察組(n=41)。本次研究經本院醫學倫理學委員會批準。患者或家屬知情同意。
1.2 方法
對照組進行開放椎弓根內固定治療:常規術前檢查,患者于俯臥位下進行手術治療,全麻下,以骨折椎體為中心,做上下切口,充分暴露病灶,將椎弓根釘置入,將釘道擴大后,以椎弓根螺釘置入,接入連接桿,有效恢復創傷椎體的高度,然后進行縫合及術后抗感染。觀察組則進行經皮椎弓根內固定:常規術前檢查,于俯臥過伸位下進行治療,首先采用C臂機進行病灶椎體的確定,于體表進行投影,并于標記處將皮膚進行切開處理,于上下四個椎弓根處做四個切口,依次將皮膚、皮下組織及深筋膜切開,然后將椎旁肌分離,于透視指導下將穿刺針從外側緣進行穿刺,置入椎弓根螺釘,連接棒置入及復位,固定后進行縫合及其他處理。
1.3 觀察指標及判定標準
比較兩組的優良率、手術時間、切口長度、術中出血量、住院時間、并發癥發生率,以及手術前后的疼痛程度[語言分級評分法(VRS)]和脊柱穩定性(前、后緣高度比、矢狀面指數及后凸Cobb角)。(1)治療效果:術后24周,胸腰椎骨折相關癥狀體征全部消失,對工作生活無影響為優;胸腰椎骨折相關癥狀輕微,對工作生活無影響為良;胸腰椎骨折相關癥狀有明顯改善,對工作生活影響較小為可;未達到可即為差[6]。優良率=(優+良)例數/總例數×100%。(2)并發癥發生情況:統計兩組感染、內固定移位、傷口紅腫等并發癥發生率,并計算其總發生率。(3)疼痛程度:于術前及術后1、4、12、24周分別采用VRS評估,根據患者主訴進行疼痛評估,其評分范圍為0~5分,評分越高表示疼痛感越強[7]。(4)脊柱穩定性:于術前及術后12、24周分別采用X平片進行脊柱穩定性的檢測,檢測及統計項目為傷椎前、后緣高度比、矢狀面指數及后凸Cobb角。
1.4 統計學處理
本研究中的數據檢驗選用軟件SPSS 23.0。計數資料的表達方式為率(%),比較方式為字2檢驗;計量資料的表達方式為(x±s),比較方式為t檢驗(組間用獨立樣本t檢驗,組內用配對t檢驗)。P<0.05為差異有統計學意義。
2 結果
2.1 兩組基線資料比較
對照組男22例,女19例;年齡22~63歲,平均(47.36±10.36)歲;骨折至手術時間1.0~3.9 d,平均(2.11±0.63)d;骨折部位:T11 5例,T12 15例,L1 15例,L2 6例;致傷原因:車禍21例,墜落15例,其他5例。觀察組男23例,女18例;年齡21~64歲,平均(47.63±10.19)歲;骨折至手術時間1.0~4.5 d,平均(2.09±0.59)d;骨折部位:T11 5例,T12 15例,L1 16例,L2 5例;致傷原因:車禍20例,墜落15例,其他6例。兩組無神經損傷胸腰椎骨折患者的性別、年齡、骨折至手術時間、骨折部位及致傷原因比較,差異均無統計學意義(P>0.05),具有可比性。
2.2 兩組優良率比較
兩組優良率比較,差異無統計學意義(字2=0.156,P=0.692),見表1。
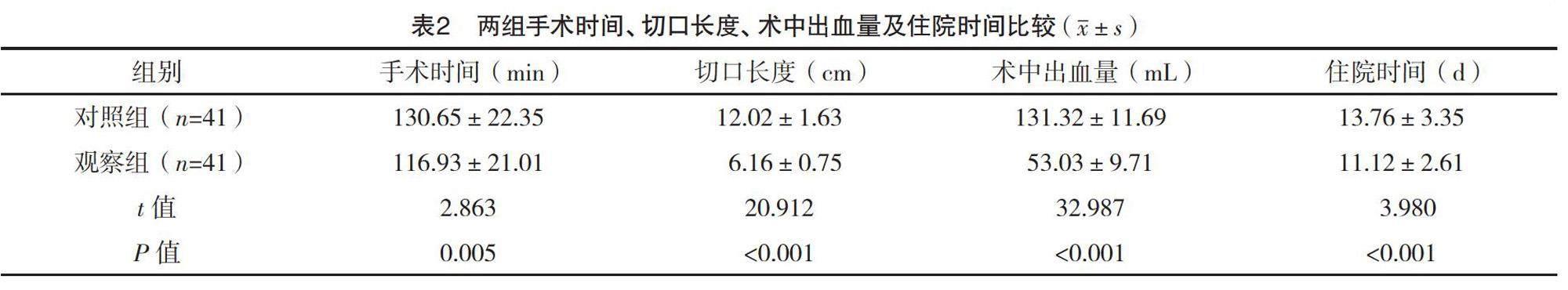
2.3 兩組手術時間、切口長度、術中出血量及住院時間比較
觀察組的手術時間、住院時間及切口長度均顯著短于對照組,術中出血量顯著少于對照組,差異均有統計學意義(P<0.05),見表2。
2.4 兩組并發癥發生情況比較
觀察組的并發癥發生率顯著低于對照組,差異有統計學意義(字2=4.493,P=0.034),見表3。
2.5 兩組手術前后VRS評分比較
術前兩組VRS評分比較,差異無統計學意義(P>0.05);術后1、4、12周,觀察組的VRS評分均顯著低于對照組,差異均有統計學意義(P<0.05);兩組術后24周的VRS評分比較,差異無統計學意義(P>0.05)。見表4。
2.6 兩組手術前后脊柱穩定性比較
術前及術后12、24周,兩組脊柱穩定性指標比較,差異均無統計學意義(P>0.05);兩組術后12、24周的傷椎前、后緣高度比及矢狀面指數均顯著高于術前,后凸Cobb角均顯著低于術前,差異均有統計學意義(P<0.05)。見表5。
3 討論
胸腰椎骨折不僅可導致局部的疼痛,還會對脊柱功能造成嚴重損傷,而無神經損傷的患者,雖無神經損傷相關的癥狀體征,也基本不會出現癱瘓,但是其對治療后脊柱穩定性的要求仍較高,這關系到后期的功能恢復、不適感控制及綜合生活質量[8-9]。與脊柱穩定性相關的指標較多,其中,前、后緣高度比、矢狀面指數及后凸Cobb角的改善情況與胸腰椎骨折的治療效果密切相關,可作為脊柱損傷程度及術后恢復的重要參考依據[10-12]。既往多采用開放椎弓根內固定治療無神經損傷胸腰椎骨折,而隨著醫學技術的發展及臨床對治療微創要求的提升,經皮椎弓根內固定在無神經損傷胸腰椎骨折患者中的應用研究不斷增多,其可達到與開放式手術相似的效果[13-15]。也有研究顯示,經皮椎弓根內固定因可更有效的控制手術創傷,故更有助于促進患者的術后恢復[16-17]。
本研究結果顯示,經皮椎弓根內固定在無神經損傷胸腰椎骨折中的優良率與開放式手術無明顯差異,但其手術時間、住院時間、切口長度均更短,術中出血量更少,并發癥發生率更低,且術后12周內的VRS評分均更低,說明其不僅可保證手術效果,還可減輕手術對患者造成的應激創傷,促進術后康復。分析原因,經皮椎弓根內固定的手術創傷相對更小,所致手術部位的組織損傷更小,且手術時間也較短,而這均為其術后的盡快康復提供了必要的前提[18-20]。此外,兩組患者術后的脊柱穩定性指標改善均較為明顯,但兩組比較并無統計學意義,表明此手術方式保證了患者術后較長時間的脊柱穩定性,而這也進一步肯定了經皮椎弓根內固定的臨床應用效果。
綜上所述,經皮椎弓根內固定可促進無神經損傷胸腰椎骨折患者的術后康復,療效確切,對脊柱穩定性的效果與開放手術相近。
參考文獻
[1]賴宇銳,倪增良,樂麗娜,等.經皮椎弓根螺釘治療無神經損傷胸腰椎骨折與傳統術式的療效及安全性對比研究[J].中國保健營養,2020,30(17):36-37.
[2]周建鋒.微創小切口聯合經皮椎弓根螺釘復位內固定治療胸腰椎骨折伴神經損害的效果觀察[J].醫藥前沿,2020,10(17):106-108.
[3]紀玉清,吳玉仙,袁百勝,等.經皮椎弓根釘內固定聯合傷椎置釘治療無神經癥狀Magerl A3型胸腰椎爆裂骨折[J].中國骨與關節損傷雜志,2020,35(7):706-708.
[4]盧鎮生,葉握球,馮奕鑫,等.微創經皮椎弓根螺釘內固定與開放手術治療非神經損傷胸腰椎骨折的臨床療效比較[J].吉林醫學,2022,43(10):2611-2615.
[5]盧成.經皮椎弓根釘聯合壯骨湯在胸腰椎骨折患者術后早期康復中的療效觀察[J].頸腰痛雜志,2023,44(1):57-63.
[6]屈錫亮,黃雄飛,葉永勝,等.后路椎弓根釘系統固定結合傷椎植入注射用人工骨治療胸腰椎爆裂骨折的臨床研究[J].中國實用醫藥,2020,15(29):101-103.
[7]李春蕊,張雯,樊碧發.數字評分法(NRS)與口述評分法(VRS)在老年慢性疼痛患者中的比較[J].中國疼痛醫學雜志,2016,22(9):683-686.
[8]楊名,趙祥,丁浩,等.經皮與開放椎弓根釘內固定治療胸腰椎骨折的療效比較[J].中國骨與關節損傷雜志,2021,36(11):1162-1164.
[9] KOCIS J,KELBL M,KOCIS T,et al.Percutaneous versus open pedicle screw fixation for treatment of type A thoracolumbar fractures[J]. Eur J Trauma Emerg Surg,2020,46(1):147-152.
[10]格日勒,楊鵬,劉鑫,等.無神經癥狀的胸腰椎骨折中O型臂導航下與傳統經皮椎弓根置釘效果比較[J].中華醫學雜志,2020,100(39):3099-3103.
[11] LU Q,KANG H,XIONG C,et al.Percutaneous uniplanar pedicle screw-rod system with injured vertebra fixation for thoracolumbar burst fracture and technique notes[J].J Coll Physicians Surg Pak,2022,32(10):1295-1299.
[12]司正濤,趙紫財.Sextant微創經皮椎弓根螺釘內固定術與開放式椎弓根內固定術治療胸腰椎多發脊柱骨折的療效觀察[J]. 海南醫學,2021,32(6):727-730.
[13]孫奎,劉永皚,徐耀寧,等.四維牽引法聯合經皮椎弓根釘內固定治療無神經損傷胸腰椎骨折[J].中國骨與關節損傷雜志,2021,36(3):268-269.
[14]吳林清,陳運崇,陳宏帥,等.經皮椎弓根釘內固定與開放椎弓根釘內固定治療無神經損傷胸腰椎骨折的療效比較[J].中國骨與關節損傷雜志,2023,38(3):270-272.
[15]周世強,曹銳,程亞鋒,等.經皮椎弓根釘內固定對老年無神經損傷胸腰椎骨折患者的臨床療效及生活質量的影響[J].中國醫師雜志,2020,22(2):301-303.
[16] TRUNGU S,RICCIARDI L,FORCATO S,et al.Percutaneous pedicle screw fixation without arthrodesis of 368 thoracolumbar fractures: long-term clinical and radiological outcomes in a single institution[J].Eur Spine J,2023,32(1):75-83.
[17]李廣偉,白忠旭,王亞輝,等.微創經皮椎弓根螺釘內固定術治療無神經損傷胸腰椎骨折的臨床觀察[J].中國現代醫藥雜志,2021,23(3):49-51.
[18]黃子彥,常杰,武朝欽,等.兩種微創手術方式治療胸腰椎骨折的療效比較[J].中華實驗外科雜志,2022,39(1):158-161.
[19] ZHANG Y,WANG W,BAI L,et al.A comparison of outcomes between the Wiltse approach with pedicle screw fixation and the percutaneous pedicle screw fixation for multi-segmental thoracolumbar fractures[J].Orthop Surg,2023,15(9):2363-2372.
[20]尹志平,葉樹強,羅濤,等.經皮椎弓根螺釘內固定術治療無神經損傷性胸腰椎椎體骨折的價值[J].中國醫療器械信息,2022,28(10):66-68.
(收稿日期:2024-01-25) (本文編輯:陳韻)