尿源性膿毒血癥診治分析
韋能寶 薛志剛 畢金文
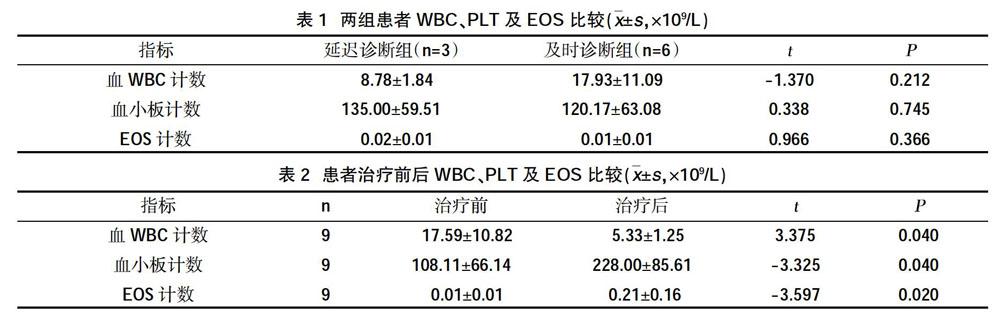
摘 ? 要:目的 ?總結(jié)尿源性膿毒血癥的診治經(jīng)驗,提高對尿源性膿毒血癥的認(rèn)識。方法 ?回顧性分析北京懷柔醫(yī)院2017年3月~2018年8月臨床確診的9例尿源性膿毒血癥患者的臨床資料,按照就診是否及時分為及時診斷組、延遲診斷組,觀察兩組患者血白細(xì)胞、血嗜酸性粒細(xì)胞、血小板、血乳酸及降鈣素原變化情況。結(jié)果 ?9例患者中,女性7例(77.78%),男性2例(22.22%);>60歲的6例(66.67%);3例(33.33%)患者合并有糖尿病,且血糖控制不佳,其中2例患者同時合并有糖尿病及慢性腎功能不全;均有發(fā)熱癥狀,2例在確診時血WBC下降,7例血WBC升高。3例患者出現(xiàn)診斷延遲,6例診斷及時。延遲診斷組患者就診時均未行PCT檢查,2例查血乳酸升高,未引起臨床重視;與治療前比較,患者WBC水平降低,EOS及血小板水平升高,差異有統(tǒng)計學(xué)意義(P<0.05)。4例尿培養(yǎng)陽性(陽性率44.44%),其中3例為大腸埃希菌,1例為肺炎克雷伯桿菌。經(jīng)積極治療,所有患者均好轉(zhuǎn)出院,未出現(xiàn)死亡病例。結(jié)論 ?老年女性合并有糖尿病或慢性腎功能不全是尿源性膿毒血癥的高危因素;對于出現(xiàn)高熱或低體溫血WBC未見明顯升高或降低患者,需完善PCT及血乳酸檢查,EOS、乳酸及PCT值對早期診斷有一定價值;尿源膿毒血癥進(jìn)展迅速,需綜合治療,甚至需多科室協(xié)作,避免出現(xiàn)不良并發(fā)癥。
關(guān)鍵詞:尿源性膿毒血癥;白細(xì)胞;血嗜酸性粒細(xì)胞;糖尿病;腎功能不全
中圖分類號:R691.4 ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ?文獻(xiàn)標(biāo)識碼:B ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ?DOI:10.3969/j.issn.1006-1959.2018.24.052
文章編號:1006-1959(2018)24-0170-03
Abstract:bjective ?To summarize the experience of diagnosis and treatment of urinary sepsis and improve the understanding of urinary sepsis. Methods ?The clinical data of 9 patients with urinary sepsis who were clinically diagnosed from March 2017 to August 2018 in Beijing Huairou Hospital were retrospectively analyzed. According to the timely treatment, the patients were divided into timely diagnosis group and delayed diagnosis group. Changes in blood leukocytes, blood eosinophils, platelets, blood lactate, and procalcitonin in patients. Results ?Of the 9 patients, 7 (77.78%) were female, 2 (22.22%) were male; 6 (66.67%) were >60 years old; 3 (33.33%) patients had diabetes and poor glycemic control. 2 of the patients had diabetes and chronic renal insufficiency at the same time; all had fever symptoms, 2 patients had decreased blood WBC at the time of diagnosis, and 7 patients had elevated blood WBC. Three patients had a delayed diagnosis and six were diagnosed promptly. Patients in the delayed diagnosis group did not undergo PCT examination at the time of treatment, and 2 patients had elevated blood lactate levels, which did not cause clinical attention. Compared with before treatment, patients' WBC levels decreased, EOS and platelet levels increased,the difference was statistically significant (P<0.05). 4 cases were positive for urine culture (positive rate 44.44%), of which 3 cases were Escherichia coli and 1 case was Klebsiella pneumoniae. After active treatment, all patients were discharged and no deaths occurred. Conclusion ?Older women with diabetes or chronic renal insufficiency are risk factors for urinary sepsis. For patients with high fever or hypothermia without significant increase or decrease in WBC, PCT and blood lactate tests, EOS, should be improved. Lactic acid and PCT valueshave certain value for early diagnosis; urinary sepsis is rapidly progressing, requiring comprehensive treatment, and even multi-disciplinary collaboration is needed to avoid adverse complications.
Key words:Urinary sepsis;White blood cells;Blood eosinophils;Diabetes;Renal insufficiency
尿源性膿毒血癥(urogenic sepsis)是指尿路感染出現(xiàn)臨床感染癥狀并且伴有全身炎癥反應(yīng)征象,其本質(zhì)是機(jī)體對感染性因素的應(yīng)激反應(yīng)[1]。尿源性膿毒血癥分為三個階段:第一階段為全身炎癥反應(yīng)綜合征(systematic inflammatory response syndrome,SIRS),第二階段為膿毒血癥(sepsis),第三階段為感染性休克(septic shock)[2]。該病起病急、進(jìn)展快、病情危重,部分患者甚至在就診前已經(jīng)出現(xiàn)SIRS,如得不到及時診斷和治療,可進(jìn)一步進(jìn)展為感染性休克,甚至多器官功能障礙,病情會迅速失控、惡化,重癥病死率高達(dá)22%~76%[3]。有學(xué)者認(rèn)為,診斷延遲是導(dǎo)致尿源性膿毒血癥病死率高的主要原因之一,診斷每延遲1 h,病死率可能上升8%[4]。為……

