孕婦肥胖與剖宮產術中、術后并發癥發生的關系
張娜 杜慧
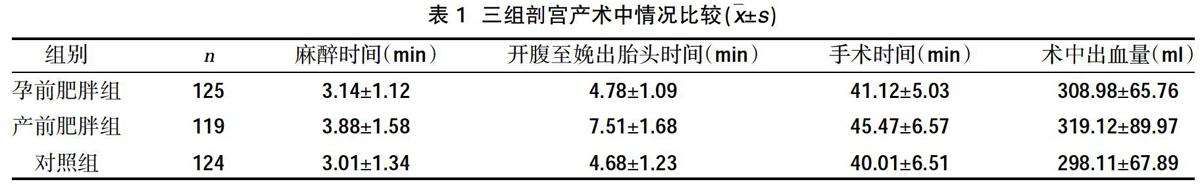
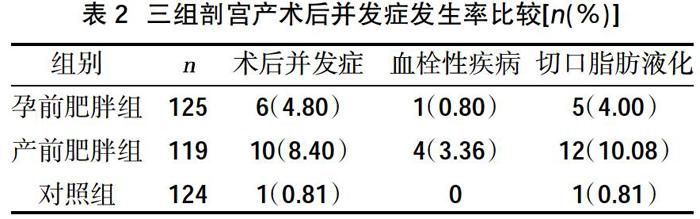

摘要:目的 ?分析孕婦肥胖與剖宮產術中、術后并發癥的關系,以期為剖宮產并發癥的防治工作提供參考依據。方法 ?選擇2018年5月~2019年5月我院收治的足月行剖宮產分娩的孕婦368例作為研究對象,按照體重指數(BMI)分為三組,將孕前BMI≥25 kg/m2的125例設為孕前肥胖組,將分娩前BMI>28 kg/m2的119例設為產前肥胖組,另將孕前BMI為17~24 kg/m2的124例設為正常對照組。比較三組麻醉時間、手術時間、開腹至娩出胎頭時間、術中出血量、術后傷口愈合情況、住院時間以及切口脂肪液化發生率。結果 ?孕前肥胖組麻醉時間、開腹至娩出胎頭時間、手術時間均較正常對照組時間稍延長,但差異無統計學意義(P>0.05);產前肥胖組麻醉時間、開腹至娩出胎頭時間、手術時間均較正常對照組時間延長,術后并發癥、血栓性疾病發生率、腹壁切口脂肪液化發生率高于對照組(P<0.05);孕、產前肥胖組術中出血量較正常對照組增多,血栓性疾病發生率高于對照組,差異無統計學意義(P>0.05);孕前肥胖組術后孕婦術后并發癥、切口脂肪液化發生率高于對照組(P<0.05);孕、產前肥胖組術后住院時間均長于對照組(P<0.05)。結論 ?孕婦孕前肥胖、產前肥胖均會延長剖宮產麻醉、手術時間,增加術后發病率,在今后的臨床工作中應給予重視,積極采取有效應對措施,加強宣教,控制孕期體重,降低剖宮產率,減少母嬰并發癥,改善妊娠結局。
關鍵詞:孕婦肥胖;剖宮產;并發癥
中圖分類號:R719.8 ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? 文獻標識碼:A ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? DOI:10.3969/j.issn.1006-1959.2020.18.026
文章編號:1006-1959(2020)18-0085-02
Relationship Between Obesity of Pregnant Women and Complications During and
After Cesarean Section
ZHANG Na,DU Hui
(Department of Obstetrics,Hubei Provincial Maternity and Child Health Hospital,Wuhan 430071,Hubei,China)
Abstract:Objective ?To analyze the relationship between obesity of pregnant women and complications during and after cesarean section, in order to provide a reference for the prevention and treatment of cesarean section complications.Methods ?From May 2018 to May 2019, 368 pregnant women undergoing cesarean section were selected as the research objects. They were divided into three groups according to the body mass index (BMI). The pre-pregnancy BMI ≥25 kg/m2 125 cases were set as pre-pregnancy obesity group, 119 cases with BMI>28 kg/m2 before childbirth were set as antenatal obesity group, and 124 cases with BMI before pregnancy 17-24 kg/m2 were set as normal control group. The anesthesia time, operation time, time from laparotomy to delivery of the fetal head, intraoperative blood loss, postoperative wound healing, hospitalization time, and incidence of incision fat liquefaction were compared among the three groups. Results ?The pre-pregnancy obesity group anesthesia time, the time from laparotomy to delivery of the fetal head, and the operation time were slightly longer than the normal control group time, but the difference was not statistically significant (P>0.05); the prenatal obesity group anesthesia time, the time from laparotomy to delivery of the fetal head the time and operation time were longer than those in the normal control group. The incidence of postoperative complications, thrombotic diseases, and fat liquefaction of abdominal wall incision were higher than those of the control group (P<0.05); the intraoperative bleeding was higher in the pregnant and prenatal obesity groups The normal control group increased, and the incidence of thrombotic diseases was higher than that of the control group, the difference was not statistically significant (P>0.05); the incidence of postoperative complications and incision fat liquefaction in the pre-pregnancy obesity group was higher than that of the control group (P<0.05); the postoperative hospital stay in the pregnancy and prenatal obesity group was longer than that in the control group (P<0.05).Conclusion ?Pre-pregnancy obesity and prenatal obesity would prolong the anesthesia and operation time of cesarean section and increase the postoperative morbidity. In future clinical work, attention should be paid to actively adopt effective countermeasures, strengthen publicity and education, control weight during pregnancy, and reduce cesarean section. Uterine birth rate, reduce maternal and infant complications, and improve pregnancy outcome.
Key words:Obesity of pregnant women;Cesarean section;Complications
剖宮產是解決難產、高危妊娠的一種有效措施。近年來剖宮產率逐年上升,一定程度上增加母嬰風險,對母嬰安全構成一定的威脅。隨著人們生活水平的提高,營養失衡現象也日益嚴峻,有調查顯示[1],我國約有70%以上孕婦出現孕期體重超標現象,而孕期孕婦體重超重會對妊娠結局、分娩方式造成一定程度影響。因此預防高危妊娠,降低剖宮產率是目前需要亟待解決問題。本研究比較了孕前肥胖、產前肥胖以及正常體重孕婦剖宮產術中、術后并發癥發生情況,以期為臨床預防及診治提供參考,現將結果報道如下。