伴有CEBPA雙位點突變的急性髓系白血病臨床特征及預后分析
章俏雷 江錦紅 劉永華 王曉麗 江妤 葉琇錦 方炳木
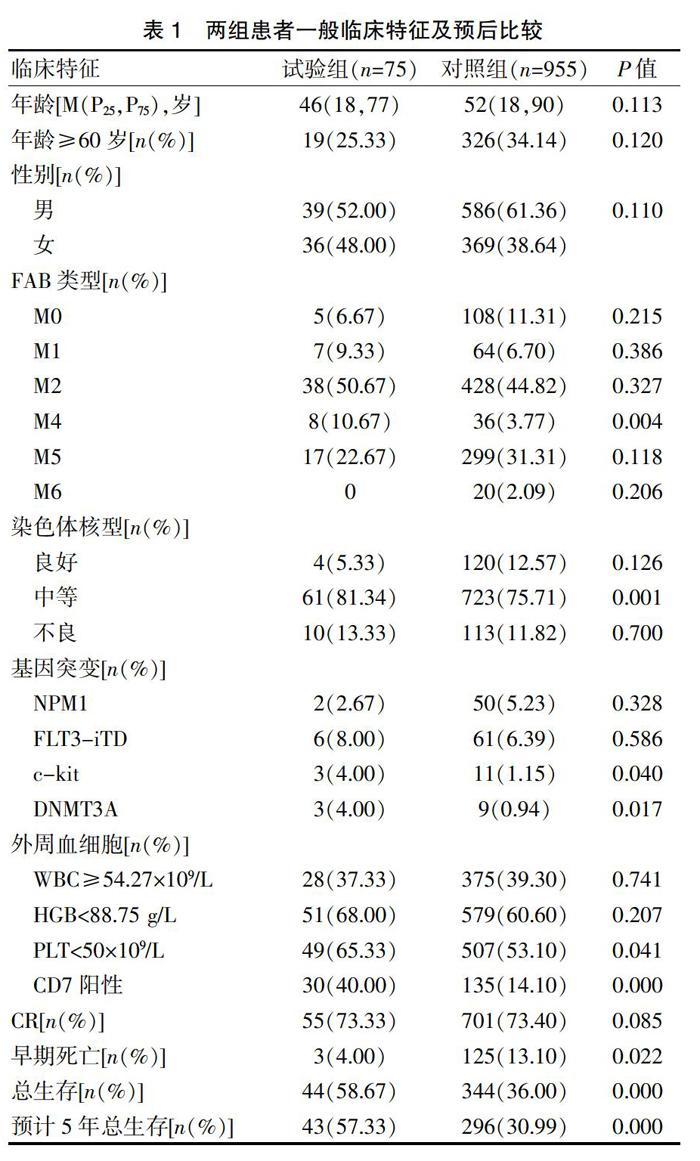

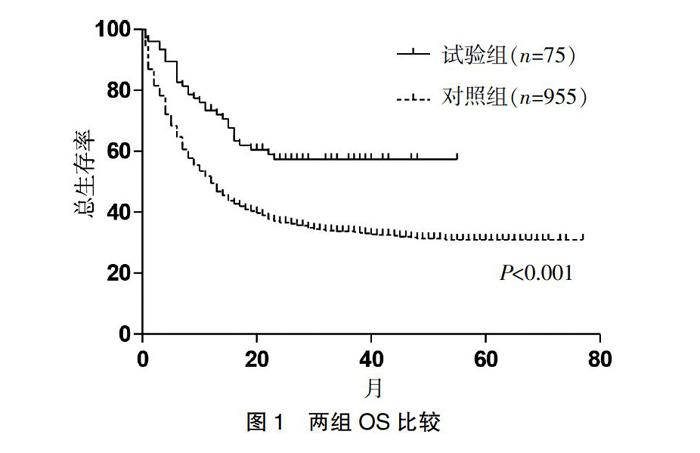
[摘要] 目的 分析伴有CEBPA雙位點突變的急性髓系白血病(AML)的臨床特征及預后。 方法 回顧性分析2013年1月至2019年5月浙江大學醫學院附屬第一醫院及麗水市人民醫院血液科連續收治的AML(非M3)患者1030例,其中CEBPA雙位點突變AML共75例為試驗組,非CEBPA雙位點突變AML共955例為對照組。比較兩組患者的臨床特征及預后差異。 結果 試驗組AML患者FAB分型中M4比例明顯高于對照組(P=0.004);試驗組初診PLT水平低于對照組(P=0.041);試驗組預后中等染色體核型比例明顯高于對照組(P=0.001);試驗組CD7抗原陽性比例明顯高于對照組(P<0.001);試驗組患者早期死亡率為4.00%,低于對照組患者的13.10%(P=0.022),其預計5年總生存(OS)率明顯高于對照組(57.33% vs. 30.99%,P<0.001);試驗組中多因素分析顯示,年齡≥60歲、HGB<88.75 g/L和不良染色體核型是預后不良的獨立危險因素。 結論 試驗組AML患者因有較低的早期死亡率,其預后明顯優于對照組患者;年齡≥60歲、HGB<88.75 g/L和不良染色體核型是CEBPA雙位點突變AML患者預后不良的獨立危險因素。
[關鍵詞] CEBPA雙位點突變;急性髓系白血病;臨床特征;預后
[中圖分類號] R733.7 ? ? ? ? ?[文獻標識碼] B ? ? ? ? ?[文章編號] 1673-9701(2021)04-0042-04
Clinical features and prognostic analysis of acute myeloid leukemia with double CEBPA mutations
ZHANG Qiaolei1 ? JIANG Jinhong1 ? LIU Yonghua1 ? WANG Xiaoli1 ? JIANG Yu1 ? YE Xiujin2 ? FANG Bingmu1
1.The Sixth Hospital Affiliated to Wenzhou Medical University, Lishui Municipal People′s Hospital in Zhejiang Province, Lishui ? 323000, China; 2.The First Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou ? 310003,China
[Abstract] Objective To analyze the clinical features and prognosis of acute myeloid leukemia(AML) with double CEBPA mutations. Methods A retrospective analysis was made on 1030 consecutive AML(non-M3) patients admitted to the First Affiliated Hospital of Zhejiang University School of Medicine and the hematology department of Lishui Municipal People′s Hospital from January 2013 to May 2019, of which CEBPA double-site mutant AML(n=75) were the experimental group and non-CEBPA double-site mutant AML(n=955) were the control group. The clinical features and prognostic analysis of the two groups were compared. Results The proportion of M4 in FAB typing of AML patients in the experimental group was significantly higher than that in the control group(P=0.004). The PLT level in the experimental group was lower than that in the control group(P=0.041). The proportion of moderate chromosome karyotype in the experimental group was significantly higher than that in the control group(P=0.001). The positive rate of CD7 antigen in the experimental group was significantly higher than that in the control group(P<0.001). The early mortality rate of the patients in the experimental group was 4.00%, which was lower than that of the control group (13.10%) (P=0.022), and its estimated 5-year overall survival (OS) rate was significantly higher than that of the control group (57.33% vs 30.99%, P<0.001). Multivariate analysis in the experimental group showed that age ≥60 years old, HGB<88.75 g/L and poor karyotype were independent risk factors for poor prognosis. Conclusion The prognosis of AML patients in the experimental group is obviously better than that in the control group due to their lower early mortality rate. Age≥60 years old, HGB<88.75 g/L and poor chromosome karyotype are independent risk factors for poor prognosis of CEBPA double site mutant AML patients.
[Key words] Double CEBPA mutations; Acute myeloid leukemia; Clinical features; Prognosis
急性髓系白血病(Acute myeloid leukemia,AML)是一組高度異質性血液系統惡性腫瘤[1-5]。核型異常是AML—個重要的預后標志。盡管如此,約有50%的AML患者缺少特征性的染色體標志物,而這些患者對治療的反應具有很大的差異[6]。AML患者伴CEBPA基因突變是AML中很大的一個亞型,占AML患者的10%~25%[7-9]。CEBPA基因定位于染色體19q13.1,cDNA全長2385 bp。CEBPA蛋白是維持造血系統粒系分化的重要轉錄因子,在調節細胞增殖與分化的平衡中起著關鍵的作用。CEBPA基因突變可分為單突變和雙突變這兩大類型,CEBPA基因雙突變是AML患者預后良好的分子標志[10-12]。國內絕大多數有關AML患者CEBPA基因突變研究樣本量均較小且無長期預后數據[13-14]。為此,本研究回顧性分析了1030例初診AML(非APL)患者的臨床資料,以探討初診CEBPA基因雙突變AML患者的臨床特征及預后,現報道如下。
1 資料與方法
1.1 一般資料
2013年1月至2019年5月浙江大學醫學院附屬第一醫院及麗水市人民醫院血液科共收治1030例初診AML(非APL)患者。診斷均符合WHO(2001)MICM分型診斷標準。CEBPA基因雙突變患者為試驗組,CEBPA基因單突變或無突變患者為對照組。
1.2 方法
1.2.1 免疫表型、細胞遺傳學及分子生物學檢查 ?采用美國貝克曼庫爾特公司EPICS-XL型流式細胞儀采集數據。采用直接法和(或)短期培養法常規制備染色體標本,按照《人類細胞遺傳學國際命名體制(ISCN 2009)》進行染色體核型分析。采用聚合酶鏈反應(PCR)擴增產物片段長度分析及序列分析方法進行相關基因突變檢測。
1.2.2 治療方案 ?誘導方案包括:大部分患者采用IA方案(去甲氧基柔紅霉素+阿糖胞苷)或HA方案(高三尖杉酯堿+阿糖胞苷),部分老年患者采用CAG方案(G-csf+阿糖胞苷+阿克拉霉素);獲得CR患者繼續原方案鞏固治療1療程,而后行大劑量或中劑量阿糖胞苷鞏固治療3~4 療程,少部分患者亦行DA或MA等方案鞏固治療。
1.2.3 誘導治療期間支持治療 ?每天檢測凝血功能、血常規,每周檢查2次生化常規。酌情輸注成份血。
1.3 觀察指標
所有病例根據FAB標準確診,對于是否緩解的評價在2個足量聯合化療療程后進行;早期死亡為確診后2周內經化療或未經化療的死亡;總生存(OS)時間為從疾病確診起至患者任何原因的死亡或隨訪截止日期[15]。隨訪時間截止于2019年5月。
1.4 統計學處理
采用SPSS 19.0統計學軟件進行數據分析。兩組間率的比較采用χ2檢驗和Fisher確切概率檢驗,單因素分析P<0.05的因素納入Logistic模型進行多因素分析。OS采用Kaplan-Meier法分析并進行Log-rank檢驗。P<0.05為差異有統計學意義。
2 結果
2.1 兩組患者一般臨床特征及預后比較
試驗組患者75例(7.28%),對照組患者955例,兩組性別比較,差異無統計學意義(P>0.05)。試驗組FAB分型最多見的是M2(50.67%);與對照組患者比較,試驗組患者初診時具有M4比例低(P=0.004)、PLT水平低(P=0.041)、CD7抗原表達比例高(P<0.001)、預后中等核型比例高(P=0.001)、c-kit陽性比例高(P=0.040)、DNMT3A陽性比例高(P=0.017);而兩組年齡、WBC、HGB指標比較,差異均無統計學意義(P>0.05)。見表1。
2.2 治療反應
試驗組完全緩解(CR)率與對照組CR率比較,差異無統計學意義(P>0.05)。見表1。
2.3 生存分析
1030例AML患者中位隨訪25(0~76)個月。至誘導治療結束共有128例發生早期死亡,試驗組早期死亡率低于對照組[3(4.00) vs. 125(13.10),P=0.022];至隨訪截止,44例試驗組患者存活,明顯高于對照組[44(58.67) vs. 344(36.00)],差異有統計學意義(P<0.001)。Kaplan-Meier生存分析顯示預計5年總生存(OS)率,試驗組明顯高于對照組[43(57.33) vs. 296(30.99)],差異有統計學意義(P<0.001)。見表1及圖1。
2.4 試驗組相關預后因素
分析比較試驗組患者診斷時的疾病特征(年齡、WBC、HGB、骨髓原始細胞數、CD7、FLT3-iTD、NPM1、染色體核型)與預后的關系,結果顯示,年齡≥60歲(OR=3.256,95%CI 1.419~7.471,P=0.005)、初診HGB<88.75 g/L(OR=5.416,95%CI 2.182~13.438,P=0.001)及不良染色體核型(OR=2.180,95%CI 1.142~4.164,P=0.018)為試驗組患者預后不良的獨立危險因素。見表2。
3 討論
急性髓系白血病是一組異質性的疾病,精細的分層對提高治療療效具有十分重要的作用。從分子學角度分析AML伴CEBPA雙位點突變被認為是低危組[10-12]。關于CEBPA基因雙突變的AML患者的臨床特點及相關預后研究,目前國內尚無大宗病例報道。本研究試圖探討伴CEBPA雙位點突變AML患者的臨床特征及預后因素,以探索臨床個體化治療策略,進一步提高該類患者的長期生存率。
本研究中CEBPA基因雙突變陽性率為7.28%,與相關報道相近[9,16-18],低于其他報道的22.0%~25.6%[9,19]。有研究發現,CEBPA雙突變多集中在FAB的M1和M2型[20-21],患者年齡較年輕[20,22-23],血小板計數較低[17,22,24]。本研究結果顯示,試驗組患者多集中在M2、M5型,中位年齡低于對照組,血小板計數較低。
CEBPA基因突變患者有獨特的免疫表型,其CD7、CD15、CD34、CD65高表達[23-25]。在本研究中,試驗組CD7抗原陽性比例明顯高于對照組(P<0.001)。CD7抗原為一單鏈糖蛋白,與AML不良的預后結果相關[26-28]。但在多因素分析中,發現CD7抗原表達并不是CEBPA雙突變AML患者的獨立預后危險因素。
有研究發現,在CEBPA雙突變的患者中很少發生NPM1突變和FLT3-ITD突變[23]。國內吳繼穎等[17]研究6例CEBPA基因突變AML患者,其中3例CEBPA雙突變的患者有1例合并FLT3-ITD突變。國外也有研究者發現在CEBPA雙突變的患者中幾乎不發生FLT3-ITD突變[23]。本研究結果顯示,試驗組患者中僅2例合并NPM1突變,6例合并FLT3-ITD突變。本研究認為國內外的這種不同可能是人種差異造成的。
CEBPA的突變主要集中在正常核型及9q-的AML患者中[23-24,29-30]。本研究中,試驗組預后中等核型比例明顯高于對照組(P=0.001),而預后中等核型中大部分是正常核型。值得注意的是,許多文獻證實CEBPA基因突變幾乎不發生在伴t(8;21)、inv(16)和t(15;17)這些預后相對較好的AML患者中[20-21]。另外,除正常核型和9q-患者外,CEBPA基因突變患者還可以出現inv(16)(p13;q22)、+13、+8、+21、11q23等染色體異常及復雜核型[14,28],本研究也證實了這一點。
國外研究報道,CEBPA雙突變AML患者CR率達到90%~92%[20,22]。本研究顯實,試驗組CR率為73.33%,與對照組相比差異無統計學意義。推測國內AML患者CR率較國外報道低的現象可能與亞洲人種及就診延遲有關。大量研究發現,CEBPA雙突變是AML患者獨立的預后良好因素[20,22-23]。本研究中,試驗組5年OS達到57.33%,明顯高于對照組的30.99%。由此可見,CEBPA雙突變對AML患者CR率影響不大,但對OS影響明顯。進一步對試驗組的預后相關危險因素進行分析,提示在CEBPA雙突變AML患者中,年齡≥60歲、初診HGB<88.75 g/L及不良染色體核型是預后的獨立危險因素。研究顯示,年齡≥60歲[31]、不良染色體核型[32]均是AML患者預后獨立危險因素。
綜上所述,伴CEBPA雙突變AML患者有較低的早期死亡率,預后明顯較非CEBPA雙突變AML患者好。對于年齡≥60歲、初診HGB<88.75 g/L及不良染色體核型的伴CEBPA雙突變AML患者,應制定個體化的治療以提高患者的長期生存率。
[參考文獻]
[1] Arber DA.Acute myeloid leukemia[J]. Atlas of Bone Marrow Pathology,2018,5:173-191.
[2] Godwin CD,Gale RP,Walter RB,et al. Gemtuzumab ozogamicin in acute myeloid leukemia[J]. Leukemia,2017, 31(9):1855-1868.
[3] Sayar H,Bashardoust P. Therapies for acute myeloid leukemia:Vosaroxin[J]. Onco Targets Ther,2017,10:3957-3963.
[4] 楊懿春,石林,王建渝,等.含地西他濱方案治療老年急性髓系白血病26例療效分析[J]. 臨床血液學雜志,2018,31(5):373-378.
[5] 李珊,楊麗葭,趙慧,等.初診老年急性髓系白血病淋巴細胞亞群分布特點及其與預后的相關性[J].臨床血液學雜志,2018,31(7):523-527.
[6] 金潔.急性髓系白血病靶向治療[J].臨床血液學雜志,2018,31(3):178-180.
[7] Amy B,Matthew M,Aruna R,et al.Acute myeloid leukemia characterized by four CEBPA mutations[J]. American Journal of Clinical Pathology,2018,150(1): 103-104.
[8] Tawana K,Rio-Machin A,Preudhomme C,et al.Familial CEBPA-mutated acute myeloid leukemia[J]. Seminars in Hematology,2017,54(2):87-93.
[9] Su L,Tan YH,Lin H,et al. Mutational spectrum of acute myeloid leukemia patients with double CEBPA mutations based on next-generation sequencing and its prognostic significance[J]. Oncotarget,2018,38:24 970-24 979.
[10] Vinhas R,Tolmatcheva A,Canto ?R,et al. A novel mutation in CEBPA gene in a patient with acute myeloid leukemia[J].Leukemia & Lymphoma,2016,57(3):711-713.
[11] Yang Z,Fang W,Xue C,et al. CSF3R Mutations are frequently associated with abnormalities of RUNX1,CBFB,CEBPA,and NPM1 genes in acute myeloid leukemia[J]. Cancer,2018,124(16):3329-3338.
[12] Ryan SR. Acute myeloid leukemia with recurrent genetic abnormalities, part Ⅱ:Mutations involving CEBPA,NPM1,and RUNX1[J].Precision Molecular Pathology of Myeloid Neoplasms,2017(12):27-46.
[13] 張艷,張蘇江,仇紅霞,等.急性髓系白血病CEBPA基因突變研究[J].中國實驗血液學雜志,2010,18(4):859-862.
[14] 阮國瑞,牛繼紅,李玲娣,等. NDA片段長度分析檢測急性髓性白血病CEBPA基因突變[J].中華臨床醫師雜志(電子版),2011,5(1):640-669.
[15] 張之南.血液病診斷及療效標準[M].北京:科學出版社,1998:171-183.
[16] Shen Y,Zhu YM,Fan X,et al. Gene mutation patterns and their prognostic impact in a cohort of 1185 patients with acute myeloid leukemia[J].Blood,2011,118(20):5593-5603.
[17] 吳繼穎,范進婷,趙芳,等.急性髓系白血病 CEBPA 基因突變與臨床特點的關系[J].臨床醫藥實踐,2015,24(12):899-902.
[18] El-Sharkawi D,Sproul D,Allen CG,et al. Variable outcome and methylation status according to CEBPA mutant type in double-mutated acute myeloid leukemia patients and the possible implications for treatment[J].Haematologica,2018, 103(1):91-100.
[19] Ahn J,Kim JY,Kim HJ,et al. Normal karyotype acute myeloid leukemia patients with CEBPA double mutation have a favorable prognosis but no survival benefit from allogeneic stem cell transplant[J]. Annals of Hematology,2016,95(2):301-310.
[20] Green CL,Koo KK,Hills RK,et al. Prognostic significance of CEBPA mutations in a large cohort of younger adult patients with acute myeloid leukemia:Impact of double CEBPA mutations and the interaction with FLT3 and NPM1 mutations[J]. J Clin Oncol,2010,28(16):2739-2747.
[21] Taskesen E,Bullinger L,Corbacioglu A,et al. Prognostic impact, concurrent genetic mutations, and gene expression features of AML with CEBPA mutations in a cohort of 1182 cytogenetically normal AML patients:Further evidence for CEBPA double mutant AML as a distinctive disease entity[J].Blood,2011,117(8):2469-2475.
[22] Fasan A,Haferlach C,Alpermann T,et al. The role of different genetic subtypes of CEBPA mutated AML[J]. Leukemia,2014,28(4):794-803.
[23] Lin LI,Chen CY,Lin DT,et al. Characterization of CEBPA mutations in acute myeloid leukemia:Most patients with CEBPA mutations have biallelic mutations and show a distinct immunophenotype of the leukemic cells[J]. Clin Cancer Res, 2005,11(4):1372-1379.
[24] R?觟hrs S,Scherr M,Romani J,et al. CD7 in acute myeloid leukemia:Correlation with loss of wild-type CEBPA,consequence of epigenetic regulation[J]. J Hematol Oncol,2010(3):15.
[25] Yamamoto K,Yakushijin K,Ichikawa H,et al. Expression of a novel ZMYND11/MBTD1 fusion transcript in CD7+CD56+ acute myeloid leukemia with t(10;17)(p15;q21)[J]. Leukemia & lymphoma,2018(18):1-5.
[26] Xiao SS,Zhu HQ. Correlation study on CD7,CD34, CD56 and HLA-DR expressions and its prognosis among patients with acute myeloid leukemia[J]. Biomedical Research-India,2017,28(15):6786-6790.
[27] Hojilla C,Thomas M,Sukhai M,et al. Genetic heterogeneity,CD7 and CD34 expression identifies a subpopulation of nucleophosmin 1-mutated acute myeloid leukemia (NPM1+AML) with early relapse[J]. Laboratory Investigation,2016(96):352.
[28] Ahn JS,Kim JY,Kim HJ,et al. Erratum to:Normal karyotype acute myeloid leukemia patients with CEBPA double mutation have a favorable prognosis but no survival benefit from allogeneic stem cell transplant[J]. Ann Hematol,2016,95(2):363.
[29] Jehan AE,Laila MS,Atef MT,et al. Prognostic significance of CEBPA mutations and BAALC expression in acute myeloid leukemia patients with normal karyotype[J].European Journal of General Medicine,2015,7(1):17-28.
[30] Renneville A,Boissel N,Gachard N,et al. The favorable impact of CEBPA mutations in patients with acute myeloid leukemia is only observed in the absence of associated cytogenetic abnormalities and FLT3 internal duplication[J]. Blood, 2009,113(21):5090-5093.
[31] Zhang QL,Li XY,Wei ZY,et al. Risk factors and clinical characteristics of non-promyelocytic acute myeloid leukemia of intracerebral hemorrhage:A single center study in China[J]. Journal of Clinical Neuroscience,2017(44):203-206.
[32] Shannon RM,Mark JL. Emerging molecular predictive and prognostic factors in acute myeloid leukemia[J]. Leukemia & Lymphoma,2018,9(9):2021-2039.
(收稿日期:2020-06-12)